Neurofibromatoses are a group of genetic disorders that cause tumours to form on the nerve tissue. These tumours can progress to more proliferative lesions and can also eventually become malignant, giving rise to a Malignant Peripheral Nerve Sheath Tumour (MPNST). The authors describe a rare case involving a 27-year-old female who presented with swelling on the left forearm in the surgery Outpatient Department (OPD). The swelling measured 6×5 cm and was noted on the left upper forearm. The overlying skin appeared normal, with no evident pulsations. Notably, a scar mark indicative of a previous surgery for a similar swelling was observed at the same site. The patient reported that the previous swelling was operated 2 years ago. Magnetic Resonance Imaging (MRI) findings indicated fusiform swelling in the mid-forearm, possibly originating from the ulnar nerve with significant involvement of the adjacent structures. This case underscores the complexity and diagnostic challenges associated with such swellings, necessitating thorough examination and ongoing monitoring for timely intervention. This case highlights the importance of thorough clinical evaluation, histopathological examination, and molecular analysis in accurately characterising such tumours, guiding clinical management decisions, and ensuring optimal patient outcomes. The diagnostic evaluation and analysis of such swellings contribute invaluable information regarding their proliferation rate and propensity for malignant progression. This comprehensive understanding aids clinicians in tailoring management approaches that prioritise minimal invasiveness while effectively addressing the potential for malignancy, thus optimising patient care.
Forearm, Malignant peripheral nerve sheath tumour, Neurofibromatosis, Schwannoma, Swelling
Case Report
A 27-year-old female presented to the surgery Outpatient Department (OPD) of the authors’ hospital with swelling over her left forearm, which was there for seven months. The swelling over her left forearm was insidious in onset and gradually progressive in nature with no aggravating or relieving factors. Seven months ago, the patient underwent an excision of schwannoma of the left forearm from the same site. There was no history of similar swelling anywhere else on the body, and she did not complain of any restriction in the movement.
Swellings present in association with neural tissue can have the differential diagnosis of recurrent schwannoma associated with the neural tissue, neurofibroma, Malignant Peripheral Nerve Sheath Tumour (MPNST), plexiform neurofibroma, metastatic melanoma, pigmented neurofibroma, and Atypical Neurofibromatous Neoplasm of Uncertain Biologic Potential (ANNUBP).
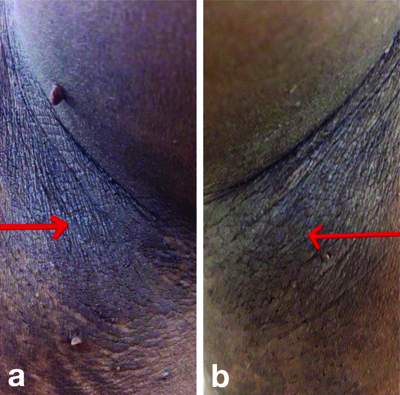
Contrast-enhanced Magnetic Resonance Imaging (CEMRI) of left forearm [Table/Fig-1a,b] stated that in this operated case of left forearm schwannoma, there is evidence of a well-defined fusiform homogeneously enhancing altered signal intensity mass lesion in the medial aspect in the intramuscular plane measuring approximately 4.9×4.7×4.1 cm in size which appears iso to hypointense on T1 Weighted Imaging (T1WI), heterogeneously hyperintense on T2 Weighted Imaging (T2WI)/Short Tau Inversion Recovery (STIR) and showing peripheral blooming on Gradient Recalled Echo (GRE) with surrounding soft-tissue involvement. The lesion was in close proximity to the ulnar, median, and anterior interosseous nerve, compressing the ulnar and radial vein, displacing the ulnar and radial artery and causing compression of flexor digitorum profundus, flexor digitorum superficialis, palmaris longus, flexor carpi radialis, pronator teres, brachioradialis, extensor carpi radialis longus and extensor carpi radialis brevis. The radius and ulna were normal in contour and signal intensity.
