Introduction
An Odontogenic Keratocyst (OKC) is always a topic of debate due to its distinct biological behaviour to recur after surgical procedure. Also, it has an odyssey cyst-tumour-cyst from 1956 to 2005 to 2017. For this reason, number of treatment modalities was cited in the literature. Modified Carnoy’s Solution (MCS) is commonly used due to its effectiveness, while 5FU, an antimetabolite used in cancer treatment, presents a newer approach.
Need of the study
The varying Recurrence Rate (RR) and postoperative complications associated with different treatment modalities for OKC. While MCS is a commonly used adjuvant therapy due to its effectiveness, and bone resection minimises recurrence but leads to severe functional and aesthetic issues, there is limited data comparing the efficacy of MCS to newer agents like 5-Fluorouracil (5FU) in reducing recurrence. Evaluating the effectiveness of 5FU, a promising chemotherapeutic agent, could potentially offer a less invasive and equally effective treatment option for reducing recurrence and improving patient outcomes in OKC management.
Aim
To compare and evaluate the postoperative outcomes, specifically the RR, of MCS vs 5FU used for chemical cauterisation following enucleation and peripheral ostectomy in patients with OKC.
Materials and Methods
An experimental in-vivo study will be conducted in the Department of Oral and Maxillofacial Surgery, Sharad Pawar Dental College, Datta Meghe Institute of Higher Education and Research (DMIHER), Sawangi (M), Wardha, Maharashtra, India, from April 2023 to March 2024. The approach involves categorising 12 histologically proven cases of OKC into two groups according to distinct adjunct techniques used (six patients in each group). Group A includes subjects treated with MCS. Group B includes subjects with 5FU. Postoperative outcomes will be evaluated and compared among the groups. The data will be analysed and compared using Student’s t-test and Mann-Whitney U test. It will be used at a 5% level of significance (p-value ≤0.05).
Introduction
Philipson in 1956 defined the term OKC as, a developmental cyst derived from remnants of dental lamina or enamel organ [1]. It is an entity with controversial nature. This is because of its potential aggressive pattern of growth and lofty recurrence after treatment procedure (13-80%) [2]. Moreover, the mutations found in Patched (PTCH), Cyclin-dependent Kinase Inhibitor 2a (CDKN2A), Tumour Protein p53 (TP53), Mutated in Colorectal Cancer (MCC), Cellular Adhesion Molecule 1 (CADMI), and Fragile Histidine Triad (FHIT) gene World Health Organisation (WHO) in 2005 classified it under benign neoplasm as ‘Keratocystic Odontogenic Tumour (KCOT)’ Interestingly the WHO panel was unable to reproduce the molecular evidence to prove against the neoplastic nature of the KCOT, they reclassified it again as OKC in 2017 [3].
The OKCs primarily occur in the posterior mandible and ascending ramus, though they can develop in any region of the jaws [4]. Radiographically, OKCs appear as unilocular or multilocular radiolucencies with distinct sclerotic margins and are often associated with unerupted teeth. The cysts typically expand in an anteroposterior direction, resulting in minimal cortical bone expansion, and root resorption of adjacent teeth is uncommon. Odontogenic cysts are often asymptomatic and may go undiagnosed until they become infected or aggressive, leading to bone resorption and large bony defects. Diagnosis is confirmed through clinical, radiological and aspiratory findings, with histopathological analysis of the cystic lining serving as the gold standard [5].
Down the years, there has been ample surgical treatment modalities introduced, practiced, published and recognised in the literature. It categorised as: a) conservative- decompression, marsupilisation enucleation with or without curettage; b) radical- peripheral ostectomy and aggressive resection; c) with or without adjuvant treatment like chemical cauterisation, cryotherpy and electrocautery [6].
As there is lack of said treatment protocol, the selection of these modalities solely depends upon the surgeon’s clinical judgment and expertise. Hence, the goal of treatment must be complete abolition of cyst, to prevent recurrence along with minimal morbidity by preserving the continuity of the mandible and function of the nerve, wherever possible.
