Introduction
Temporomandibular Disorders (TMD) encompass a range of conditions affecting the joint and surrounding structures, often resulting in pain, restricted movement, and dysfunction. Arthrocentesis involves the insertion of a single needle into the joint space, allowing for irrigation, lavage, and aspiration of the joint. The present procedure aims to alleviate symptoms, improve joint function, and promote healing by removing inflammatory mediators, debris, and adhesions from the joint space.
Need of the study
Arthrocentesis offers several advantages over traditional techniques, including reduced trauma, quicker recovery times, and a decreased risk of complications. It has emerged as a valuable tool in the multidisciplinary approach to managing TMDs, offering patients a minimally invasive option to relieve their symptoms and restore jaw function. Hence, the present study will present the utility of arthrocentesis as an adjunct procedure to closed reduction in high condylar fractures, improving the functionality of the condyle, providing pain relief, increasing mouth opening and bite force, stabilising bilateral occlusion, and normalising excursive movements.
Aim
To compare and evaluate the efficacy of closed reduction with or without arthrocentesis in patients with high condylar fractures regarding functional outcomes.
Materials and Methods
A randomised controlled trial will be conducted at Siddharth Gupta Memorial Cancer Hospital, Sawangi, Wardha, Maharashtra, India, from September 2024 to May 2026, involving 10 patients. The protocol includes examining patients with suspected high condylar fractures, taking detailed case histories, performing clinical examinations focusing on the Temporomandibular Joint (TMJ), and recording preoperative measurements of mouth opening and pain levels using a Visual Analogue Scale (VAS). Patients with suspected fractures will undergo radiographic examinations, and those meeting the inclusion criteria will be included in the study after providing informed consent. Arthrocentesis will be performed using a specialised needle with two lumens, inlet and outlet bevels, and a silicone stopper for maximal insertion depth. Statistical analysis will be conducted using descriptive and inferential statistics, specifically the Chi-square test and Student’s paired and Unpaired t-tests, with p-value <0.05 considered significant.
Introduction
Injury to the maxillofacial skeleton can occur from various sources, including road traffic accidents, occupational injuries, physical violence, sports injuries, and falls that impact the jaw region. The type of fracture sustained often depends on the individual’s age, as well as the direction and force of the impact. For example, a horizontal strike to the body of the mandible, such as a punch, typically results in fractures on the same side of the body and may also affect the opposite condyle. The condyle is a common fracture site due to its prominent position [1].
The mandible is one of the most frequently fractured bones [1]. Mandibular condyle fractures represent approximately 30 to 37% of all mandible fractures in both dentulous and edentulous patients. Symptoms of a condylar fracture may include pain, swelling around the ear, ear bleeding, misalignment of teeth, restricted mouth opening, and deviation of the mouth toward the affected side upon opening [2].
Management of these fractures is generally categorised into nonsurgical and surgical interventions. Open Reduction with Internal Fixation (ORIF) is the preferred treatment for bilateral condylar fractures, restricted functionality, malocclusion, or when closed reduction is likely to result in complications such as osseous or fibrous ankylosis and the risk of avascular necrosis [3].
On the other hand, closed reduction with functional therapy offers significant safety benefits. This method poses minimal risk of damaging nerves or blood vessels during the procedure and decreases the likelihood of postoperative complications, such as infection or scarring [2]. Historically, the treatment of condylar fractures focused on conservative methods aimed at achieving stable occlusion through intermaxillary fixation. The decision between conservative and surgical treatments remains a subject of ongoing debate. Conservative methods often involve varying periods of intermaxillary fixation, usually followed by intensive physiotherapy, although the optimal approach is still unclear. Regardless of the chosen treatment, rehabilitation after a mandibular condyle injury is crucial. This includes careful monitoring, a soft diet, Maxillomandibular Fixation (MMF) with wires or elastics, and aggressive physiotherapy to restore mouth function [2,4].
