Acanthosis Nigricans: A Rare Presentation in a Patient with Hypothyroidism and Metabolic Syndrome
Rucha Sawant1, Pranav Chaudhari2, Sourya Acharya3, Roma Chavhan4
1 Resident, Department of General Medicine, Datta Meghe Institute of Higher Education and Research (Deemed to be University), Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
2 Resident, Department of General Medicine, Datta Meghe Institute of Higher Education and Research (Deemed to be University), Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
3 Professor, Department of General Medicine, Datta Meghe Institute of Higher Education and Research (Deemed to be University), Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
4 Resident, Department of General Medicine, Datta Meghe Institute of Higher Education and Research (Deemed to be University), Jawaharlal Nehru Medical College, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Rucha Sawant, Resident, Third Floor, Department of Medicine, Acharya Vinoba Bhave Rural Hospital, Jawaharlal Nehru Medical College, Sawangi (Meghe), Wardha-442001, Maharashtra, India.
E-mail: dr.rucha.medicine28@gmail.com
Hyperkeratotic, Hyperpigmented, Suffusion
A 38-year-old male came to the Medicine Outpatient Department (OPD) with complaints of easy fatigability for four months. He had no other significant history. Upon general examination, his Body Mass Index (BMI) was 33.2 kg/m2, and his waist circumference was 142 cm. The patient was diffusely hyperpigmented; upon examining his neck region, a dark, velvety hyperkeratotic plaque suggested Acanthosis Nigricans (AN) [Table/Fig-1].
Shows hyperpigmented, hyperkeratotic plaque over the neck region.
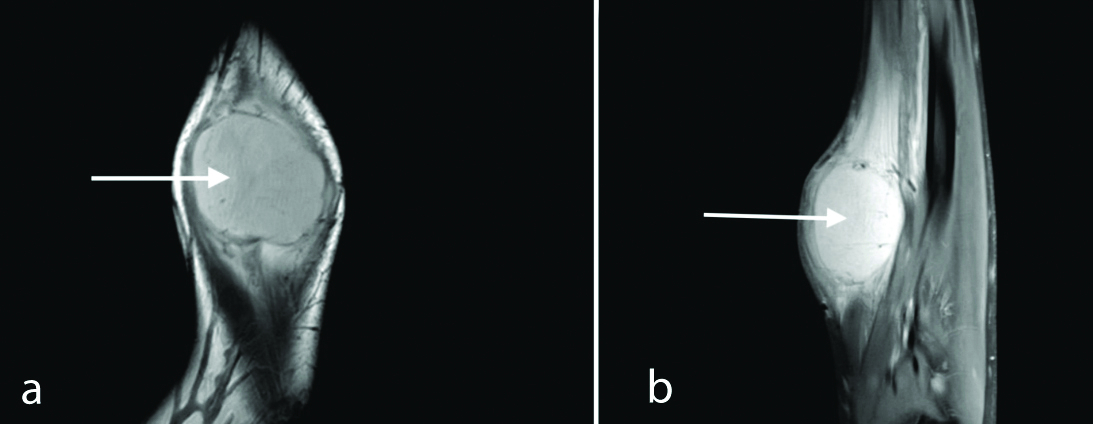
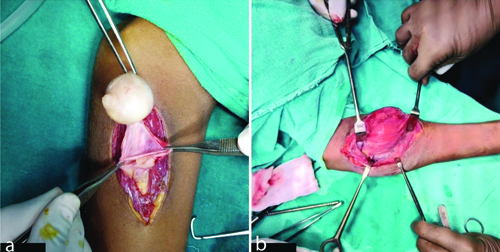
His axillary region showed similar pigmentation [Table/Fig-2a,b]. Upon further examination, the patient also had facial suffusion, hoarseness of voice, coarse skin and brittle hair [Table/Fig-3].
a,b) Shows hyperpigmented, hyperkeratotic plaque in the left and the right axillary region, respectively.
Top red arrow showing coarse brittle hair. Middle and bottom red arrows showing thick, dry and coarse skin.

Upon examination, his blood pressure was 138/92 mmHg. On neurological examination, he displayed delayed relaxation of the ankle reflex [Video-1]. His cardiovascular, respiratory, and abdominal examinations were within normal limits.
When the case was further investigated, his lipid profile was deranged, with increased triglycerides at 288 mg/dL (<150 mg/dL) and decreased High-density Lipid (HDL) at 30 mg/dL (>40 mg/dL). His fasting and postprandial blood sugars were within the normal range, ruling out diabetes mellitus as a contributing factor for AN. He was diagnosed with Metabolic Syndrome (MS) based on the National Cholesterol Education Program (NCEP) - Adult Treatment Panel (ATP) III criteria [1].
His thyroid profile showed an elevated Thyroid stimulating Hormone (TSH) of 78 μIU/mL (0.4-4.68 μIU/mL), with free T3 at 1.7 pg/mL (2.76-5.26 pg/mL) and free T4 at 0.2 ng/mL (0.77-2.18 ng/mL), suggestive of overt hypothyroidism. The patient was started on levothyroxine 100 mcg once a day, advised dietary and lifestyle modifications, and instructed to follow-up in a month.
Despite a lack of significant change in BMI (32.9 kg/m2), after one month, the patient experienced positive results from treatment. His fatigue levels became minimal, and thyroid function tests demonstrated improvement, with TSH reaching 60 μIU/mL (0.4-4.68 μIU/mL), free T3 reaching 2.6 pg/mL (2.76-5.26 pg/mL), and free T4 reaching 1 ng/mL (0.77-2.18 ng/mL). These findings suggest the need for continued monitoring and potential treatment adjustments for optimal outcomes.