The Carnoy’s Solution (CS) as an adjuvant used after enucleation and peripheral ostectomy reduces the risk of recurrence. But with its carcinogenic content chloroform is removed and MCS is being used instead. In a study by Ecker J et al., showed that, there is markedly high RR with modified CS than original CS [7]. Ledderhof NJ et al., proposed that cystic cavity managed with 5FU proved to have a reduced instance of recurrence [8]. Lone PA et al., studied 27 patients with OKCs and observed that treatment with 5FU resulted in minimal complications, no recurrence and good preservation of aesthetics, whereas MCS had a RR of 66.6% [9]. The 5FU, an antimetabolite chemotherapy drug, shows potential as an adjuvant therapy in OKC management by inhibiting residual epithelial cells and promoting fibrosis, thereby reducing recurrence [8]. Similarly, Caldas RD et al., described a case where 5FU, following marsupialisation of an OKC, led to significant bone regeneration without recurrence after four months. These findings indicate that 5FU may be a viable, low-morbidity option for OKC management [10].
Hence, the present study will be hypothesised to find out the most suitable material used for chemical cauterisation following enucleation and peripheral ostectomy with respect to better postoperative outcome and minimal RR in patients with OKC.
Objectives
To evaluate the postoperative outcomes of MCS for chemical cauterisation following enucleation and peripheral ostectomy in patients with odontogenic cyst;
To evaluate the postoperative outcomes of 5-Flurouracial for chemical cauterisation following enucleation and peripheral ostectomy in patients with odontogenic cyst
To compare and evaluate the postoperative outcomes of MCS vs 5-Flurouracial used for chemical cauterisation following enucleation and peripheral ostectomy in patients with odontogenic cyst.
Null hypothesis: No significant difference will be observed in the rate of recurrence of OKC among the 5FU group and MCS group as a chemical adjunct used for the treatment of OKC.
Alternate hypothesis: A significant difference will be observed in reducing the rate of recurrence of OKC while using 5- FU as chemical cauterising agent after enucleation and peripheral ostectomy of OKC over MCS.
Review of Literature
Nayak MT et al., highlighted the complexity of classifying odontogenic cysts, leading to confusion for clinicians and pathologists. The OKC stands out due to its distinctive histopathological and clinical features, aggressive behavior and high RR. Despite various classifications, managing this common jaw lesion remains challenging for clinicians [11].
Wright JM and Vered M, summarised updates in the 4th edition of the WHO classification of head and neck tumours, published in January 2017. This edition reinstated odontogenic cysts, previously excluded in the 3rd edition (2005), and included other unique jaw conditions. Numerous new tumours identified since 2005 were also added. Despite the consensus that neoplasms do not spontaneously regress, OKCs have been documented to fully regress after decompression, with the lining of decompressed cysts often resembling oral mucosa rather than the typical OKC histology [3].
Al-Moraissi EA et al., conducted a comprehensive systematic review and meta-analysis involving 2,287 cases of OKCs across 35 studies. They reported weighted RR for various treatments: enucleation alone (23.1%), enucleation with curettage (17.4%), enucleation with CS (11.5%), enucleation with liquid nitrogen cryotherapy (14.5%), marsupialisation alone (32.3%), decompression followed by residual cystectomy (14.6%) and resection (8.4%). The pooled weighted overall RR for all treatments was 16.6%. The study concluded that while radical resection achieves the lowest RRs, enucleation combined with CS could be considered a primary treatment option for OKCs due to its effectiveness in reducing recurrence [12].
Donnelly LA et al., conducted a retrospective cohort study on 77 patients with OKCs treated with Enucleation and Curettage (EC), peripheral ostectomy, and either CS or MCS. They found similar RRs (14.29%) and median time to recurrence (24 months) between the CS (13.9% recurrence) and MC (14.6% recurrence) groups. Preserving adjacent teeth was associated with significantly higher RRs (p-value=0.0036). The study concluded no significant difference in RRs or time to recurrence between OKCs treated with CS or MC [13].
