Maintaining posture, responding to voluntary motions, and adjusting to external disturbances require balance [1]. Agility, i.e., the body’s capacity to move quickly in many directions while retaining the stability of the center of gravity, is essential for balance [2]. As people age, their body’s ability to maintain balance is compromised by the central nervous system’s inability to interpret vestibular, visual, and proprioceptive information. Additionally, their ability to respond and adapt is also diminished [3]. The ability to balance has long been considered a key indicator of an older individual’s functional state. Strong evidence indicates that functional decreases in balancing performance are associated with worse health outcomes, decreased independence in daily living activities, and increased healthcare utilisation [4].
Approximately 25 to 35% of people over 65 years of age experience one or more falls yearly [5]. In essence, elderly people who are at risk of falling due to imbalance also face health issues, psychological issues, financial difficulties, or even death [6]. Hence, this should be addressed to reduce the likelihood of falling and its consequences [7]. In India, the Fear of Falling (FOF) has been reported to be 33.2% among the population above the age of 60 years. This has resulted in significant limitations in access to areas, socialisation, and quality of life. There is a significant amount of morbidity and mortality associated with FOF [8]. Balance impairment among the elderly has been the main cause of FOF, and it has a clear correlation with fall rates. Cognitive deficits and poor balance render an elderly person 5.4 times more susceptible to falls compared to those of similar age without such deficits [9].
Improving the conditions under which the vestibular, ocular, and somatosensory systems receive sensory information is necessary to prevent falls by activating the muscles of the effector system and promoting balance [10]. Improved balance and coordination, along with increased motor neuron recruitment and resistance to muscle exhaustion and hypertrophy—especially of type II fibers—also lower the incidence of falls in older adults [11]. The American Geriatric Society panel made a general observation that exercise is one strategy used to encourage responses that promote balance, thereby reducing falls among the elderly [12]. Tai Chi, a land-based activity, has also been demonstrated to lower the risk of falls in older individuals living in communities [13]. However, some individuals may find land-based programs challenging due to conditions such as pain or FOF.
Since multiple inputs are needed for balance (including proprioception, kinaesthesia, visual, and vestibular inputs), training for balance becomes a significant task. Aquatic training presents an alternative for these individuals due to the physical characteristics of water: its warmth helps to reduce muscle spasms, its buoyancy relieves sore joints, and its viscosity prolongs the time needed for balance recovery when disturbed. Additionally, water pressure enhances balance reactions by supporting the body’s proprioception in space [14]. Compared to land-based programs, these benefits may increase the acceptability of interventions and self-management for aquatic programs. There is evidence to support the use of water therapy for retraining balance [15], but detailed suggestions for the most effective procedures are scarce.
Ai Chi is a form of aquatic intervention and relaxation program that has evolved from Tai Chi on land. It involves slow, flowing movements combined with deep breathing, promoting relaxation, strength, and improved range of motion [16]. Ai Chi has been recognised as an emerging method for falls prevention and balance retraining [17]. An Ai Chi program has been shown to positively impact both balance and FOF.
While existing literature supports aquatic therapy for balance improvement, it primarily focuses on Western populations [18,19]. However, there is a paucity of research exploring the efficacy of Ai Chi, a holistic aquatic exercise, particularly in the Indian context. Given the cultural and societal factors influencing healthcare preferences in India, it is essential to investigate the applicability and effectiveness of interventions like Ai Chi. This study aims to bridge this gap by evaluating the impact of Ai Chi on balance in older Indian adults, providing evidence-based support for its integration into rehabilitation programs.
Materials and Methods
This single-blinded randomised controlled trial was conducted in Bangalore, Karnataka, India, from January 2023 to June 2023, over a duration of six months, during which the assessor was blinded. The source of data was community-dwelling elderly individuals residing in Bangalore, Karnataka, India. The study took place in an indoor temperature-controlled swimming pool with a depth of 4-5 feet and a temperature maintained between 30-34o Celsius. The study faced many challenges due to the impact of COVID-19. Pandemic-related restrictions, fear of infections, and the need to convince elderly participants to enter the pool resulted in limited recruitment.
