OA staging can be performed according to the Kellgren-Lawrence (KL) classification [10]. HHS is sensitive for diagnosing coxarthrosis [11]. Treatment options include lifestyle changes, physical therapy, medical treatments, injections and surgery. Non Steroidal Anti-inflammatory Drugs (NSAIDs) and acetaminophen are used as first-line treatments. New treatments, such as nerve blocks, mesenchymal stem cell injections, Platelet-Rich Plasma (PRP) injections and ozone therapy, are being investigated [12]. Steroid treatments, specifically intra-articular corticosteroid injections, are commonly used to manage pain and inflammation in patients with coxarthrosis (hip OA). When performed under ultrasound guidance, these injections offer several advantages [13].
Ozone therapy accelerates anabolic mechanisms, provides vascularisation of cartilage and bone, and slows down the degenerative process. Additionally, it affects inhibitory cytokines, antioxidant enzymes and neoangiogenesis. Ozone is involved in stimulating fibroblasts, chondrocytes and stem cells in the joint repair process. Research has shown that ozone reduces local pain and improves joint function and mobility. Ozone can be administered intra-articularly and periarticularly, with a very low-risk of complications [14,15].
Hence, the present study aimed to evaluate and compare the effectiveness of ultrasound-guided intra-articular ozone therapy and corticosteroid injections in managing hip OA (coxarthrosis) in patients who have not responded to conventional treatments.
Materials and Methods
A retrospective comparative analysis was conducted at Ankara Training and Research Hospital, Ankara, Turkey, from August 2021 to August 2022. Ethical approval was obtained from the ethics committee for the study (ethical approval number: 1049/2022). This study uses a retrospective design, sourcing patient data from hospital archives. Clinical findings for all clinic visitors are documented as pretreatment data. Patients who had intra-articular hip interventions were scheduled for follow-ups at 1, 3, and 6 months, during which detailed clinical information was recorded. After obtaining ethical approval, patient data was retrieved. Patients who received injections for coxarthrosis during this period were included in the study [Table/Fig-1].
Flowchart diagram.
PRP: Platelet rich plasma; PRF: Pulsed radiofrequency
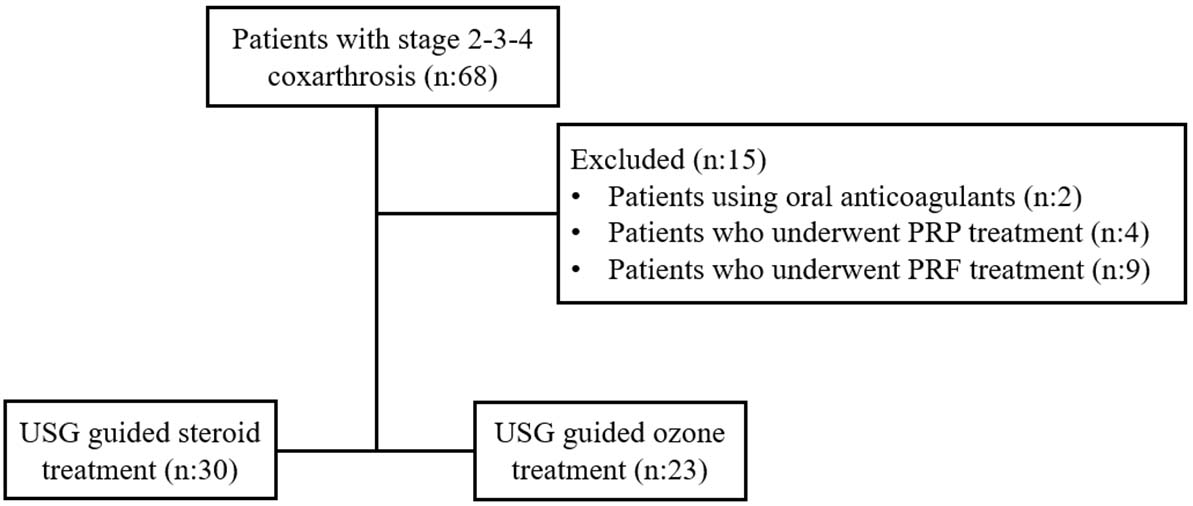
Inclusion criteria: Participants aged 50-85 years, who were resistant to conventional treatments, were not candidates for surgery, or preferred not to undergo surgery, as well as patients with hip OA classified as Kellgren-Lawrence grade ≥2 and a VAS score ≥4 [10], were included in the study.