Wanve SA et al., conducted a study on 42 cases of OKCs treated with enucleation, followed by MCS or 5FU as adjunct therapies. The outcomes, including pain, swelling, paresthesia, bone sequestrum formation, osteomyelitis and RRs, were evaluated over 12 months. The study found no significant differences in pain or swelling between groups; however, permanent paresthesia and recurrence were slightly higher in the MCS group, without reaching statistical significance. The authors concluded that 5FU is a feasible, biocompatible and cost-effective alternative to MCS, effectively minimising recurrence and morbidity. Given the limited literature comparing these adjuvants, the present study aimed to further validate the use of 5FU as a preferable, less invasive option due to its availability, ease of application and reduced morbidity compared to MCS [14].
Materials and Methods
An experimental in-vivo study will be conducted in the Department of Oral and Maxillofacial Surgery, Sharad Pawar Dental College, DMIHER, Sawangi (M), Wardha, Maharashtra, India, from April 2023 to March 2024. Ethical clearance for the research methodology has been granted by the Institutional Ethics Committee (IEC) of the study Institute {DMIHER (DU)/IEC/2023/845, dated March 2023}.
Inclusion criteria:
Histologically proven cases of OKC with the age range of 18-70 years;
Patients having cystic lesion of size ≥2 cm in greatest dimension;
Patient having interincisal mouth opening of at least 30 mm;
Patient who shall be non-smoker and non-alcoholic.
Exclusion criteria:
Patients having cystic lesion of size <2 cm in diameter;
All patients who have multiple cystic lesions;
All previously treated patient with same diagnosis of OKC;
Patients with immunocompromised status;
Pregnant and lactating females.
Sample size calculation: The formula to be used for sample size calculation is as follows:
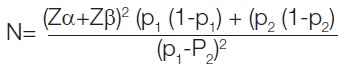
Zα=1.64
alpha= Type I error at 5%
Zβ=0.84
beta=Type II error at 20%
Reccurance rate of OKC while treatment with MCS=66.6%
Recurrance rate of OKC while treatment with 5-flurouracial=0%
Difference (p2-p1)=66.6%
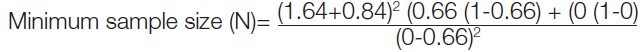
=6
6 Each in 2 groups
Sample size= 12. (Lone PA et al., 2020) [9].
Intervention
Twelve patients fitting in to the criteria of the study will undergo the procedure of assessment and surgery. History will be taken and the pretreatment clinical condition of the patient will be assessed based on the clinical and radiological data and records will be maintained for the evaluation of parameters (RR). All the patients willing to be taken for surgery after presurgical work-up which shall include: Preanaesthetic Check-up (PAC) fitness, thoroughly explained, written and signed consents, patient’s preparation, preoperative photographs.
Patient will be then divided randomly into two groups for both groups intraoral incision will be given according to the site of the lesion. After infiltration with saline and adrenaline solution, crevicular incision will be given and full thickness mucoperiosteal flap will be reflected and bony window will be created. Enucleation, curettage of cystic lesion and peripheral ostectomy will be performed.
Group A: Treatment with Modified Carnoy’s Solution (MCS): Immediately after enucleation and peripheral ostectomy intraoperatively, cavity will be covered with modified Carnoy solution (60% ethanol, and 10% glacial acetic acid, 1 g of ferric chloride) for 3 min, followed by thorough irrigation with normal saline. To preserve nerve- Vaseline gauze will be applied.
Group B: Treatment with 5-Flurouracil (5FU): Immediately after enucleation and peripheral ostectomy, sterile ribbon gauze will be coated with 5FU (500 mg ampule) 10 mL and packed into the surgical cavity. Wound will be closed in usual manner leaving a small end exposed into oral cavity, and removed after 24 hours postoperatively.
Followed by primary closure with the help of 3-0 vicryl. All the surgical procedure performed by senior surgeon, having a considerable experience in head and neck surgery. Patient will be kept on regular follow-up where clinical and radiological evaluation {Cone Beam Computed Tomography (CBCT)} will be done in an interval of seven days, three months and six months. The scoring criteria for the clinical findings has been presented in [Table/Fig-1].
Landry’s (1988) healing scale [15].
| Score | Clinical findings | Scoring criteria |
|---|
| 1 | Very poor healing (with presence of 2 or more signs) | ≥50% of gingiva red.