The study was duly presented to the Institutional Review Board on January 7, 2020 (Ethical certificate no. HHEIEC/REV/188/2020), and subsequently to the Assam Downtown University Ethics Committee on December 22, 2021. However, the study could only commence in January 2023 due to COVID-19 restrictions. Informed consent was obtained from all participants before the study began.
Inclusion criteria: 1) Older adults aged 60 years and above [20] of both genders; 2) Having good cognitive function as assessed by the Clock Drawing Test (CDT) [21]; 3) BBS score <44/56 [22]; 4) Subjects with one of the following reported histories: FOF, a history of at least one fall in the past two years, or a referral from a physician for balance training.
Exclusion criteria: 1) Subjects who are hydrophobic or allergic to chlorine; 2) Unstable vital signs; 3) Co-morbidities that make it difficult to participate in water activities; and 4) Participants undergoing other physical therapy interventions for balance within the past three months.
Sample size estimation: The sample size for the study was calculated using the clinical superiority design formula [23]. The alpha value was set at 5%, and the confidence interval was taken as 95%. The beta value was 10%, with a power analysis performed at 90%. The Minimum Clinically Important Differences (MCID) for the BBS from a previous study was used to calculate the effect size, which was 12.5±0.86 [24]. Using the formula, a total sample size of 30 participants was needed, including a 25% dropout rate.
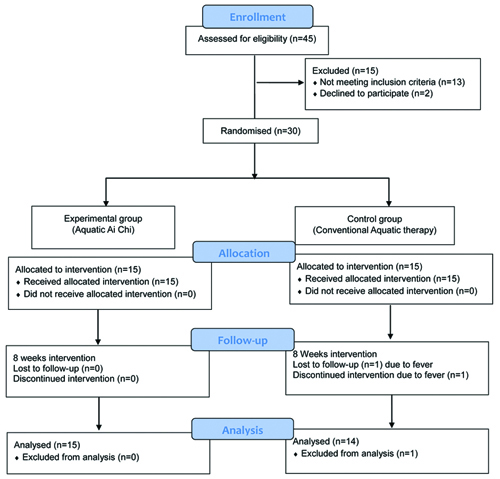
Forty-five elderly individuals gave their consent to participate in the study. Of these, 30 participants were included based on the inclusion and exclusion criteria. Two declined to participate, and 13 participants did not meet the inclusion criteria.
Methodology: The participants were provided with an information sheet that included all the details regarding the study in simple layman’s English and in the local language (Kannada). The information was also narrated to the participants and their caregivers/relatives to ensure they understood what was expected of them and what they could expect from the research. They later signed an informed consent form, giving full acceptance and cooperation for the research. Participants were randomly divided into two groups using a chit method conducted by a neutral person who was not involved in the study. The study consort is presented in [Table/Fig-1].
The experimental group received Ai Chi aquatic intervention [25], while the control group received conventional aquatic therapy based on Halliwick principles [26].
Both groups participated in each session for 40 minutes, three sessions per week for eight consecutive weeks. Every subject in both groups began with a warm-up lasting five minutes, which consisted of active free oscillatory movements emphasising the joint’s end range. The movements were performed rhythmically for five to ten repetitions across all joints of the bilateral lower limbs, upper limbs, and trunk. Group-specific exercises were conducted for a duration of 30 minutes. Following the group-specific exercises, cool-down exercises were performed for five minutes, incorporating techniques such as ninja walking and other forms that promote fascial resilience. The following Ai Chi aquatic therapy protocol was followed [Table/Fig-2,3,4, and 5].



Antero-posterior stability.