Many surgeons prefer surgical treatment over closed reduction due to the potential long-term complications associated with the latter, such as tenderness and pain, open bite, mandibular deviation during jaw movement, malocclusion from insufficient restoration of ramus vertical height, arthritis, and ankylosis. The goal of surgical intervention is to restore pre-existing anatomical relationships and achieve stable fixation for acceptable function [5].
The TMJ arthrocentesis is a minimally invasive surgical option for patients suffering from TMJ disorders and can also serve as an adjunctive treatment for trauma patients. The procedure involves draining the joint and potentially applying therapeutic substances. Indications for arthrocentesis include chronic or acute pain with restricted motion due to disk displacement, with or without reduction [6]. Nitzan DW et al., reported long-term success in 39 patients (40 joints) treated with arthrocentesis for acute lockjaw [7].
Additionally, intra-articular corticosteroid injections and irrigation have been shown to improve TMJ functionality and reduce discomfort in cases of mandibular condyle fractures. This is associated with increased concentrations of the cytokine Interleukin-6 (IL-6) in patients who exhibit Magnetic Resonance Imaging (MRI) evidence of Joint Effusion (JE), and a correlation has been noted between IL-6 concentrations and the severity of JE [8,9].
Therefore, the present trial aimed to compare the functional outcomes of patients treated with and without TMJ arthrocentesis after undergoing closed reduction for high condylar fractures.
Primary objectives:
To assess the effectiveness of closed reduction with arthrocentesis in improving functional outcomes for patients with high condylar fractures.
To evaluate the effectiveness of closed reduction without arthrocentesis in improving functional outcomes for patients with high condylar fractures.
Secondary objective: To compare the effectiveness of closed reduction with and without arthrocentesis in improving functional outcomes in patients with high condylar fractures.
Null hypothesis: There will be no significant difference in functional outcomes between high condylar fractures managed with closed treatment alone and those managed with closed treatment along with TMJ arthrocentesis.
Alternate hypothesis: There will be a notable difference in functional outcomes between high condylar fractures that are treated solely with closed treatment and those treated with closed treatment in combination with TMJ arthrocentesis.
Review of Literature
The TMD encompasses a variety of conditions that can greatly disrupt a patient’s day-to-day life, with symptoms such as persistent pain and restricted jaw movement. These issues often lead to significant discomfort and affect overall quality of life. General dentists frequently serve as the first point of contact for patients experiencing these challenges, making their role crucial in addressing TMD. A thorough evaluation and accurate diagnosis are essential steps in crafting an effective management plan tailored to the individual needs of the patient. For those who require surgical intervention, minimally invasive procedures like arthrocentesis and arthroscopy can be beneficial. These techniques aim to decrease inflammation by removing excess fluid and debris from the joint, ultimately alleviating pain and enhancing joint mobility [6].
Nogami S et al., conducted a comparative study examining the effects of arthrocentesis versus conventional closed reduction in unilateral mandibular high condyle fractures [9]. The research involved 30 patients presenting with unilateral high condylar fractures and magnetic resonance imaging evidence of JE. The participants were categorised into two groups: Group I received arthrocentesis with irrigation and betamethasone, while group II underwent conservative treatment with rigid fixation. Results indicated that group I demonstrated superior outcomes regarding range of motion and joint pain at both one and three months post-intervention. This study suggests that arthrocentesis may facilitate more effective and expedited healing than conventional closed reduction [9].
In a study conducted by Tino MT et al., a 56-year-old man with bilateral diacapitular mandibular condyle fractures was examined. The findings indicated that incorporating arthrocentesis into conservative treatment protocols resulted in decreased pain and improved mouth opening during the initial phases of treatment [10]. Another study led by Nogami S et al., investigated the recovery of masticatory function following arthrocentesis in patients with unilateral condylar head fractures [9]. They compared patients who underwent arthrocentesis for therapeutic purposes with those who did not. Up to three months after treatment, patients treated with arthrocentesis showed a greater occlusal contact area and maximum bite force compared to those who did not receive the procedure. Although the differences were not statistically significant, significant reductions in the occlusal contact area and maximum bite force on the fractured side compared to the non fractured side were observed at one and three months post-arthrocentesis. The study suggests that arthrocentesis, as a less invasive alternative to open reduction and internal fixation, may lead to a prolonged healing interval in cases where surgical intervention is to be avoided [11].
