The first laparoscopic splenectomy was performed by Delaitre B and Maignien B in 1991. Since then, it has become the method of choice for elective surgery of the spleen [1]. Many studies have reported the advantages of this minimally invasive approach, including less postoperative pain, early recovery, shorter hospital stays and better cosmetic outcomes [2-4]. The introduction of advanced laparoscopic tools has resulted in fewer intraoperative complications. Laparoscopic removal of the spleen, particularly for benign conditions, is aided by morcellation, which allows for extraction through a small incision. The spleen measures approximately 11 cm in the long axis in healthy adults and weighs between 150 to 200 grams [5]. The European Association of Endoscopic Surgeons (EAES) defines splenomegaly as a spleen with a long axis greater than 15 cm and massive splenomegaly as a long axis greater than 20 cm [6]. Laparoscopic splenectomy has become the procedure of choice for mild to moderately enlarged spleens. However, when it comes to laparoscopic splenectomy for massive spleens, the procedure can be more challenging due to the increased size and weight of the organ, reduced working space and difficulty in retrieval. Nevertheless, with appropriate planning and surgical expertise, it is possible to perform laparoscopic splenectomy for massive spleens.
In the present article, the authors share their five-year experience with laparoscopic splenectomy, focusing on the surgical technique and outcomes observed in managing massive spleens.
Materials and Methods
A retrospective descriptive study was conducted in the Department of Surgery, Government Medical College, Srinagar, Jammu and Kashmir, India, from May 2018 to May 2023. The data was collected and analysed in March 2024. A total of 41 patients were included in the study.
Inclusion and Exclusion criteria: Patients aged 18 to 65 years who had undergone elective laparoscopic splenectomies, with no cutoff for spleen size, were included. Patients who were not fit for general anaesthesia, those requiring emergency splenectomy and patients with splenomegaly associated with portal hypertension were excluded from the study.
Study Procedure
Parameters recorded included age, sex of the patients, indications for splenectomy and spleen size. Other parameters recorded were operative time, blood loss, intraoperative adverse events, conversion rate, postoperative complications and length of hospital stay.
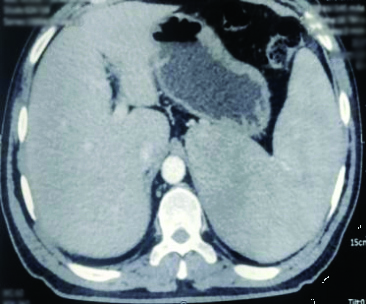