Exclusion criteria: Patients who had received other treatments for the hip joint (e.g., radiofrequency, PRP) in the past year, those with bleeding disorders, allergies to the medications used in the study, septic arthritis, skin or systemic infections at the injection site, uncontrolled hyperthyroidism, poorly regulated hypertension or diabetes mellitus, pregnant women, and patients with G6PD enzyme deficiency for whom ozone injection was contraindicated were excluded from the study.
Study Procedure
Group A (n=30) received an intra-articular steroid (triamcinolone acetonide), while Group B (n=23) received three weekly ozone sessions (200 μg/20 mL), both under USG guidance [16]. Changes in VAS, HHS [11], and the average number of analgesic use days per month before and after treatment were evaluated and compared between the two groups.
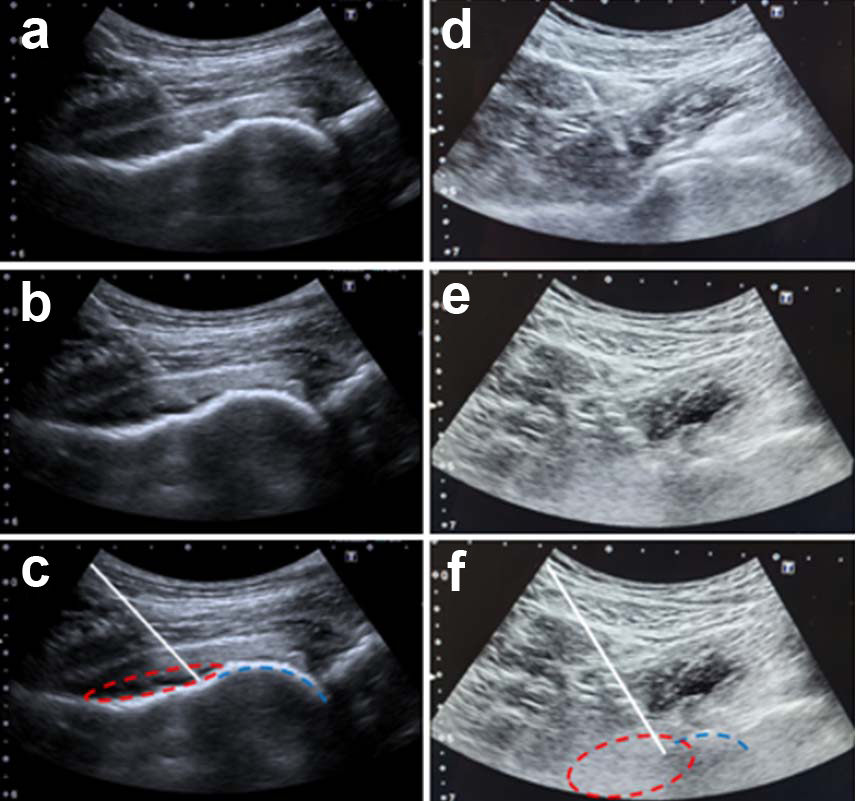
Patients were asked to lie down on the examination table after monitors were placed. The intervention site was cleaned using povidone-iodine. A 22-gauge Quincke needle was inserted using an in-plane approach with a 1.5-6 MHz convex USG probe. After administering 3 mL of 2% prilocaine intra-articularly, 20 mL of ozone at a dose of 10 μg/mL was administered through the same needle for a total of three weekly sessions. For patients who received corticosteroids, 3 mL of 2% prilocaine and 1 mL of corticosteroid (40 mg triamcinolone acetonide) were administered. Pre- and post-injection images of two patients who underwent ozone and drug injections using a Toshiba Aplio 500 USG device are illustrated in [Table/Fig-2a-f].