In a study by Sinbel A et al., the objective was to assess the effectiveness of arthrocentesis in restoring mandibular function after MMF in cases of sub-condylar fractures [12]. Arthrocentesis, or TMJ lavage, proved to be an effective procedure for removing inflammatory mediators within the TMJ post-trauma. The study demonstrated significant improvement in mandibular movements immediately after arthrocentesis, contributing to enhanced patient quality of life. Patients resumed normal activities, and rehabilitation commenced as early as the second week postoperatively. The findings suggest that arthrocentesis is a beneficial treatment modality for subcondylar fractures when combined with MMF [12].
Kondoh T et al., compared two treatment approaches for managing unilateral mandibular condyle fractures: intra-articular irrigation with corticosteroid injection (IR group) and conventional conservative treatment with closed reduction and intermaxillary fixation (CC group). The IR group, which included 14 patients, received saline irrigation along with a dexamethasone injection into the superior joint compartment, followed by standard rehabilitation. In contrast, the CC group, consisting of 12 patients, underwent closed reduction and intermaxillary fixation for two weeks before starting standard rehabilitation. The results revealed significant differences between the two groups. Early relief of joint pain was observed in the IR group. By one year post-injury, occlusal changes were noted in one patient from the IR group and four patients from the CC group [8].
Overall, these findings indicate that arthrocentesis in patients with high condylar fractures can alleviate pain associated with the TMJ and enhance mouth opening.
Materials and Methods
A randomised controlled trial will be conducted at Siddharth Gupta Memorial Cancer Hospital, Sawangi, Wardha, Maharashtra, India, from September 2024 to May 2026. A total of 10 patients will be included in the study. The trial registration has been completed on the website with Ref. No: CTRI/2024/09/073175. The Institutional Ethical Clearance has been obtained before initiating the study (Reference number: DMIHER (DU)/IEC/2024/230). Informed written consent from the patients will be obtained in their language before conducting the study.
Inclusion criteria:
Patients with unilateral high condylar fractures;
Sagittally fractured unilateral high condylar fractures;
Intracapsular fractures in the condyle unilaterally;
Patients with pan facial fractures, including unilateral high condylar fractures;
Patients within the age group of 18-60 years;
Patients with American Society of Anaesthesiology (ASA) Grade I status [13].
Exclusion criteria:
Patients with bilateral high condylar fractures;
Subcondylar fractures;
Patients with extracapsular fractures of the condyle;
Patients with co-morbidities contraindicating closed reduction of condyles (e.g., epilepsy).
Sample size calculation: The sample size is calculated as follows:
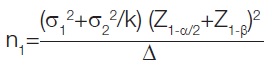
Mean Range of Motion (ROM) in group I=43.4
Mean ROM in group II=39.5
σ1=SD of ROM in group I=1.6
σ2=SD of ROM in group II=2.4 [9]
For detecting mean difference of 3.9 i.e., Δ=43.4-39.5=3.9
K=1
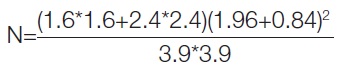
=4.29 ~5 patients/group.
Power of the Test: 80%
Level of significance: 5% (95% confidence interval)
A total of 10 patients will be recruited for present study. They will be randomly divided into two groups: Group A: five patients undergoing closed reduction with arthrocentesis. Group B: five patients undergoing closed reduction without arthrocentesis. Randomisation will utilise an odd-even method.