Response to palpation: bleeding
Granulation tissue: present
Incision margin: Not epithelialised, with loss of epithelium beyond incision margin suppuration present. |
| 2 | Poor healing | >50% of gingiva red
Response to palpation: bleeding
Granulation tissue: present
Incision margin: Not epithelialised, with connective tissue exposed. |
| 3 | Good healing | Tissue colour: 25-50% and of gingiva red
Response to palpation: No bleeding
Granulation tissue: None
Incision margin: No connective tissue exposed. |
| 4 | Very good healing | Very good tissue colour: <25% of gingiva red
Response to palpation: No bleeding
Granulation tissue: None
Incision margin: No connective tissue exposed. |
| 5 | Excellent healing | Excellent tissue colour: All tissues pink
Response to palpation: No bleeding
Granulation tissue: None
Incision margin: No connective tissue exposed. |
Outcomes
Soft-tissue healing measurement:
Soft-tissue assessment: Clinical appearance of the soft-tissues will be assessed postoperatively after one week using a Landry’s (1988) healing scale [Table/Fig-1] [15].
Radiographic assessment: CBCT
Clinical and radiological parameter evaluation: An independent observer will evaluate the patient on the basis of the following parameters:
Assessment of bone formation: Radiographic assessment of bone formation will be assessed on, 3rd and 6th months follow-up using CBCT in axial, coronal and saggital view. All the scans shall be obtained from Oral Radiology Department of the study Institute using Carestream machine [16].
Rate of recurrence: Clinical and radiological assessment will be done on 3rd and 6th month of follow-up using clinical evaluation (pain, tenderness, oedema, bleeding and pus discharge) and CBCT [17]. (Any above-mentioned signs and symptoms shall be considered for probability of recurrence of disease).
Dissemination: The result of the present study will provide level I evidence of which material is superior for chemical cauterisation in form of postoperative outcomes for minimal RR used for chemical cauterisation following enucleation and peripheral ostectomy in patients with OKC.
Statistical Analysis
Statistical analysis shall be done by using descriptive and inferential statistics using Student’s t-test and Mann-Whiney U test. The software shall use in the analysis will be Statistical Package for the Social Sciences (SPSS) software version 27.0 and GraphPad Prism 7.0 version and p-value ≤0.05 will consider as level of significance. This shall be according to the study performed by Lone PA et al., 2020 [9].
[1]. Pogrel MA, The keratocystic odontogenic tumour (KCOT)- An odysseyInt J Oral Maxillofac Surg 2015 44(12):1565-68.10.1016/j.ijom.2015.03.00826003518 [Google Scholar] [CrossRef] [PubMed]
[2]. Stoelinga PJW, Bronkhorst FB, The incidence, multiple presentation and recurrence of aggressive cysts of the jawsJ Craniomaxillofac Surg 1988 16(4):184-95.10.1016/S1010-5182(88)80044-13290262 [Google Scholar] [CrossRef] [PubMed]
[3]. Wright JM, Vered M, Update from the 4th edition of the World Health Organization Classification of head and neck tumours: Odontogenic and maxillofacial bone tumorsHead Neck Pathol 2017 11(1):68-77.10.1007/s12105-017-0794-128247226PMC5340735 [Google Scholar] [CrossRef] [PubMed]
[4]. Pitak-Arnnop P, Chaine A, Oprean N, Dhanuthai K, Bertrand JC, Bertolus C, Management of odontogenic keratocysts of the jaws: A ten-year experience with 120 consecutive lesionsJ Craniomaxillofac Surg 2010 38(5):358-64.10.1016/j.jcms.2009.10.00619897381 [Google Scholar] [CrossRef] [PubMed]