a) Drug (Steroid+local anaesthetic) injection pre-USG image; b) The drug injection post-USG image; c) White line: needle, Dashed red line: Represents the distribution of the local anaesthetic and steroid mixture within the joint, Dashed blue line: Represents the femoral head); d) Ozone injection pre-USG image; e) Ozone injection post-USG image; f) White line: Needle, Dashed red line: Indicates the spread of ozone within the joint, Dashed blue line: Represents the femoral head).
Statistical Analysis
Data analysis was conducted using Statistical Package for the Social Sciences (SPSS) version 20.0. The Shapiro-Wilk test was employed to assess normal distribution. Statistical analysis included unpaired t-tests, repeated measures Analysis of Variance (ANOVA), post hoc Bonferroni tests, Fisher’s exact test, and Chi-square tests. A p-value <0.05 was considered significant.
Results
The mean age of the participants included in the study was 63.23±10.50 years (min: 50, max: 85). A total of 53 patients were included in the study, with 30 in Group A and 23 in Group B. Gender distribution is presented in [Table/Fig-3]. There were 15 patients with Kellgren-Lawrence stage 2, 20 patients with stage 3, and 18 patients with stage 4. No significant difference was found between the groups in terms of gender distribution and coxarthrosis stage (p=0.089, p=0.066, respectively). When the analgesic needs were compared pre- and postintervention within the same group, the analgesic needs decreased significantly in both groups, with a p-value of <0.001 [Table/Fig-4].
Gender distribution according to groups.
| Gender | Group | p-value |
|---|
| A | B | Total |
|---|
| Male | Count | 9a | 2a | 11 | 0.089 |
| % within group | 30.0% | 8.7% | 20.8% |
| Female | Count | 21a | 21a | 42 |
| % within group | 70.0% | 91.3% | 79.2% |
| Total | Count | 30 | 23 | 53 |
| % within group | 100.0% | 100.0% | 100.0% |
(Each subscript letter denotes a subset of Group categories whose column proportions do not differ significantly from each other at the 0.05 level, as determined by Fisher’s exact test.)
Changes in the amount of analgesic within the group.
| Analgesic need | Groups |
|---|
| A (n:30) | B (n:23) |
|---|
| 1st week | 1st month | 3rd month | 6th month | p-value | 1st week | 1st month | 3rd month | 6th month | p-value |
|---|
| Decreased | 15 (50) | 23 (76.7) | 16 (53.3) | 7 (23.3) | <0.001 | 17 (73.9) | 17 (73.9) | 10 (43.5) | 4 (17.4) | <0.001 |
| Not changed | 15 (50) | 7 (23.3) | 12 (40.0) | 18 (60.0) | 6 (26.1) | 5 (21.7) | 13 (56.5) | 17 (73.9) |
| Increased | - | - | 2 (6.7) | 5 (16.7) | | 1 (4.3) | | 2 (8.7) |
*Chi-square test, **p-value <0.05
However, no significant difference was found in analgesic needs over time when comparing the two groups at 1 week, 1 month, 3 months and 6 months (p-values=0.139, 0.724, 0.391, and 0.546) [Table/Fig-5].