Spleen size was estimated by preoperative imaging studies {ultrasound and Computed Tomography (CT)/Magnetic Resonance Imaging (MRI)} [Table/Fig-1] and during surgery using a marked feeding tube. Operative time was measured from the skin incision for creating pneumoperitoneum to wound closure. Postoperative complications were defined as adverse events occurring within 30 days of surgery. Length of hospital stay was measured from the day of surgery to the day of discharge.
CT showing enlarged spleen.
Surgical technique: After the patient was placed under general anaesthesia, a nasogastric tube was inserted into the stomach to decompress it.
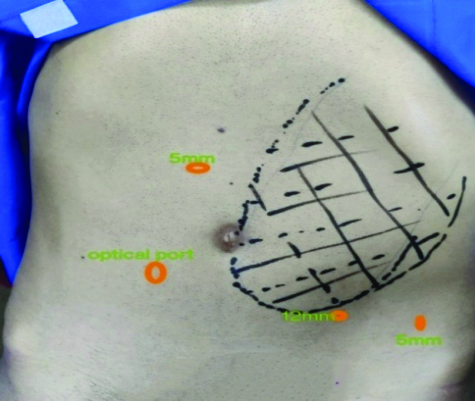
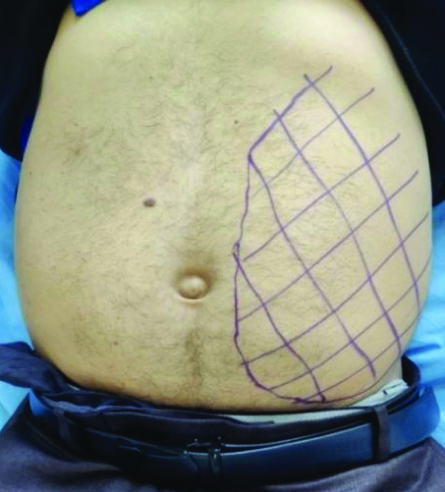
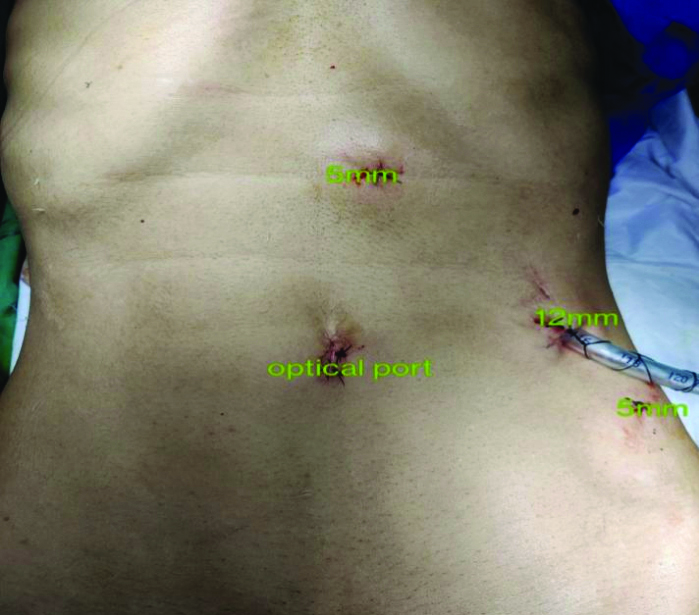
Port placement: The medial and inferior borders of the enlarged spleen were marked. The camera port was placed 5 cm below and to the right of the inferior margin of the spleen [Table/Fig-2,3]. After performing diagnostic laparoscopy, two working ports were introduced on either side of the camera port. The spleen was measured intraoperatively using an infant feeding tube [Table/Fig-4]. A 5 mm accessory port was introduced in the left iliac fossa for the retraction of the spleen.
Preoperative marking of enlarged spleen and port sites.
Preoperative marking of massive spleen.
Intraoperative measurement of spleen by infant feeding tube.
Dissection: Dissection was initiated at the lower pole of the spleen, taking down the splenic flexure of the colon as the first step. The authors continued dissecting the gastrosplenic ligament with a vessel sealer, progressing along to the upper pole of the spleen while ligating all the short gastric vessels, thereby mobilising the stomach from the spleen.
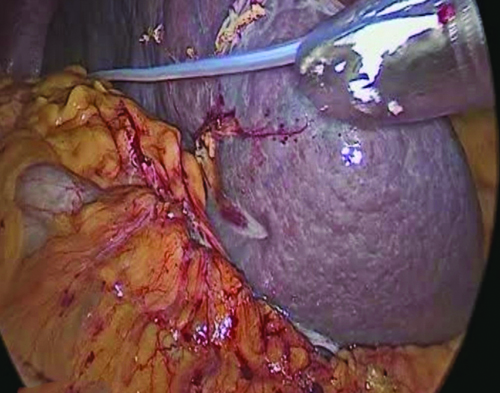
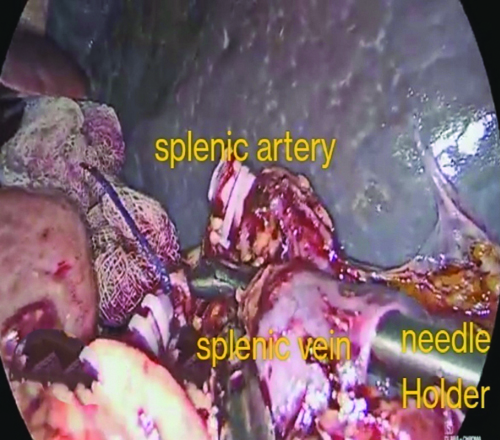
Dissection at splenic hilum: Dissection at the splenic hilum began inferiorly, carefully mobilising the pancreatic tail from the hilum, dissecting the splenic hilum and ligating the splenic artery first. Ligating the artery first causes shrinkage of the spleen and allows for the dissection of the splenic vein, which usually lies behind the artery. Sutures were used for ligating the arteries and vein, especially in the case of massive spleens, as the caliber of these vessels was very large. A laparoscopic needle holder was employed for perivascular dissection, creating a window beneath the vessels by using a rotary motion of the needle holder with its jaws closed [Table/Fig-5]. Following the division of the hilar vessels, the authors dissected the pancreatic tail away from the splenic hilum. Subsequently, they proceeded to release the spleen by dividing its lateral and superior attachments.