Contrast-enhanced Magnetic Resonance Imaging (CEMRI) of the left forearm showing a hyperintense area depicting a fusiform swelling (white arrow).

The CEMRI of left forearm revealed a fusiform swelling in the medial aspect of the left forearm as described, which is suggestive of recurrence of schwannoma, possibly arising from the ulnar nerve.
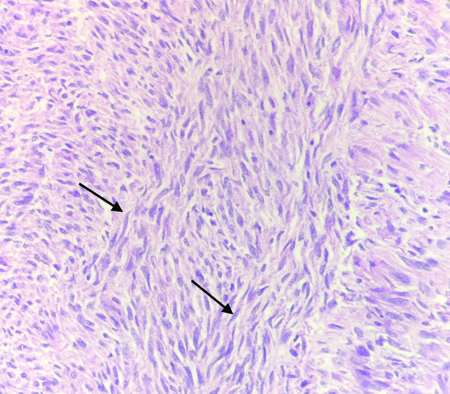
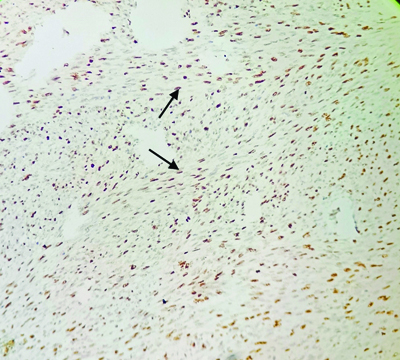
The patient provided informed consent for the surgical resection of the mass. She was thoroughly briefed on the procedure, potential risks, and anticipated outcomes. Additionally, explicit consent was obtained to document the present case. The mass was resected [Table/Fig-2a,b] and sent for histopathological examination. The sample received in the histopathology laboratory was a single, irregular, reddish-white, well-encapsulated tumour measuring 5×5×4 cm [Table/Fig-3]. The Haematoxylin and Eosin (H&E) stained images of the resected swelling revealed nuclear atypia, high cellularity, loss of neurofibroma architecture showing herringbone pattern, and few mitotic activities; there was no necrosis [Table/Fig-4,5]. All these features highly indicated ANNUBP. Immunostaining was also performed, which was highly positive (more than 20% positivity) for Kiel 67 (Ki67) [Table/Fig-6].
Intraoperative pictures of resection of the swelling on left forearm.
Clinical picture of resected specimen (black arrow).

Herringbone pattern (black arrow) depicting the loss of neurofibroma architecture (H&E; 10X).
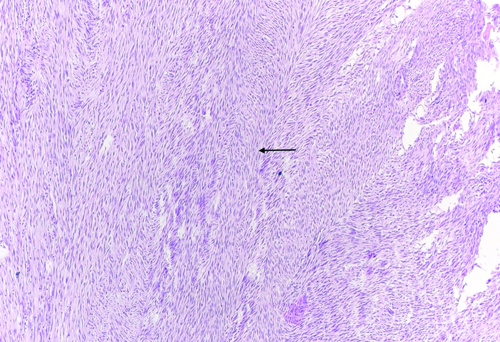
Herringbone pattern (black arrow) depicting the loss of neurofibroma architecture (H&E; 40X).
Immunohistochemistry showing Ki67 highly positive (more than 20% positivity).
Preoperative MRI and H&E stains were highly suggestive of ANNUBP; hence, any aggressive treatment required for MPNST was avoided. At the time of writing, the patient had been scheduled for a follow-up appointment.
Discussion
Neurofibromatoses are a group of genetic disorders that cause tumours to form on the nerve tissue. The Neurofibromatosis 1 (NF1) tumour can progress to MPNST [1]. These are highly aggressive tumours and have a meagre survival rate of 34-52% [2]. Early diagnosis and suitable therapy should, therefore, be demanded. Most NF1 patients have plexiform neurofibroma, which usually affects nearly every nerve. However, growth arrest and rapid tumour growth in adulthood should be considered indicators of malignant change [3]. ANNUBP is recognised as a precursor to MPNST, indicating a condition that has not yet progressed to malignancy but carries the potential for such transformation. The consensus reached by experts in a 2016 meeting established a classification for the progression of ANNUBP to MPNST, delineating categories such as neurofibroma with cytological atypia or hypercellularity, ANNUBP, and MPNST [3].