Study Procedure
A comprehensive case history and thorough clinical examination will be conducted, which includes reviewing the patient’s past medical, dental, and personal history. The TMJ will also be examined. Further radiographic examinations will include a Computed Tomography (CT) scan and an Orthopantomogram (OPG) X-ray. Arthrocentesis will be performed using the single-prick technique [14]. A modified double-lumen single-barrel needle will be used for the arthrocentesis procedure. This needle features a sharp pointed tip with two lumens, and the inlet and outlet bevels face opposite directions. To avoid damaging the needle tip during soldering, it incorporates a 6 mm unsoldered double barrel. The needle also has an entry and exit port for the inflow and outflow of the irrigant. A silicone stopper will be placed approximately 25 mm from the tip to ensure maximum insertion depth during the arthrocentesis procedure. With all precautions taken and following standard surgical protocols, closed reduction will be performed in both groups. Arch bars will be placed on the upper and lower dental arches, securing them to the teeth with 26-gauge wire. The wires will be tightened to achieve proper alignment and immobilisation.
Primary outcomes:
Pain assessment: Pain levels will be assessed both pre- and postoperatively in both groups using the VAS scale, which ranges from 0 (no pain) to 10 (worst pain) [15].
Interincisal mouth opening: For measuring maximal mouth opening, the incisal edges of the upper and lower incisors will serve as reference points. The gap will be measured using a Vernier Caliper for both pre- and postsurgery assessments [16].
Secondary outcomes:
Occlusion classification (stable or unstable): The following scale, devised by the author of present study and available for free use, will be validated after implementation in this protocol:
Stable- No intervention needed (Grade 0);
Mild discrepancy- Elastics required (Grade 1) (Angle’s Class I achieved with guiding force);
Moderate discrepancy- Intermaxillary Fixation (IMF) and occlusal adjustments needed (Grade 2) (Angle’s Class I cannot be achieved even with guiding force);
Severe discrepancy- Requires re-operation (Grade 3) (No occlusal contact).
Bite force measurement: Bite force will be recorded and measured pre- and postoperatively with a BYTE Biteforce Measurement Device [17], which weighs 900 grams and has dimensions of 150×100×70 mm, manufactured by Innovatios Technology in Bengaluru, India.
Statistical Analysis
Statistical evaluations will be conducted using Statistical Package for Social Sciences (SPSS) version 27.0 and GraphPad Prism version 7.0. Both descriptive and inferential statistics will be employed, including the Chi-square test and paired and unpaired Student’s t-tests. These analyses will assess pain, mouth opening, bite force, and occlusion. A p-value of less than 0.05 will be considered statistically significant.
[1]. Singh V, Malkunje L, Mohammad S, Singh N, Dhasmana S, Das SK, The maxillofacial injuries: A studyNatl J Maxillofac Surg 2012 3(2):166-71.10.4103/0975-5950.11137223833492PMC3700151 [Google Scholar] [CrossRef] [PubMed]
[2]. Choi KY, Yang JD, Chung HY, Cho BC, Current concepts in the mandibular condyle fracture management part i: Overview of condylar fractureArch Plast Surg 2012 39(4):291-300.10.5999/aps.2012.39.4.29122872830PMC3408272 [Google Scholar] [CrossRef] [PubMed]
[3]. Kuang SJ, He YQ, Zheng YH, Zhang ZG, Open reduction and internal fixation of mandibular condylar fractures: A national inpatient sample analysis, 2005-2014Medicine (Baltimore) 2019 98(37):e1681410.1097/MD.000000000001681431517812PMC6750236 [Google Scholar] [CrossRef] [PubMed]