Balance exercises, both standing and/or walking, for 20 minutes, divided into five random blocks of four minutes each;
Slow agility walking: forward, backward, and sideways in a random order, including directional changes and stop-go turns [Table/Fig-2];
Ai Chi katas, depending on ability, focusing on mediolateral stability, hip strategies, and limits of reaching [Table/Fig-3,4];
Walking with obstacles and/or performing double tasks and/or silly walks;
Ai Chi as in B, but focusing on anterior-posterior stability, with only one kata performed to both sides [Table/Fig-5];
Walking with an emphasis on muscle power and fast agility.
The conventional aquatic therapy protocol was as follows [Table/Fig-6,7 and 8]:
Sagittal rotation control.
Transverse rotation control.

Dual-tasking and multitasking tasks were provided to participants, who were expected to maintain balanced standing while engaged in both motor and motor-cognitive tasks.
Negotiating obstacles: Participants were instructed to walk while avoiding obstacles that were either placed on the floor or floats that needed to be circumvented while walking toward their destination.
The study utilised the BBS, DGI, and TUGT to assess the changes that occurred following the intervention. Balance was the primary outcome, which was approached from three dimensions. The BBS is widely used to objectively determine a patient’s ability (or inability) to safely balance during a series of predetermined tasks [27].
The Minimal Detectable Change at 95% confidence (MDC95) for the BBS in older adults indicates that a seven-point or greater difference in scores (MDC95=6.2 points) is required to confidently assert that a true change in balance has occurred [28,29]. Clinicians utilise the DGI as an outcome measure to evaluate a patient’s adaptability in gait in response to changing task demands [30]. Originally designed for older adults, a 3-point (MDC95=2.9) difference between testing sessions is necessary to be confident that a true change has occurred [31]. The DGI demonstrated strong inter-rater reliability (r=0.96) and test-retest reliability (r=0.98) when administered to 44 older adults living in the community [32]. The TUGT evaluates functional mobility and can be used to assess an older person’s risk of falling. A duration of more than 12.47 seconds on the TUGT was found to be predictive of falls in older individuals living in the community, according to a prospective study by Alexandre TS et al., [33].
The outcome measure assessments were conducted by an observer who was blinded, before the intervention (pretest-P1), at the end of the 4th week of the intervention (post-test 1-P2), and at the end of the 8th week of the intervention (post-test 2-P3).
Statistical Analysis
Statistical Package for the Social Sciences (SPSS) version 23.0 was used to conduct the statistical analysis for the study. The demographic data were analysed using Chi-square analysis to assess baseline homogeneity. Outcome measures were categorised into parametric and non parametric data. The BBS, DGI, and TUG were treated as parametric data; therefore, an independent t-test was used for between-group analyses, while a dependent t-test was used for within-group analysis. A Bonferroni test was applied to analyse differences between groups, with a p-value <0.01 considered statistically significant.
Results
There was only one dropout from the control group and none from the Ai Chi group, resulting in 29 participants completing the study. Participants’ demographic data are summarised in [Table/Fig-9].
Baseline demographics and clinical characteristics of patients.
| Demographics | Age (years) | Gender n (%) | Number of fall |
|---|
| Mean±SD | Male | Female | Median | Range |
|---|
| Ai Chi (N=15) | 71.6±5.93 | 8 (53.3) | 7 (46.7) | 1 | 0-5 |
| Control (N=15) | 72.4±5.22 | 7 (46.7) | 8 (53.3) | 2 | 0-5 |
Participants in both groups were similar in age, with a mean age of approximately 72 years and a standard deviation of five years. Baseline assessments revealed no significant differences between the groups in terms of balance function, as measured by the BBS, TUGT, and DGI.
The mean baseline scores for the BBS, TUGT, and DGI were approximately 39, 13 seconds, and 14, respectively. Initial outcome data showed some differences between groups, particularly on the DGI, with the Ai Chi group demonstrating more confidence in their balance. Shapiro-Wilk test results revealed that the pretest data for both Group A and Group B were normally distributed [Table/Fig-10].