Intergroup comparison of analgesic requirement.
| Groups | Time | Analgesic need (n) | p-value* |
|---|
| Decreased | Not changed | Increased |
|---|
| Group A (n:30) | 1st week | 15 | 15 | - | 0.139 |
| Group B (n:23) | 17 | 6 | - |
| Group A | 1st month | 23 | 7 | 0 | 0.724 |
| Group B | 17 | 5 | 1 |
| Group A | 3rd month | 16 | 12 | 2 | 0.391 |
| Group B | 10 | 13 | 0 |
| Group A | 6th month | 7 | 18 | 5 | 0.546 |
| Group B | 4 | 17 | 2 |
Chi-square test, p-value <0.05
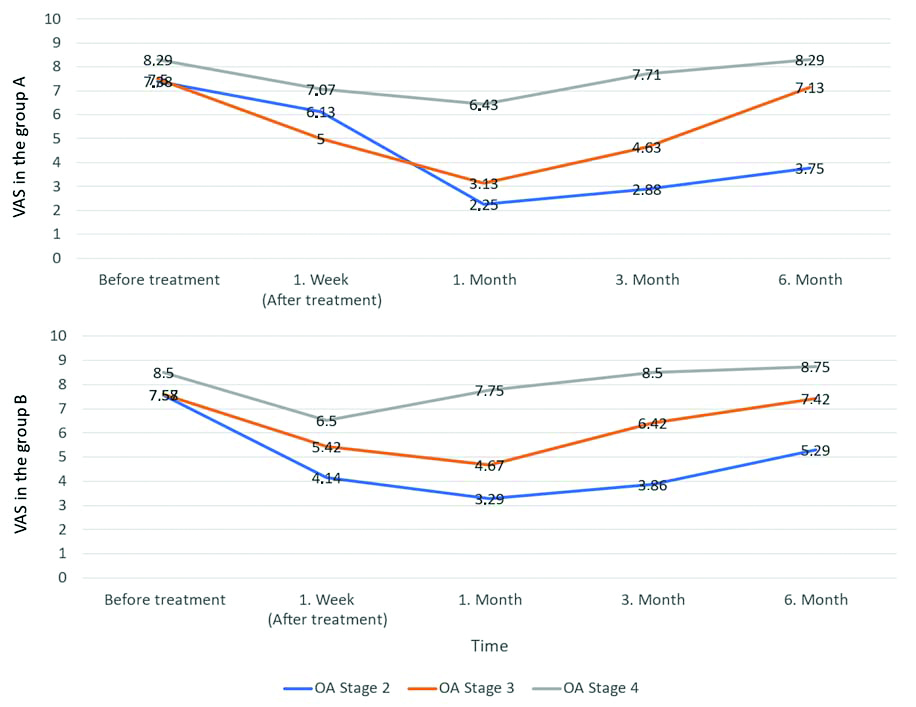
Comparison of VAS scores: When the VAS scores of the treatment groups were evaluated according to the coxarthrosis stage, it was found that the decrease in VAS scores was significant in stages 2 and 3 in both treatment groups, and the effect size decreased as the stage increased [Table/Fig-6]. In stage 2, significant short-term results were obtained regarding pain improvements at one week and one month, with p-values of 0.014 and 0.031. However, in stages 3 and 4, while some short-term improvements were noted, long-term outcomes showed limited progress, and no significant differences were found between the groups [Table/Fig-7].
Comparison of VAS scores within treatment groups.
| Groups | Coxarthrosis stage | VAS before treatment | VAS 1st week (After-treatment) | VAS 1st month | VAS 3rd month | VAS 6th month | p
and
partial eta2 |
|---|
| Group A | 2 | Mean | 7.38 | 6.13 | 2.25 | 2.88 | 3.75 | 0.001 |
| SD | 0.518 | 1.553 | 0.707 | 1.246 | 2.252 | 0.817 |
| 3 | Mean | 7.50 | 5.00 | 3.13 | 4.63 | 7.13 | 0.001 |
| SD | 0.756 | 1.690 | 0.835 | 2.326 | 1.246 | 0.689 |
| 4 | Mean | 8.29 | 7.07 | 6.43 | 7.71 | 8.29 | 0.002 |
| SD | 0.726 | 1.542 | 2.102 | 1.541 | 0.726 | 0.380 |
| Group B | 2 | Mean | 7.57 | 4.14 | 3.29 | 3.86 | 5.29 | <0.001 |
| SD | 0.787 | 1.069 | 0.951 | 1.464 | 2.059 | 0.739 |
| 3 | Mean | 7.58 | 5.42 | 4.67 | 6.42 | 7.42 | <0.001 |
| SD | 0.793 | 2.392 | 2.188 | 2.109 | 0.996 | 0.488 |
| 4 | Mean | 8.50 | 6.50 | 7.75 | 8.50 | 8.75 | 0.089 |
| SD | 0.577 | 1.291 | 1.258 | 0.577 | 0.500 | 0.553 |
ANOVA, p<0.05
Comparison of VAS between treatment groups.