Miettinen MM et al., in their case report states that the Ki67 labelling index can also be helpful in assessing nerve sheath tumours in NF1 patients highlighting proliferative hot-spots [3]. Similarly, in the present case a marked Ki67 positivity indicated high proliferation rate of the lesion.
It is imperative to differentiate between ANNUBP and MPNST due to the malignant nature of the latter. MPNST is characterised by heightened recurrence rates, increased metastatic potential, and a more aggressive surgical resection than ANNUBP [4]. Recognising and accurately categorising these conditions is crucial for determining appropriate clinical management strategies, as MPNST demands a more vigilant and aggressive approach in contrast to the generally less aggressive nature of ANNUBP. Correct pretreatment classification is critical for optimising diagnosis and treatment of patients with peripheral nerve sheath tumours [5]. Swellings present in association with neural tissue can have the differential diagnosis of recurrent schwannoma associated with the neural tissue, neurofibroma, MPNST, plexiform neurofibroma, metastatic melanoma, pigmented neurofibroma, and ANNUBP. The stages of a neurofibroma’s malignant transition into MPNST are designated as neurofibroma with atypia, cellular neurofibroma, ANNUBP, low-grade MPNST, and high-grade MPNST based on histological characteristics [6].
The likelihood of developing MPNSTs over a lifetime is estimated to be between 8% and 13%. Early indications of malignant transformation include persistent pain, rapid tumour growth, alterations in texture upon physical examination, and the onset or worsening of neurological symptoms. Achieving a cure depends on complete surgical removal, underscoring the critical importance of early detection for effective treatment [4,7]. It is essential to treat neurofibromas as early as possible before it progresses to the malignant stage, but the early detection of neurofibromas is still a challenge. The ability of benign neurofibromas to mimic MPNST with clinical features such as increased growth rate, irregular contour, and pain has made diagnosis without surgical excision for histology challenging [8].
Therefore, a new category has been recommended, designated as “ANNUBP” for the tumours that show some worrisome features of malignant transformation but histologically fall short of MPNST [2]. MRI has been proven useful in the diagnosis of ANNUBP. Preoperative MRI and histologic findings were suggestive of ANNUBP, and hence, any aggressive treatment corresponding to MPNST was avoided. Whole-body MRI data from the National Cancer Institute (NCI) shows that most of the patients with Atypical Neurofibromas (ANF) have extensive plexiform neurofibroma tumour body burden as well as multiple nodular lesions, which may be an indicator for a higher risk of ANF and MPNST [9]. Tsuchie H et al., in their case report mentions that ANNUBP displays unique characteristics such as nuclear atypia, hypercellularity, inconsistent preservation of neurofibroma architecture, and an elevated level of mitotic activity exceeding isolated mitotic figures (more than 1 per 50 high-power fields but less than 3 per 10 high-power fields) [10]. The definitive identification of ANNUBP typically requires the presence of any two of the features mentioned above. Apart from MRI and histopathological studies, 18-Fluoro-deoxyglucose Positron Emission Tomography (FDG-PET) is considered to be a useful investigation for distinguishing between benign and malignant neurofibromas [10].