Analysis of pretest data for normal distribution of sample.
| Parameters | Shapiro-Wilk test | p-value | Conclusion |
|---|
| BBS Pretest scores for both groups | 0.977 | 0.512 | Fail to reject the null hypothesis |
| TUGT Pretest scores for both groups | 0.959 | 0.112 | Fail to reject the null hypothesis |
| DGI Pretest scores for both groups | 0.960 | 0.117 | Fail to reject null hypothesis |
BBS: Berg balance scale; TUGT: Timed up and go test; DGI: Dynamic gait index
The dependent t-test analysis showed significant improvement in both the Ai Chi and control groups (p-value <0.01) for BBS and TUGT scores. These analyses indicated that, by the end of the eight-week intervention, measures of static and dynamic balance had improved [Table/Fig-11].
Comparison of pretreatment and post-treatment evaluation parameters of the Ai Chi group and control group.
| Outcome score | Ai Chi Group A Mean±SD | Control Group B Mean±SD | Total cohort Mean±SD |
|---|
| BBS-P1 | 39.93±3.41 | 38.20±5.12 | 39.06±4.26 |
| BBS-P2 | 43.733±4.7127 | 40.333±5.2735 | 42.03±4.99 |
| BBS-P3 | 48.533±3.1593 | 43.933±5.5865 | 46.23±4.36 |
| TUGT-P1 | 12.80±1.66 | 13.87±2.77 | 13.33±2.21 |
| TUGT-P2 | 11.067±2.8652 | 12.400±3.0426 | 11.73±2.95 |
| TUGT-P3 | 9.667±2.1931 | 11.667±2.7430 | 10.66±2.46 |
| DGI-P1 | 15.87±3.14 | 12.40±2.77 | 14.13±2.65 |
| DGI-P2 | 18.067±3.1502 | 13.333±3.1091 | 15.69±3.12 |
| DGI-P3 | 18.533±2.9488 | 13.933±3.6148 | 16.23±3.27 |
BBS: Berg balance scale; TUGT: Timed up and go test; DGI: Dynamic gait index; P1: Pretest; P2: Post-test 1; P3: Post-test 2; Group-A: Ai Chi group; Group-B: Control group
A post-hoc analysis of BBS scores revealed both short-term and long-term improvements in the Ai Chi group, with significant differences found between the pretest and post-test 1 (MD=3.80, p=0.005), post-test 1 and post-test 2 (MD=4.80, p<0.001), and between the pretest and post-test 2 (MD=8.608, p<0.001). The Mean Difference (MD) indicated that the improvement was sustained; in fact, the improvement from post-test 1 to post-test 2 was greater than the improvement from pretest to post-test 1. In contrast, the control group also showed improvement, but it was not as pronounced [Table/Fig-12].
Comparison of percent change and difference scores of clinical parameters between groups.