| Coxarthrosis stage and groups | VAS Before treatment | VAS 1st week (After-treatment) | VAS 1st month | VAS 3rd month | VAS 6th month |
|---|
| 2 | Group A | Mean | 7.38 | 6.13 | 2.25 | 2.88 | 3.75 |
| SD | 0.518 | 1.553 | 0.707 | 1.246 | 2.252 |
| Group B | Mean | 7.57 | 4.14 | 3.29 | 3.86 | 5.29 |
| SD | 0.787 | 1.069 | 0.951 | 1.464 | 2.059 |
| p-value | 0.014 | 0.031 | 0.184 | 0.194 |
| 3 | Group A | Mean | 7.50 | 5.00 | 3.13 | 4.63 | 7.13 |
| SD | 0.756 | 1.690 | 0.835 | 2.326 | 1.246 |
| Group B | Mean | 7.58 | 5.42 | 4.67 | 6.42 | 7.42 |
| SD | 0.793 | 2.392 | 2.188 | 2.109 | 0.996 |
| p-value | 0.676 | 0.075 | 0.091 | 0.569 |
| 4 | Group A | Mean | 8.29 | 7.07 | 6.43 | 7.71 | 8.29 |
| SD | 0.726 | 1.542 | 2.101 | 1.541 | 0.726 |
| Group B | Mean | 8.50 | 6.50 | 7.75 | 8.50 | 8.75 |
| SD | 0.577 | 1.291 | 1.258 | 0.577 | 0.500 |
| | p-value | | 0.511 | 0.254 | 0.341 | 0.252 |
*unpaıred t-test
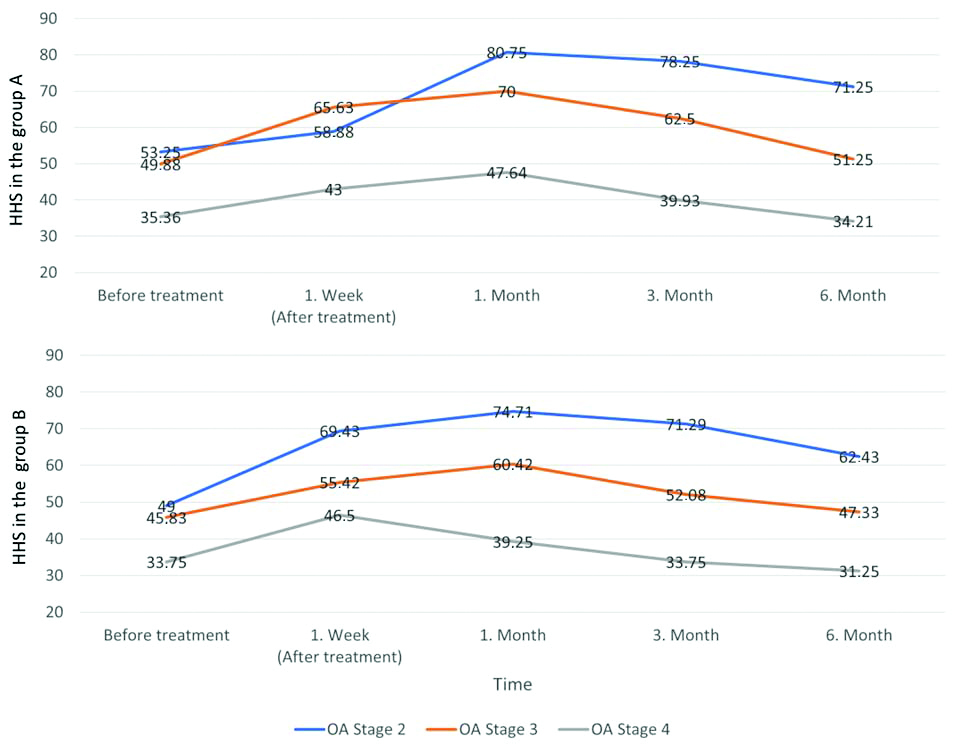
Comparison of Harris Hip Scores (HHS): When the HHS scores of the treatment groups were evaluated according to the coxarthrosis stage, it was found that the increase in HHS scores was significant in stages 2 and 3 in both treatment groups, and the effect size decreased as the stage increased. In stage 2, both interventions were found to be effective. In stage 3, the effect size of steroids was greater, while ozone treatment had a moderate effect. In stage 4, the increase in HHS scores was significant in Group A, but the effect was weak, and the effect of ozone treatment on HHS scores in stage 4 was not significant in Group B [Table/Fig-8].