[4]. Karan A, Kedarnath NS, Reddy GS, Harish Kumar TVS, Neelima C, Bhavani M, Condylar fractures: Surgical versus conservative managementAnn Maxillofac Surg 2019 9(1):15-22.10.4103/ams.ams_157_1731293925PMC6585226 [Google Scholar] [CrossRef] [PubMed]
[5]. Ellis E 3rd, Walker RV, Treatment of malocclusion and TMJ dysfunction secondary to condylar fracturesCraniomaxillofac Trauma Reconstr 2009 2(1):01-18.10.1055/s-0028-110290022110792PMC3052650 [Google Scholar] [CrossRef] [PubMed]
[6]. Henein P, Ziccardi VB, Temporomandibular disorders: Surgical implications and managementDent Clin North Am 2023 67(2):349-65.10.1016/j.cden.2022.12.00236965936 [Google Scholar] [CrossRef] [PubMed]
[7]. Nitzan DW, Samson B, Better H, Long-term outcome of arthrocentesis for sudden-onset, persistent, severe closed lock of the temporomandibular jointJ Oral Maxillofac Surg Off J Am Assoc Oral Maxillofac Surg 1997 55(2):151-57.discussion 157-5810.1016/S0278-2391(97)90233-09024352 [Google Scholar] [CrossRef] [PubMed]
[8]. Kondoh T, Hamada Y, Kamei K, Kobayakawa M, Horie A, Iino M, Comparative study of intra-articular irrigation and corticosteroid injection versus closed reduction with intermaxillary fixation for the management of mandibular condyle fracturesOral Surg Oral Med Oral Pathol Oral Radiol Endodontology 2004 98(6):651-56.10.1016/j.tripleo.2004.03.02415583535 [Google Scholar] [CrossRef] [PubMed]
[9]. Nogami S, Yamauchi K, Kataoka Y, Takano H, Yamashita Y, Takahashi T, Clinical comparison between arthrocentesis and conventional conservative treatment with maxillomandibular fixation for unilateral high condylar fracturesJ Oral Rehabil 2014 41(2):141-47.10.1111/joor.1212424372314 [Google Scholar] [CrossRef] [PubMed]
[10]. Tino M, Teixeira M, Novaes D, Santana W de, Junior A da S, Neves G das, Arthrocentesis as adjuvant therapy for conservative treatment of condyle trauma: A case reportInt J Oral Maxillofac Surg 2019 48:4010.1016/j.ijom.2019.03.122 [Google Scholar] [CrossRef]
[11]. Nogami S, Yamauchi K, Izumita K, Kitamura J, Takeda Y, Otake Y, Clinical course of masticatory function recovery following arthrocentesis in patients with unilateral mandibular condyle head fractureJ Cranio-Maxillofac Surg 2022 50(3):225-29.10.1016/j.jcms.2021.12.00534930666 [Google Scholar] [CrossRef] [PubMed]
[12]. Sinbel A, Shaaban A, Shokry M, The efficacy of arthrocentesis on restoring mandibular function in unilateral subcondylar fracture following maxillomandibular fixation (a clinico-radiographic study)Alex Dent J 2015 40(1):51-57.10.21608/adjalexu.2015.58736 [Google Scholar] [CrossRef]
[13]. Irlbeck T, Zwißler B, Bauer A, ASA classification: Transition in the course of time and depiction in the literatureAnaesthesist 2017 66(1):05-10.10.1007/s00101-016-0246-427995282 [Google Scholar] [CrossRef] [PubMed]
[14]. Bhargava D, Thomas S, Moghe S, Pathak P, Pawar P, Temporomandibular joint arthrocentesis using double lumen single barrel needle for acute lock cases: A preliminary summary of findingsActa Scientific Orthopaedics 2018 1(1):17-21. [Google Scholar]
[15]. Conti PC, de Azevedo LR, de Souza NV, Ferreira FV, Pain measurement in TMD patients: Evaluation of precision and sensitivity of different scalesJ Oral Rehabil 2001 28(6):534-39.10.1046/j.1365-2842.2001.00727.x11422679 [Google Scholar] [CrossRef] [PubMed]
[16]. Clinical Methods: The history, physical, and laboratory examinations. 3rd edition. Walker HK, Hall WD, Hurst JW, editors 1990 BostonButterworths [Google Scholar]
[17]. Zaky MM, Fayed NA, Shehab MF, Comparison of biting force when using a combination of one microplate and one miniplate versus two miniplates for fixation of parasymphyseal mandibular fracture: The use of microplates for parasymphyseal mandibular fractureOral Maxillofac Surg 2020 24(1):19-24.10.1007/s10006-019-00810-031713697 [Google Scholar] [CrossRef] [PubMed]