Discussion
The presence of AN is characterised by dark, hyperpigmented, velvety-textured skin with hyperkeratosis. This condition is generally observed in skin folds, such as the neck and axillary areas. Other common sites for AN include the groin, umbilicus, popliteal region, and antecubital area. These locations often experience frequent friction, which contributes to hyperkeratosis. The female-to-male ratio is approximately 3:2 [2].
Causative factors for AN can be categorised as paraneoplastic or non paraneoplastic. The paraneoplastic association is typically linked to adenocarcinomas of gastroenterological or genitourinary origin. Other rarer paraneoplastic causes include thyroid cancer, lung cancer, and lymphomas [3]. Non paraneoplastic causes include diabetes mellitus, metabolic conditions like obesity, and familial AN. Rarely, AN can also be drug-induced due to medications such as nicotinic acid, insulin, systemic steroids, and oral contraceptive pills. Additionally, AN can be mixed, featuring more than one causative factor.
Patients with AN are at increased susceptibility to develop MS, which comprises obesity, hypertension, elevated triglycerides, low HDL and impaired glucose tolerance [2]. A study conducted by Puri N establishes a crucial association between AN and malignancy. However, recognising its stronger association with obesity and insulin resistance provides a valuable opportunity for the early detection of related diseases, such as type 2 diabetes and MS [2]. Puri N further observes a connection between obesity and several conditions, noting that it is associated with insulin resistance, hyperinsulinemia, and AN [2]. Addressing hyperinsulinemia often leads to improvements in hyperkeratotic lesions of AN, highlighting the potential link between insulin levels and these skin conditions. Thyroid dysfunction is observed in approximately 13.3% of patients with AN [2].
The relationship between TSH and obesity is well-established. TSH is generally elevated in obese individuals because leptin causes the upregulation of Thyrotropin-releasing Hormone (TRH). Increased levels of leptin lead to elevated TSH by activating the pituitary-thyroid axis. A 33% drop in BMI after weight reduction made all these changes reversible. The results show that obesity can cause Thyroid Hormone (TH) resistance and that adipocytes play a crucial role in regulating THs. The relationship between leptin levels and Autoimmune Thyroid Disease (AITD) has been studied in obese individuals in several research studies, which reveal that Thyroid Peroxidase Antibodies (TPOAb) are more common in obese patients and that leptin levels might be connected with Hashimoto’s thyroiditis [4].
Imbalances in glucose homeostasis (adverse glucose metabolism) can be observed in hyperthyroidism. However, these disruptions can also extend to hypothyroidism, elevated serum TSH concentrations, and dyslipidemia characterised by abnormal serum triglyceride levels [5]. Research suggests a link between abnormal thyroid function, including both hypothyroidism and hyperthyroidism, and high blood pressure. This association may be due to how thyroid hormones (THs) influence the heart’s blood vessels, potentially through genetic factors or non genomic effects [5].
The THs and their metabolites play a multifaceted role in regulating adiposity. This influence extends beyond metabolic rate to include appetite control and sympathetic activity [5]. Notably, sympathetic stimulation by THs impacts cardiovascular function as well as glucose and lipid metabolism, further contributing to the regulation of adiposity [5]. THs regulate lipid metabolism by stimulating both synthesis and degradation, which may contribute to the observed association between dyslipidemia and thyroid dysfunction [5]. In addition to their well known effects on lipid metabolism, THs are crucial in regulating the body’s ability to secrete and degrade insulin [5].
Research by Brenta G et al., suggests a link between low thyroid function and MS [6]. Since, AN is often associated with MS, this finding compels physicians to investigate both conditions if one is already present in a patient. There have been reports suggesting that AN can be treated by addressing the underlying causative factors, which in present case are MS and hypothyroidism. AN is generally a cosmetic issue and can be locally treated with keratolytics such as topical tretinoin 0.05% and ammonium lactate 12% cream [2].
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Mar 18, 2024
Manual Googling: Jun 08, 2024
iThenticate Software: Jun 11, 2024 (6%)
[1]. Rezaianzadeh A, Namayandeh SM, Sadr SM, National cholesterol education program adult treatment panel III versus international diabetic federation definition of metabolic syndrome, which one is associated with diabetes mellitus and coronary artery disease?Int J Prev Med 2012 3(8):552-58.22973485PMC3429802 [Google Scholar] [PubMed]
[2]. Puri N, A study of the pathogenesis of Acanthosis nigricans and its clinical implicationsIndian J Dermatol 2011 56:67810.4103/0019-5154.9182822345770PMC3276896 [Google Scholar] [CrossRef] [PubMed]
[3]. Popa ML, Popa A, Tanase C, Gheorghisan-Galateanu AA, Acanthosis nigricans: To be or not to be afraid (Review)Oncol Lett 2019 17(5):4133-38.Published Online First: 19 November 201810.3892/ol.2018.973630944606PMC6444334 [Google Scholar] [CrossRef] [PubMed]
[4]. Biondi B, Subclinical hypothyroidism in patients with obesity and metabolic syndrome: A narrative reviewNutrients 2023 16:8710.3390/nu1601008738201918PMC10780356 [Google Scholar] [CrossRef] [PubMed]
[5]. Teixeira PDFDS, Dos Santos PB, Pazos-Moura CC, The role of thyroid hormone in metabolism and metabolic syndromeTherapeutic Advances in Endocrinology 2020 11:20420188209178610.1177/204201882091786932489580PMC7238803 [Google Scholar] [CrossRef] [PubMed]
[6]. Brenta G, Caballero AS, Te Nunes M, Case finding for hypothyroidism should include type 2 diabetes and metabolic syndrome patients: A Latin American Thyroid Society (LATS) position statementEndocrine Practice 2019 25:101-05.10.4158/EP-2018-031730742573 [Google Scholar] [CrossRef] [PubMed]