Comparison of HHS scores within treatment groups.
| Group | Coxarthrosis stage | HHS before
treatment | HHS 1st week (After
treatment) | HHS 1st month | HHS 3rd month | HHS 6th month | P and partial eta2 |
|---|
| Group A | 2 | Mean | 53.25 | 58.88 | 80.75 | 78.25 | 71.25 | <0.001 |
| SD | 6.902 | 4.190 | 4.773 | 7.960 | 8.940 | 0.790 |
| 3 | Mean | 49.88 | 65.63 | 70.00 | 62.50 | 51.25 | 0.004 |
| SD | 5.222 | 9.797 | 5.345 | 12.247 | 7.025 | 0.597 |
| 4 | Mean | 35.36 | 43.00 | 47.64 | 39.93 | 34.21 | <0.001 |
| SD | 8.872 | 13.456 | 16.113 | 15.117 | 9.209 | 0.391 |
| Group B | 2 | Mean | 49.00 | 69.43 | 74.71 | 71.29 | 62.43 | <0.001 |
| SD | 5.354 | 8.324 | 5.936 | 10.111 | 10.983 | 0.722 |
| 3 | Mean | 45.83 | 55.42 | 60.42 | 52.08 | 47.33 | <0.001 |
| SD | 6.686 | 13.222 | 14.687 | 14.055 | 9.480 | 0.438 |
| 4 | Mean | 33.75 | 46.50 | 39.25 | 33.75 | 31.25 | 0.101 |
| SD | 6.292 | 7.681 | 6.397 | 6.292 | 6.292 | 0.540 |
A repeated measures ANOVA was applied, and the significant p-value p<0.05
In stage 2, significant short-term results were obtained regarding functional improvements (one week and one month), with a notable improvement in functional scores for Group B observed particularly at one week. However, in stages 3 and 4, while some short-term improvements were noted, long-term outcomes showed limited progress, and no significant differences were found between the groups [Table/Fig-9].
Comparison of HHS between treatment groups.