| Bonferroni test | Within the group | Between the group |
|---|
| Outcome measures | Timeline | Groups | Mean Difference (SD) | Change % | p-value | A Vs B |
|---|
| BBS | P1-P2 | Group A | -3.80±2.01 | 9.52 | <0.01 | 0.008 |
| Group B | -2.13±1.06 | 5.58 | <0.01 |
| P1-P3 | Group A | -8.60*±1.55 | 21.54 | <0.01 | <0.01 |
| Group B | -5.73±2.09 | 15.01 | <0.01 |
| P2-P3 | Group A | -4.80±2.48 | 10.98 | <0.01 | 0.15 |
| Group B | -3.60±1.92 | 8.93 | <0.01 |
| TUGT | P1-P2 | Group A | 1.73±1.58 | 13.54 | 0.002 | 0.568 |
| Group B | 1.47±0.83 | 10.58 | <0.01 |
| P1-P3 | Group A | 3.13*±1.13 | 24.48 | <0.01 | 0.017 |
| Group B | 2.20±0.86 | 15.87 | <0.01 |
| P2-P3 | Group A | 1.40±1.06 | 12.65 | <0.01 | 0.828 |
| Group B | 0.73±0.80 | 5.91 | 0.006 |
| DGI | P1-P2 | Group A | -2.20±0.86 | 13.87 | <0.01 | <0.01 |
| Group B | -0.93±0.80 | 7.53 | 0.001 |
| P1-P3 | Group A | -2.67±1.18 | 16.81 | <0.01 | 0.0032 |
| Group B | -1.53±1.55 | 12.37 | 0.004 |
| P2-P3 | Group A | -0.47±0.74 | 2.58 | 0.058 | 0.692 |
| Group B | -0.60±1.06 | 4.50 | 0.090 |
BBS: Berg balance scale; TUGT: Timed up and go test; DGI; Dynamic gait index; P1: Pretest; P2: Post-test 1; P3: Post-test 2; Group-A: Ai Chi group; Group-B: Control group
*improvement more than 40%
Discussion
The present study aimed to investigate the efficacy of Ai Chi aquatic therapy in improving balance among older adults in the Indian population. The results indicate significant improvements in balance parameters, particularly in the Ai Chi group compared to the control group.
The demographic characteristics of the two groups were comparable and homogeneous, suggesting that the groups were well-matched at baseline. The mean age of participants in both groups was around 72 years, with a standard deviation of approximately five years. Both groups exhibited similar baseline scores on the BBS, TUGT, and DGI, indicating comparable levels of balance function. The mean BBS score for both groups was around 39, the mean TUGT score was around 13 seconds, and the mean DGI score was around 14.
Older adults, due to age-related changes, are susceptible to impaired balance, increased disability, and a higher risk of falls. To address these issues, present study evaluated the impact of an aquatic exercise program specifically focusing on dynamic balance (TUGT and DGI) and static balance (BBS). The findings indicated that aquatic exercise can improve these parameters in elderly individuals. Both the Ai Chi and control groups demonstrated significant improvements (p-value <0.01) in all balance measures. The Ai Chi group exhibited significantly greater improvements in the BBS and TUGT compared to the control group, particularly at the end of the 8th week. It showed a significant improvement of 9.8 points on the BBS from pretest to post-test 2. The mean difference in BBS scores between the Ai Chi and control groups at post-test 2 was 4.6 points. More than half of the participants demonstrated an improvement in the BBS score that was above the MDC. The total cohort’s mean±SD for the BBS before therapy were 39.06±4.26 and after eight weeks 46.23±4.36, showing a difference of more than 5 points. Similarly, in a study conducted by Donoghue D, the MDC for the BBS was reported to be 5 points for individuals scoring within the 35-44 range [29]. Another study conducted by Pérez de la Cruz, demonstrated that a 10-week, twice-weekly Ai Chi aquatic exercise program improved functionality in terms of balance, with an improvement of more than seven points in the BBS for patients with Parkinson’s disease [34]. Bei N et al., also found that an 8-week aquatic physical activity program can improve balance in hemiplegic patients [35].
The combined cohort’s mean±SD for the TUG in the present study before therapy was 13.33±2.21 and after therapy was 10.66±2.46, which were significant (p-value=0.013). This initial score, which was slightly higher than 13 seconds, has been identified as a predictor of fall risk according to Shumway Cook A et al., [32]. After eight weeks of intervention, the percentage of individuals at risk for falls dropped from 42% to 20%. The changes were not only statistically significant but also clinically meaningful. These findings were consistent with previous studies, such as that of Silva LAD et al., who investigated the effects of aquatic exercises on depression and functional mobility in elderly individuals. A significant decrease in TUG test values was observed in the experimental group (7.68±0.3 sec) compared to pretest scores (11.5±0.7 sec) (p<0.05) [36].
