Skull fractures are very common after trauma to the head, accounting for 6% of traumatic brain injuries [1]. Blunt trauma to the head is accountable in the majority of cases [2]. Not all skull fractures warrant the attention of a neurosurgeon; however, complicated skull fractures require special consideration. Among all the complicated skull fractures, skull-base fractures and depressed vault fractures are of particular importance.
Skull base fractures carry the risk of injury to cranial nerves, vascular injuries, and the potential for CSF leaks, manifesting as CSF rhinorrhoea or otorrhoea. Skull vault fractures are associated with cosmetic concerns. In more complicated cases, it is often associated with laceration of the overlying scalp and galea in continuity with the fracture site, as well as underlying dural and brain parenchymal injury, contributing to associated neurological deficits [3].
The leakage of brain matter through the scalp wound, the nose, or the ear itself indicates the presence of a fracture and suggests a definitive brain injury. Such cases require utmost attention from neurosurgeons to avoid complications associated with these types of injuries [4]. Some complications encountered in compound skull fractures include wound infection, sinusitis, meningitis, osteomyelitis, brain abscess, seizure disorders (both immediate and late), and, although rare, brain fungus [4]. The overall well being of the patient depends on the early and prompt management by the neurosurgeon. Hence, special attention and skill are necessary to avoid such complications associated with skull fractures, particularly compound ones [5].
Linear, un-displaced skull fractures do not require any treatment. Similarly, all depressed fractures do not require surgical treatment. Debridement is required only in compound depressed fractures, conventionally indicated if the degree of depression of the fracture equals or exceeds the thickness of the adjacent intact bone, or if there is associated underlying contusion or haematoma that needs to be evacuated [2,6].
The process of debridement involves the removal of comminuted fracture segments, identification of the extent of dural injury along with excision of devitalised dural margins, removal of in-driven bone fragments if any, contusectomy (if associated with underlying contusions), followed by watertight dural closure, closure of the calvarial defect, and finally, tension-free wound closure. The closure of the calvarial defect in the same sitting as debridement requires special consideration due to the significant risk of postoperative infections in these cases (2 to 10%) [4]. So usual protocol is to perform cranioplasty in a separate sitting (secondary cranioplasty) after the debridement. There is no difference in infection rates between single-stage cranioplasty and delayed cranioplasty [7]. The use of titanium mesh in cranioplasty has potential benefits, as they are biologically inert and cost-effective [8].
The objective of present study is to shed light on the management of compound depressed skull fractures, with special emphasis on the results of simultaneous debridement and mesh cranioplasty in the same sitting.
Materials and Methods
This was a retrospective descriptive study conducted at the Department of Neurosurgery in Veer Surendra Sai Institute of Medical Sciences and Research in Burla, Sambalpur, Odisha, India. Case records of patients with compound skull fractures from January 2018 to July 2023, in whom surgical intervention was planned and carried out, were initially retrieved. These records were critically analysed based on various clinical, radiological, and operative parameters, and 98 patients were included in the study.
Inclusion and Exclusion criteria: The inclusion criteria were the presence of a significant depressed skull fracture with or without underlying brain parenchymal injury, as confirmed by Computed Tomography (CT), and admission within 72 hours of injury.
Study Procedure
Patients with a very low Glasgow Coma Scale (GCS) score (<8) [9], loss of scalp tissue, and those with delayed presentation (beyond 72 hours after the incident) were excluded from the study. All selected patients underwent simultaneous debridement followed by titanium mesh cranioplasty in the same surgical session. The surgeries were performed by two neurosurgeons who adhered to the same surgical principles. The demographic characteristics of the patients (such as age, sex, and mode of injury) and the radiologic features (including the site of fracture, sinus involvement, and any associated injuries) were evaluated. Data from a three-month follow-up of the patients were collected and analysed for the incidence of wound infection, CSF leak, implant rejection after cranioplasty, and any other complications. Evidence of infection was assessed clinically through local examination of the wound for any signs of inflammation or discharge, any association with fever by measuring body temperature, complete blood count assessment, and quantitative measurement of C-reactive Protein (CRP).
A good surgical outcome was defined as restoration of the skull contour without infection and with good surgical healing, while a bad surgical outcome was characterised by prosthesis exposure or graft rejection.
Surgical technique and principles: All patients included in the study were given prophylactic antibiotics, specifically piperacillin and tazobactam, along with metronidazole on a Three-times-Daily (TID) basis immediately after admission, continuing until the fifth postoperative day. After thorough scrubbing for 5-10 minutes, the skin flap covering the depressed fracture segment was raised, followed by the removal of all foreign bodies and thorough debridement of devitalised tissues, accompanied by copious irrigation of the wound with hydrogen peroxide and normal saline.
In cases of frontal sinus involvement, mucosa was scooped out, cleaned with a dilute betadine solution, and the sinus was obliterated using a pericranial flap. The standard burr hole technique was employed to identify adjacent normal dura, followed by circumferential craniectomy around the fractured segment for the safe elevation of depressed fragments. The extent of any dural injury was delineated, and dural closures were made with an artificial dural patch graft, followed by titanium mesh cranioplasty. Finally, thorough irrigation of the wound was performed before closure, using copious normal saline to reduce the incidence of postoperative infection. The scalp wound was closed primarily after trimming the margins, if required.