| Coxarthrosis stage and groups | HHS before treatment | HHS 1st week (After-treatment) | HHS 1st month | HHS 3rd month | HHS 6th month |
|---|
| 2 | Group A | Mean | 53.25 | 58.88 | 80.75 | 78.25 | 71.25 |
| SD | 6.902 | 4.190 | 4.773 | 7.960 | 8.940 |
| Group B | Mean | 49.00 | 69.43 | 74.71 | 71.29 | 62.43 |
| SD | 5.354 | 8.324 | 5.936 | 10.111 | 10.983 |
| p-value | | 0.007 | 0.048 | 0.159 | 0.110 |
| 3 | Group A | Mean | 49.88 | 65.63 | 70.00 | 62.50 | 51.25 |
| SD | 5.222 | 9.797 | 5.345 | 12.247 | 7.025 |
| Group B | Mean | 45.83 | 55.42 | 60.42 | 52.08 | 47.33 |
| SD | 6.686 | 13.222 | 14.687 | 14.055 | 9.480 |
| p-value | | 0.079 | 0.096 | 0.105 | 0.332 |
| 4 | Group A | Mean | 35.36 | 43.00 | 47.64 | 39.93 | 34.21 |
| SD | 8.872 | 13.456 | 16.113 | 15.117 | 9.209 |
| Group B | Mean | 33.75 | 46.50 | 39.25 | 33.75 | 31.25 |
| SD | 6.292 | 7.681 | 6.397 | 6.292 | 6.297 |
| p-value | | 0.630 | 0.332 | 0.444 | 0.558 |
A repeated measures ANOVA was applied, and the significant p-value p<0.05
In Groups A and B, VAS and HHS values were found to be significantly lower in the first week, the first month, and the third month in the post-treatment period compared to the pre-treatment period (post-hoc Bonferroni test). However, no significant difference was found at the sixth-month interval [Table/Fig-10,11].
Change in VAS according to the stages of coxarthrosis after ozone and steroid treatment.
Change in HHS according to the stages of coxarthrosis after ozone and steroid treatment.
Discussion
Repeated ozone therapy induces the antioxidative system and provides resistance against oxidative stress. In the present study, 20 mL of ozone at a concentration of 10 μg/mL was administered intra-articularly into the hip joint once a week for a total of three sessions. This treatment method resulted in a reduction in analgesic requirements and significant improvements in HHS and VAS scores, particularly in patients with early-stage hip OA. The findings suggest that repeated ozone therapy may be an effective option, especially in the management of early-stage hip OA symptoms, and a potential alternative to corticosteroids [17]. Similar findings were noted in a study by Lopes De Jesus CC et al., which involved 98 patients who observed that intra-articular administration of 20 μg/mL once a week for eight weeks reduced OA-related pain, improved joint function, and enhanced the quality of life for patients with knee OA [15]. Corticosteroids have long been used in the treatment of OA due to their anti-inflammatory effects. Corticosteroid injections into the hip joint can reduce pain, stiffness and disability. However, it is emphasised that corticosteroids do not affect the underlying process of OA and are only useful in treating exacerbations [18]. Additionally, there are concerns that repeated intra-articular corticosteroid injections may lead to rapidly progressive OA of the hip [19].
In the present study, given that both steroid and ozone therapies demonstrated similar effects and provided symptom improvement within three months, authors believe that ozone therapy may be considered an alternative to corticosteroids. In a study conducted by Babaei-Ghazani A et al., on knee OA, 62 patients with mild to moderate knee OA were randomly divided into two groups. One group received a single dose of 40 mg triamcinolone, while the other group received a single dose of 10 cc (15 μg/mL) oxygen-ozone injection under USG guidance. Both groups were followed for three months and assessed at various time points before and after the injection. The study findings showed significant improvements in the VAS scores in both groups. However, three months after treatment, the improvement in VAS and the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores in the oxygen-ozone group was found to be significantly higher compared to the steroid group [20].
Similarly, in the present study, the improvements in VAS and HHS among the treatment groups, when evaluated according to the stage of coxarthrosis, showed significant short-term results regarding functional improvements (1 week and 1 month), particularly for Stage 2. A marked improvement in functional scores was observed in the group receiving ozone treatment at one week. However, in stages 3 and 4, while some short-term improvements were noted, long-term outcomes showed limited progress in improvements, and no significant differences were found between the groups.
Hashemi M et al., administered oxygen-ozone and prolotherapy to patients with knee OA three times at 10-day intervals and achieved significant improvements in VAS and WOMAC scores compared to baseline in both groups [21]. In this study, the effectiveness of oxygen-ozone in reducing pain in the early stages was similar to the findings of the present study.