The combined cohort’s mean±SD of DGI scores in the present study before therapy was 14.13±2.65 and after therapy was 16.23±3.27, which were also significant (p-value=0.003). According to Romero S et al., older adults require a minimum of a 3-point difference (MDC95=2.9) between testing sessions to be confident that a true change has occurred [31]. The difference here was less than 2.9; hence, even though these changes are statistically significant, we would prefer to see a larger improvement in DGI scores clinically. This could be due to the ceiling effect and low responsiveness, as reflected in DGI scores in this study, indicating higher-functioning older adults. Avelar NC et al., similarly found that an aquatic exercise program can improve static and dynamic balance in elderly people. Forty minutes of bi-weekly sessions for six weeks resulted in increased balance when measured on the DGI (p-value <0.05) [3].
When comparing the two groups in the present study, Ai Chi outperformed the control group. Present study results align with previous studies. A study conducted on older adults in Hong Kong by Wong TWL in 2019 concluded that Ai Chi aquatic exercise can be established as a feasible, safe, and effective program for the prevention of falls in older adults at risk of falling [37]. Another study by Ku PH et al., suggested that Ai Chi was more effective than conventional water-based exercise. With 18 sessions over six weeks, Ai Chi proved to be more effective than conventional water-based exercise in enhancing anteroposterior balance control and lower extremity motor function [16]. The sustained improvement observed in the Ai Chi group underscores its potential as a long-term strategy for enhancing balance in older adults and reducing the risk of falls.
Ai Chi exercises are slow and methodical, practitioners can focus on their form and maintain perfect alignment, which improves postural stability and lowers the chance of falling [38]. It incorporates elements of Tai Chi, a traditional Chinese martial art known for its numerous health benefits, including improved balance, flexibility, and muscle strength. By integrating Tai Chi principles into aquatic therapy, Ai Chi provides a unique and effective approach to balance training that addresses both the physical and mental aspects of balance control [39,40].
Though aquatic therapy offers numerous benefits for older adults, including improved balance, strength, and flexibility, the present study’s feasibility in India faced challenges such as the limited availability of accessible temperature-controlled pools and the willingness of older adults to participate in aquatic activities. To increase the feasibility of aquatic therapy for the elderly in India, it is essential to address these challenges and create a supportive environment. This may involve raising awareness about the benefits of aquatic therapy.
Limitation(s)
There were several limitations to the study. The study had a limited sample size due to the unprecedented pandemic, which could affect the generalisability of the findings to a larger population of older adults. The study’s findings may be limited in their applicability to other populations or settings, such as individuals with different levels of mobility or those receiving aquatic therapy interventions outside of a controlled research environment. Future research should investigate the underlying mechanisms of Ai Chi’s effectiveness, conduct long-term follow-ups, and explore its application in diverse populations and settings to optimise its therapeutic benefits.
Conclusion(s)
This study demonstrates that both conventional and Ai Chi aquatic therapy are effective interventions for reducing balance impairment in Indian elderly individuals. However, Ai Chi interventions indicated comparatively better improvements in balance parameters, suggesting the potential of Ai Chi as a valuable addition to fall prevention strategies for this population. The slow and controlled nature of Ai Chi movements likely promotes better postural control and reduces the risk of falls. Further research is needed to explore the long-term effects of Ai Chi and its applicability to diverse elderly populations.
BBS: Berg balance scale; TUGT: Timed up and go test; DGI: Dynamic gait index
BBS: Berg balance scale; TUGT: Timed up and go test; DGI: Dynamic gait index; P1: Pretest; P2: Post-test 1; P3: Post-test 2; Group-A: Ai Chi group; Group-B: Control group
BBS: Berg balance scale; TUGT: Timed up and go test; DGI; Dynamic gait index; P1: Pretest; P2: Post-test 1; P3: Post-test 2; Group-A: Ai Chi group; Group-B: Control group
*improvement more than 40%