Statistical Analysis
The data collected from patients were checked, entered, and analysed by Microsoft Excel, and the results were presented as percentages.
Results
A total of 98 consecutive patients who underwent immediate single-stage reconstruction with titanium mesh for compound skull fractures were included in present study. The mean age of the patients was 28.48±13.79 years (range, 3.5 to 65 years). The mean GCS score was 13.35 at admission and 14.90 at discharge [Table/Fig-1]. Of the patients, 91 were male and seven were female. The causes of fractures included direct impact in 23 patients (23.46%), falls in 16 patients (16.32%), and traffic accidents in 59 patients (60.20%). The locations of fractures included the frontal bone in 64 patients (65.30%), the parietal bone in 23 patients (23.46%), and mixed fronto/temporal/parietal bone in 11 patients (11.22%). Sinus involvement was observed in 41 patients (41.9%). Dural injury was associated with 69 patients (70.4%), and 21 patients had leaking brain matter through the scalp wound (21.4%). Associated lesions on CT included contusion in 46 patients (46.93%), Acute Subdural Haematoma (ASDH) in 12 patients (12.24%), Epidural Haematoma (EDH) in 7 (7.14%), and mixed pathology (contusion with SDH or EDH) in 33 patients (33.67%).
Baseline demographic, clinical and bio-chemical characteristics.
| Parameters | Minimum | Maximum | Mean±SD | Std. Deviation |
|---|
| Age (years) | 3.5 | 65.0 | 28.48 | 13.79 |
| GCS (Admission) | 10.0 | 15.0 | 13.36 | 1.29 |
| GCS (Discharge) | 12.0 | 15.0 | 14.90 | 0.48 |
| Hospital stay (in days) | 5.0 | 23.0 | 10.72 | 3.39 |
| Duration of antibiotics (in days) | 4.0 | 20.0 | 8.74 | 3.08 |
| TLC (pre-op) (in thousands) | 4300.0 | 17300.0 | 9342.86 | 3215.29 |
| TLC (post-op) (in thousands) | 5400.0 | 22300.0 | 10509.29 | 4204.56 |
| CRP (mg/L) | 1.00 | 15.50 | 3.32 | 3.29 |
All patients underwent titanium mesh cranioplasty. A mesh size of 6×6 cm was utilised in 78 patients, while a mesh size of 10×10 cm was utilised in 20 patients. Retrieved bone fragments were fixed with a miniplate and replaced in the case of a female child. The incidence of postoperative fever was 7.14%, occurring in seven patients. The mean White Blood Cell (WBC) count was 9342.85 preoperatively and 10509.28 after the 7th postoperative day. Three patients developed wound infections with sero-sanguinous discharge from the wound, but only one patient required the removal of the implant after three months of surgery, as a retained foreign body was found underneath the scalp margin upon re-exploration. The incidence of postoperative CSF leak was negligible. Approximately five patients developed CSF leaks, which were managed conservatively with acetazolamide and proper positioning, effectively controlling the leaks. None required secondary closure of the defect, and all improved with conservative treatment. Mesh rejection was not observed in any case.
Overall, a good surgical outcome was achieved in 97 (98.97%), while a poor surgical outcome occurred in 1 (1.03%).
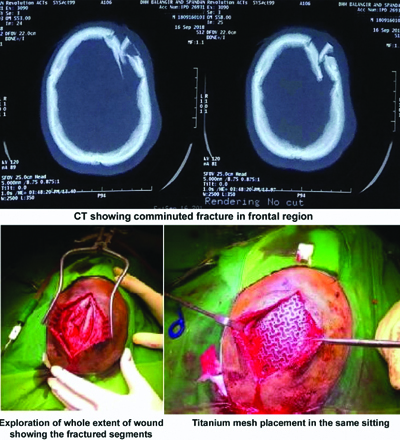
A 12-year-old boy was admitted with a comminuted fracture in the left frontal region [Table/Fig-2a,b]. He underwent surgery under general anaesthesia. After thorough scrubbing and draping, the skin flap covering the depressed fractured segments was raised [Table/Fig-2c]. All foreign bodies were removed, and debridement of devitalised tissues was performed, followed by copious irrigation of the wound with peroxide and normal saline. A titanium mesh [Table/Fig-2d] of appropriate size was placed over the defect and fixed with mini titanium screws. The wound was then irrigated again with copious warm saline, followed by tension-free skin closure. The patient showed an uneventful recovery and was followed-up for three months, which demonstrated good surgical healing without any infection, and his skull contour had been restored.
a,b) CT scan showing comminuted fracture in frontal region; c) Exploration of the whole extent of the wound showing the fractured segments; d) Titanium mesh placement in same sitting.