Raeissadat SA et al., conducted a randomised clinical study with 174 patients comparing Hyaluronic Acid (HA) and ozone therapy in knee OA. They administered a total of three sessions weekly, using 30 μg/mL of ozone (10 mL) and a solution of 20 mg/2 mL of HA. The results indicated that both HA and ozone therapy were effective for patients with knee OA, with no superiority found between the two treatments [22]. The findings regarding the effectiveness of ozone therapy align with present study, suggesting that it can provide sufficient symptom relief (especially in terms of pain and stiffness) for at least six months.
The combined use of ozone therapy with PRP and HA has been shown to yield significantly better outcomes in the treatment of OA [23,24]. Future studies examining the combination of steroids and ozone therapy could help us better understand the effects of these treatment methods and their efficacy in managing OA. Such research may contribute to optimising treatment protocols and improving patient responses to therapy.
This study concludes that both intra-articular steroid and ozone therapies are effective for early-stage coxarthrosis, but both treatments are insufficient for advanced stages. This highlights the necessity of considering the disease stage in treatment planning, with surgery being essential for Stage 4 coxarthrosis and alternative treatment methods being needed. Ozone therapy offers valuable options for patients in the early stages of hip OA. The use of evaluation scales such as HHS and VAS enriches the assessment of treatment efficacy. HHS is a sensitive metric for evaluating coxarthrosis, effectively measuring pain and hip function, as well as the impact of hip disorders on daily life [11]. While HHS focuses on overall hip function and daily activities, VAS provides a more detailed assessment of pain intensity. Utilising both scales ensures a comprehensive evaluation of the functional aspects of hip OA and the patient’s pain experiences.
Limitation(s)
The choice between ozone and corticosteroid treatment methods for individuals without health issues such as diabetes mellitus, osteoporosis, and hypertension—or where corticosteroid use is not contraindicated—has been determined by the experience of the practitioner and the preference of the patient. In the study, patients without chronic diseases (such as diabetes mellitus, hypertension, or osteoporosis) and without contraindications to corticosteroid use (such as allergies, glaucoma, or a history of peptic ulcers) were considered a separate group. Participants in this group were administered 40 mg of triamcinolone acetonide along with 3 mL of 2% prilocaine. In the other group receiving ozone therapy, participants with chronic diseases opted not to undergo corticosteroid treatment. These factors are among the significant limitations of the present study.
Conclusion(s)
This study demonstrates that corticosteroid injections and ozone therapy are effective treatment options for patients with coxarthrosis, particularly those classified as Kellgren-Lawrence grades 2 and 3. Both treatments have led to significant short-term improvements in pain and function within one month, with ozone therapy showing similar analgesic effects and a favorable safety profile. However, at the six-month follow-up, no differences in long-term effectiveness were observed. Ozone therapy offers a suitable alternative for patients seeking to avoid the side-effects of corticosteroids. In patients with advanced (stage 4) OA, however, both ozone and corticosteroid therapies have proven inadequate in providing improvements in pain and functionality, as well as in delaying the need for surgical intervention. This situation highlights the necessity of developing more effective and targeted alternative treatment strategies for advanced OA cases. Future studies should investigate the efficacy of combining steroids and ozone therapy, as well as the impact of varying the number of ozone sessions and different ozone concentrations on the management of hip OA, which could enhance our understanding of treating this condition.
(Each subscript letter denotes a subset of Group categories whose column proportions do not differ significantly from each other at the 0.05 level, as determined by Fisher’s exact test.)
*Chi-square test, **p-value <0.05
Chi-square test, p-value <0.05
ANOVA, p<0.05
*unpaıred t-test
A repeated measures ANOVA was applied, and the significant p-value p<0.05
A repeated measures ANOVA was applied, and the significant p-value p<0.05