Conclusion(s)
Timely identification of ANNUBP is crucial to prevent its misdiagnosis as a malignant condition, thereby avoiding unnecessary overtreatment. Distinguishing it accurately is essential, as the more aggressive resection required for a malignant entity differs significantly from the approach for a benign condition. Preserving a limb can profoundly impact a patient’s life, emphasising the importance of prioritising the patient’s quality of life in the process. ANNUBP is still an unexplored condition, and more studies and case studies are required to reach any further conclusions.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Feb 19, 2024
Manual Googling: Apr 27, 2024
iThenticate Software: Apr 30, 2024 (16%)
[1]. Evans DGR, Malignant peripheral nerve sheath tumours in neurofibromatosis 1J Med Genet 2002 39(5):311-14.10.1136/jmg.39.5.31112011145PMC1735122 [Google Scholar] [CrossRef] [PubMed]
[2]. Hwang IS, Hahn SM, Kim HS, Kim SK, Kim HS, Shin KH, Outcomes of treatment for malignant peripheral nerve sheath tumors: Different clinical features associated with neurofibromatosis Type 1Cancer Res Treat 2017 49(3):717-26.10.4143/crt.2016.27128052660PMC5512378 [Google Scholar] [CrossRef] [PubMed]
[3]. Miettinen MM, Antonescu CR, Fletcher CDM, Kim A, Lazar AJ, Quezado MM, Histopathologic evaluation of atypical neurofibromatous tumors and their transformation into malignant peripheral nerve sheath tumor in neurofibromatosis 1 patients – a consensus overviewHum Pathol 2017 67:01-10.Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5628119/10.1016/j.humpath.2017.05.01028551330PMC5628119 [Google Scholar] [CrossRef] [PubMed]
[4]. Nelson CN, Dombi E, Rosenblum JS, Miettinen MM, Lehky TJ, Whitcomb PO, Safe marginal resection of atypical neurofibromas in neurofibromatosis type 1J Neurosurg 2020 133(5):1516-26.10.3171/2019.7.JNS19135331653805PMC8320705 [Google Scholar] [CrossRef] [PubMed]
[5]. Benz MR, Czernin J, Dry SM, Tap WD, Allen-Auerbach MS, Elashoff D, Quantitative F18-fluorodeoxyglucose positron emission tomography accurately characterizes peripheral nerve sheath tumors as malignant or benignCancer 2010 116(2):451-58.10.1002/cncr.2475519924789PMC3188986 [Google Scholar] [CrossRef] [PubMed]
[6]. Miyamoto K, Kobayashi H, Zhang L, Tsuda Y, Makise N, Yasunaga Y, Atypical neurofibromatous neoplasm with uncertain biologic potential in the posterior mediastinum of a young patient with neurofibromatosis type 1: A Case ReportCase Rep Oncol 2022 15(3):988-94.10.1159/00052684436636686PMC9830298 [Google Scholar] [CrossRef] [PubMed]
[7]. Higham CS, Dombi E, Rogiers A, Bhaumik S, Pans S, Connor SEJ, The characteristics of 76 atypical neurofibromas as precursors to neurofibromatosis 1 associated malignant peripheral nerve sheath tumorsNeuro Oncol 2018 20(6):818-25.10.1093/neuonc/noy01329409029PMC5961015 [Google Scholar] [CrossRef] [PubMed]
[8]. Raad RA, Lala S, Allen JC, Babb J, Mitchell CW, Franceschi A, Comparison of hybrid 18F-fluorodeoxyglucose positron emission tomography/magnetic resonance imaging and positron emission tomography/computed tomography for evaluation of peripheral nerve sheath tumors in patients with neurofibromatosis type 1World J Nucl Med 2018 17(4):24110.4103/wjnm.WJNM_71_1730505221PMC6216733 [Google Scholar] [CrossRef] [PubMed]
[9]. Tovmassian D, Razak MA, London K, The role of [18F] FDG-PET/CT in predicting malignant transformation of plexiform neurofibromas in Neurofibromatosis-1Int J Surg Oncol 2016 2016:616218210.1155/2016/616218228058117PMC5183794 [Google Scholar] [CrossRef] [PubMed]
[10]. Tsuchie H, Nagasawa H, Nanjyo H, Miyakoshi N, Soft tissue tumor without neurofibromatosis type 1 with histopathological suspicion of Atypical Neurofibromatous Neoplasm of Uncertain Biological Potential (ANNUBP)Cureus 2023 15(4):e3818710.7759/cureus.3818737252482PMC10221673 [Google Scholar] [CrossRef] [PubMed]