[5]. Borghesi A, Nardi C, Giannitto C, Tironi A, Maroldi R, Di Bartolomeo F, Odontogenic keratocyst: Imaging features of a benign lesion with an aggressive behaviourInsights Imaging 2018 9(5):883-97.10.1007/s13244-018-0644-z30066143PMC6206371 [Google Scholar] [CrossRef] [PubMed]
[6]. Feudis FD, Girotto R, Balercia A, Togni L, Rubini C, Balercia P, Management of the odontogenic keratocysts from diagnosis to treatment: An algorithm derived from the comparison of a single institution experience and literature reviewJ Oral Maxillofac Surg Med Pathol 2023 35(5):410-15.10.1016/j.ajoms.2023.02.004 [Google Scholar] [CrossRef]
[7]. Ecker J, Horst RT, Koslovsky D, Current role of Carnoy’s Solution in treating keratocystic odontogenic tumorsJ Oral Maxillofac Surg 2016 74(2):278-82.10.1016/j.joms.2015.07.01826272006 [Google Scholar] [CrossRef] [PubMed]
[8]. Ledderhof NJ, Caminiti MF, Bradley G, Lam DK, Topical 5-Fluorouracil is a novel targeted therapy for the keratocystic odontogenic tumorJ Oral Maxillofac Surg 2017 75(3):514-24.10.1016/j.joms.2016.09.03927789270 [Google Scholar] [CrossRef] [PubMed]
[9]. Lone PA, Wani NA, Janbaz ZA, Bibi M, Kour A, Topical 5-fluorouracil application in management of odontogenic keratocystsJ Oral Biol Craniofac Res 2020 10(4):404-06.10.1016/j.jobcr.2020.07.00832775182PMC7394907 [Google Scholar] [CrossRef] [PubMed]
[10]. Caldas RD, Barreto JD, Santos CWN, Miceli AL, Freire ND, Abrahão AC, Therapy for odontogenic lesions with 5-fluorouracil topical: A case reportOral Surgery, Oral Surg Oral Med Oral Pathol Oral Radiol 2020 129(1):e9410.1016/j.oooo.2019.06.394 [Google Scholar] [CrossRef]
[11]. Nayak MT, Singh A, Singhvi A, Sharma R, Odontogenic keratocyst: What is in the name?J Nat Sci Biol Med 2013 4:282-85.10.4103/0976-9668.11696824082717PMC3783765 [Google Scholar] [CrossRef] [PubMed]
[12]. Al-Moraissi EA, Pogrel MA, Ellis E, Does the excision of overlying oral mucosa reduce the recurrence rate in the treatment of the keratocystic odontogenic tumor? A systematic review and meta-analysisJ Oral Maxillofac Surg 2016 74(10):1974-82.10.1016/j.joms.2016.03.04327134155 [Google Scholar] [CrossRef] [PubMed]
[13]. Donnelly LA, Simmons TH, Blitstein BJ, Pham MH, Saha PT, Phillips C, Modified carnoy’s compared to carnoy’s solution is equally effective in preventing recurrence of odontogenic keratocystsJ Oral Maxillofac Surg 2021 79(9):1874-81.10.1016/j.joms.2021.03.01033901451 [Google Scholar] [CrossRef] [PubMed]
[14]. Wanve SA, Andrade NN, Venkatakrishnan L, Desai H, Comparison of the effectiveness of 5-fluorouracil and modified carnoy’s solution in reducing the recurrence of odontogenic keratocystJ Oral Biol Craniofac Res 2023 13:436-41.10.1016/j.jobcr.2023.03.00737207018PMC10189504 [Google Scholar] [CrossRef] [PubMed]
[15]. Rodriguez AB, Alhachache S, Velasquez D, Chan HL, A systematic review of oral wound healing indicesPLoS One 2024 19(2):e029005010.1371/journal.pone.029005038330054PMC10852230 [Google Scholar] [CrossRef] [PubMed]
[16]. La Rosa GRM, Priolo CY, Abiad RS, Romeo VR, Ambu E, Pedullà E, Assessment of bone regeneration after maxillary radicular cyst enucleation with or without bone grafting materials: A retrospective cohort studyClin Oral Investig 2024 28(4):21310.1007/s00784-024-05612-738480533PMC10937747 [Google Scholar] [CrossRef] [PubMed]
[17]. Fidele NB, Yueyu Z, Zhao Y, Tianfu W, Liu J, Sun Y, Recurrence of odontogenic keratocysts and possible prognostic factors: Review of 455 patientsMed Oral Patol Oral Cir Bucal 2019 24(4):e491-e501.10.4317/medoral.2282731232383PMC6667002 [Google Scholar] [CrossRef] [PubMed]