A 23-year-old male presented with a comminuted fracture of the frontal bone involving the frontal sinus, with GCS of 15/15 and CSF rhinorrhoea. He underwent single-stage debridement, repair of the CSF fistula, and titanium mesh cranioplasty, resulting in a good postoperative recovery [Table/Fig-3a-e].
a) CT scan showing comminuted fracture in left frontal region b) Exposure of the fractured segments c) Completion of debridement d) Bony defect covered with titanium mesh e) Postoperative CT showing mesh covering the defect.

Discussion
In the majority of cases of depressed fractures, the outer table of the fractured segment lies below the inner table [3,5]. At the site of impact, the inner table fractures first and is responsible for the underlying dural injury [3]. In 75 to 90% of cases, the depressed fractures are compound in nature [2]. Previously, the majority of studies [2,6] advocated for cranioplasty as a staged procedure after initial debridement, which is usually performed a few months following the primary procedure. Since, the major concern in the management of compound depressed fractures is infection, most neurosurgical centres perform initial early debridement followed by the closure of the calvarial defect as a secondary procedure.
However, few recent studies [1,2,7,10] have emerged supporting single-stage cranioplasty in patients with compound depressed fractures, with acceptable results regarding the risk of infection and other complications. Eom KS studied 19 patients and reported frontal bone involvement in 57.97%, with sinus involvement in 62.5% [1]. They also reported no complications concerning seizures and wound infections with sinus involvement. The rationale for simultaneous debridement and cranioplasty is multifaceted. It not only avoids subjecting the patient to the usual risks of a second surgery and anaesthetic complications but also benefits the patient in terms of an early return to work, especially in urban areas.
Poorly educated rural individuals from remote areas often lose follow-up once discharged, putting themselves at risk of accidental penetrating injuries through the defect site, which could also be avoided by this single-stage procedure. Another important advantage of the single-stage procedure is its cost-effectiveness compared to two surgeries, which adds an extra burden to people from poor socio-economic backgrounds [11,12].
Jennett B and Miller JD reported on 359 patients with compound depressed fractures, with an infection rate of 10.6%, which is linked to neurological deficits, post-traumatic seizures, and poor outcomes [7]. They also reported that there is no difference in the infection rate when the bone fragments are removed, even in the presence of dural injuries with a conclusion that primary surgery is advantageous [7].
Marbacher S et al., in their small series of five consecutive patients, reported a zero-infection rate with excellent cosmetic results. They concluded that primary reconstruction of open skull fractures with titanium mesh is more feasible, safe, and cosmetically acceptable than the conventional staged approach [10]. Wylen EL et al., retrospectively reviewed case records of 32 patients with compound skull fractures, treated with debridement and elevation of depressed fracture fragments with primary replacement of bone fragments within 72 hours and concluded that there was no increased infection rate after immediate replacement [11].
Jena SP et al., reported that combined bone and titanium mesh cranioplasty is a suitable option for the primary reconstruction of compound skull fractures, positively affecting cerebral metabolism and facilitating patient rehabilitation [12]. Mohapatra AK and Nayak PK in their series of 32 patients subjected to primary fracture reconstruction, concluded that it should be carried out whenever feasible, and titanium implants are cost-effective and a better option than any other alternative measures [8]. Iqbal A et al., concluded that primary reconstruction should be attempted because it is feasible, safe, and cosmetically preferable to the conventional staged approach [13].
In present study, titanium materials were preferred for all adults, sparing children of growing age, where the retrieved bone fragments were utilised for reconstruction using a titanium plate and screws.
Regarding the material, titanium mesh is a suitable alternative to other available materials like Polymethylmethacrylate (PMMA), carbon, Polyetheretherketone (PEEK), hydroxyapatite, ceramics, and osteoconductive bioresorbable materials due to its easy handling, high tensile strength, biological inactivity, very low infection rate, non magnetic and non paramagnetic properties, and excellent biocompatibility. Therefore, titanium is increasingly preferred for the closure of calvarial defects not only in skull fractures but also in other situations where the removal of a portion of the skull is part of the procedure [12,13].
As for the surgical technique, in addition to the standard procedure, authors followed own techniques for proper handling of the surgical site. Firstly, preferred to raise a flap around the fractured segment rather than extending the primary scalp wound for better exposure and generous debridement to expose the full extent of the dual injury. The placement of the mesh is technically easier when the flap is raised. In present technique, in cases of dural injury extending to the skull base, we prefer an onlay patch of dural substitutes in two layers, which yielded better results. The most important aspect of preventing infection was thorough debridement and copious saline irrigation at the end of the procedure.
Limitation(s)
The retrospective nature is an inherent limitation of the study. It was a single-centre study; therefore, the findings cannot be generalised to the entire population. A limited number of patients were included in the study, and the follow-up period was short, so long-term evaluation was not conducted.
Conclusion(s)
Primary reconstruction of depressed compound skull fractures should be attempted whenever feasible. A single-stage procedure benefits the patient in terms of early recovery and also ensures immediate protection for the brain. The titanium implant is a suitable option because of its high biological acceptability and high tensile strength. Regarding infectious complications, the importance of thorough debridement and copious saline irrigation cannot be overemphasised. Moreover, a holistic approach and better-controlled studies are needed to justify this changing trend from a conventional staged procedure to a single-stage one.