Using needle holder for creating window beneath the splenic vein.
Specimen extraction: For benign pathology and small spleens, the authors placed the spleen in a retrieval bag and removed it in pieces through a small incision created by enlarging the 12 mm port. However, when the spleen needed to be removed in one piece for histopathological examination, they made a small subcostal incision for the removal of the spleen in the retrieval bag. Postoperative images of the normal and massive-sized spleen are shown in [Table/Fig-6,7].
Postoperative picture (normal size spleen).
Postoperative picture (massive spleen).

Statistical Analysis
The data was collected from the maintained patient records. The data was compiled and entered into a spreadsheet (Microsoft Excel) and then exported to the data editor of Statistical Package for Social Sciences (SPSS) version 20.0 (SPSS Inc, Chicago, Illinois, USA). Continuous variables were expressed as mean±SD and categorical variables were summarised as frequencies and percentages.
Results
The study group consisted of 20 (48.80%) males and 21 (51.20%) females. The mean age was 43.42±11.28 years [Table/Fig-8]. The most common indication for splenectomy was ITP (n=15), followed by hereditary spherocytosis (n=7) [Table/Fig-9]. The mean spleen size of 26 patients was 12±1.62 cm; in seven patients, it was 17±0.76 cm and in eight patients, it was 23.5±2.29 cm. The largest spleen operated on was 28 cm in size. The mean operative time and average blood loss in patients across the three groups are shown in [Table/Fig-10]. One patient needed conversion to open surgery due to bleeding. The postoperative period for most of the patients was uneventful. Two patients experienced respiratory complications and one patient had a wound infection [Table/Fig-11]. The mean hospital stay for the patients was 3.65±1.21 days [Table/Fig-12].
Distribution of patients according to age and sex.
| Age (years) | Males | Females | Total |
|---|
| n | % | n | % | n | % |
|---|
| ≤20 | 3 | 7.30% | 1 | 2.40% | 4 | 9.70% |
| 21-40 | 6 | 14.63% | 12 | 29.23% | 18 | 43.90% |
| 41-60 | 8 | 19.50% | 7 | 17.07% | 15 | 36.58% |
| ≥60 | 3 | 7.30% | 1 | 2.40% | 4 | 9.70% |
| Total | 20 | 48.80% | 21 | 51.20% | 41 | 100% |
Diagnosis of operated patients.
| Diagnosis | n | % | Average spleen size (SD) |
|---|
| Idiopathic thrombocytopenic purpura | 15 | 36.60% | 11±1.5 cm |
| Hereditary spherocytosis | 7 | 17.06% | 15.21±2.51 cm |
| Splenic lymphoma | 6 | 14.65% | 21.5±1.69 cm |
| Splenic cyst | 5 | 12.22% | 14.5±1.74 cm |
| Chronic lymphocytic lymphoma | 3 | 7.30% | 21±0.82 cm |
| Hypersplenism | 2 | 4.87% | 22.2±0.5 cm |
| Autoimmune haemolytic anaemia | 2 | 4.87% | 12.5±0.5 cm |
| Splenic sarcoid | 1 | 2.43% | 17 cm |
| Total | 41 | 100% | |
Mean operative time and blood loss.
| Spleen size | 10-15 cm | 16-20 cm | >20 cm |
|---|
| Number | 26 | 7 | 8 |
| Mean operative time | 90.5±9.2minutes | 107±12.68 minutes | 155.7±22.5 minutes |
| Mean blood loss | 50.24±8.5 mL | 70.14±11.93 mL | 102.42±88.57 mL |
Intraoperative and postoperative complications.
| Complication | Number |
|---|
| Conversion to open | 1 |
| Pulmonary complications | 2 |
| Post splenectomy bleed | 0 |
| Wound infection | 1 |
| Intra-abdominal abscess | 0 |
| Hospital stay (in days) | n | % |
|---|
| 3 | 26 | 63.45% |
| 4 | 10 | 24.40% |
| 5 | 2 | 4.85% |
| 7 | 2 | 4.85% |
| 8 | 1 | 2.45% |
| Total | 41 | 100% |
Discussion
Since Delaitre B and Maignien B performed the first laparoscopic splenectomy in 1991 [1], this technique has gained popularity over open surgery due to its substantial reduction in morbidity. Laparoscopic splenectomy has become the preferred approach in the elective surgical treatment of normal to moderately enlarged spleens with benign diseases. The outcomes are consistently favourable, solidifying laparoscopic splenectomy as the standard for most elective patients. The advantages, including early recovery, lower postoperative pain, reduced surgical trauma and blood loss, lower complication rates and improved cosmetic results, have made it the method of choice in many centres [7-9]. Initially, laparoscopic splenectomy was reserved for straightforward cases, such as Idiopathic Thrombocytopenic Purpura (ITP) and haemolytic anaemias with normal splenic sizes [10]. However, increased experience has demonstrated its safety even in cases of massive splenomegaly [11,12].
In the present series of 41 patients, 26 patients had spleen sizes in the range of 10-15 cm, seven patients had sizes in the range of 15-20 cm and eight patients had spleen sizes >20 cm. The largest spleen the authors operated on was 28 cm in size. There are three patient positions described for laparoscopic splenectomy in the literature: anterior, hemilateral and lateral. The anterior position was described first [1]. The splenic hilum is well visualised in this position and conversion to open surgery, if required, can be performed easily; however, this position has the disadvantage of moderate visualisation of the ligament structures and vessels. In the lateral position, the patient’s abdomen is vertical to the operating table and as the spleen falls due to gravity, the dissection of ligaments and hilar structures is easier, helping to avoid injury to the pancreas. Several retrospective observational studies, as well as a Randomised Controlled Trial (RCT), have compared the anterior and lateral methods [13-15], showing that the lateral approach was associated with shorter operative times, fewer perioperative and postoperative complications and shorter hospital stays. Meta-analysis of these studies has shown the lateral approach to be superior to the anterior approach in terms of access, intraoperative blood loss, blood transfusion requirements, conversion rates, morbidity and length of hospital stay [16]. We typically performed laparoscopic splenectomy on normal-sized spleens using the lateral position and placed the patient in the right decubitus position at an angle of approximately 90 degrees. This position facilitates the easy division of short gastric vessels and the dissection and ligation of hilar vessels are simpler. It also provides better access to the perisplenic ligaments [17].
However, in cases of massive splenomegaly, the patient was placed in the supine position, with straps and wide cloth tape across the chest and pelvis to allow for minor tilts of the operating table. The stomach was decompressed with a Ryle’s tube and a Foley catheter was placed.
The common indications for laparoscopic splenectomy include benign haematological diseases, with ITP being the most prevalent indication worldwide [18,19]. In the present study, authors also found ITP to be the most common indication for surgery in 36.60% of cases, followed by hereditary spherocytosis in 17.06.
The average operative time and average blood loss for cases involving normal-sized spleens were 90.5±9.2 minutes and 50.24±8.5 mL, respectively, which is consistent with the study by Radkowiak D et al., who reported an average operative time of 100 minutes (75±135 minutes) and average blood loss of 50 mL (20±150 mL) [20]. The mean operative time and average blood loss for cases of massive splenomegaly (size >20 cm) were 155.7±22.5 minutes and 102.42±88.57 mL, respectively, which is comparable to the findings of Tsamalaidze L et al., who reported a mean operative time of 153 minutes (76±328 minutes) and average blood loss of 100 mL (10±400 mL) in their study [21]. One patient with massive splenomegaly (24 cm) required conversion to open surgery during our early experience due to bleeding from an injury to the splenic vein.
The mean duration of hospital stay for our patients was 3.65±1.21 days, which was comparable to other studies [22].
There is some controversy surrounding laparoscopic splenectomy for markedly enlarged spleens and patients with portal hypertension. Somasundaram SK et al., suggest that very large spleens (>27 cm) and portal hypertension can be regarded as relative contraindications to laparoscopy [22]. There are various challenges and limitations in the laparoscopic removal of massive spleens (>20 cm). These challenges include decreased working space, difficulty with retraction and specimen retrieval and the potential for trauma to dilated veins or the splenic capsule, which may result in subsequent bleeding [15,23]. With proper planning and surgical expertise, massive spleens can be removed laparoscopically, as demonstrated by the present study.
Limitation(s)
The present study had certain limitations, as it was a non randomised, single-centre, retrospective study with a limited number of cases and the follow-up of the patients was restricted to the immediate postoperative period only.
Conclusion(s)
Laparoscopic splenectomy is a safe procedure with a low risk of perioperative complications, allowing for early recovery. A successful outcome depends on careful planning and a consistent surgical technique. Experience with the procedure over time suggests that even massive spleens can be removed safely using a minimally invasive approach.