Introduction
Patients with Type 2 Diabetes Mellitus (T2DM) typically require long-term treatment with antidiabetic medications, resulting in a significant financial burden on both the individual and the global economy.
Aim
To assess the patterns of drug utilisation and the economic aspects of antidiabetic medications in individuals with diabetes mellitus.
Materials and Methods
The current study was a hospital-based longitudinal study conducted between October 2017 and September 2019. A total of 132 diagnosed cases of T2DM, aged 18 years and older, who had been on antidiabetic medications in the past three months, were included in the study. Pregnant women and patients in diabetic coma were excluded from the study. A predesigned, pretested, semistructured questionnaire was used to collect data from the patients or their legally accepted relatives. The subjects were followed-up at three and six months to determine any changes in the type and doses of medication. Laboratory parameters such as Fasting Blood Sugar (FBS) and Postprandial Blood Sugar (PPBS) were measured at baseline and at six months, along with a history of any complications of diabetes. The data were analysed using Statistical Package for the Social Sciences (SPSS) version 27.0.
Results
A total of 132 patients were included, of which most patients were male (65.9%), aged 60 years or above (50.8%), illiterate (79.5%), and resided in rural areas (94.7%). The Average Cost-Effectiveness Ratio (ACER) for reducing a unit of FBS was higher compared to PPBS across all forms of the drug. The ACER at three months showed a constant increase, from 24.56 for metformin only to 2709.26 for insulin with Oral Hypoglycaemic Agents (OHA) for FBS, and from 7.83 for metformin only to 907.47 for insulin with OHA for PPBS. Metformin was the most commonly prescribed medication, both as a standalone therapy and in combination therapy.
Conclusion
Present investigation showed that rational prescribing effectively reduced blood sugar readings. Metformin and Glimepiride were the predominant pharmaceuticals utilised for the treatment of diabetes. The cost-effectiveness study indicates that the financial burden of diabetes is substantial, particularly when considering the socio-economic status of individuals.
Introduction
High blood glucose levels characterise a collection of metabolic illnesses known as diabetes mellitus. T2DM is a heterogeneous disorder marked by varying levels of insulin resistance, reduced insulin secretion, and heightened glucose synthesis by the liver [1]. The main cause of diabetes-related morbidity is the long-term consequences of sustained high blood sugar levels, such as microvascular and macrovascular complications. Consistent management of blood glucose levels and treatment of accompanying conditions, including hypertension and dyslipidaemia, can help alleviate these long-term consequences [2].
T2DM is a significant factor in the increasing prevalence of non communicable diseases in both industrialised and developing countries. The International Diabetes Federation Atlas (2017) projects that diabetes affects approximately 451 million individuals aged 18 years and over worldwide, with a projected increase to 693 million by 2045 [3]. Diabetes prevalence in India currently stands at 32.7 million. Projections indicate that this figure will rapidly increase to 124.9 million by 2045 [4]. In 2017, approximately 4.0 million people died worldwide due to diabetes and its complications. The cost of managing diabetes increased from 237 billion USD in 2007 to 727 billion USD in 2017 [3].
Patients with T2DM typically require long-term treatment with antidiabetic medications, resulting in a significant financial burden on both the individual and the global economy. The elderly face health economic challenges and social assistance issues [4]. Older diabetics frequently have co-morbidities that necessitate the use of multiple medications. Moreover, physiological differences in elderly individuals can lead to variations in the absorption, distribution, metabolism, and elimination of medications, as well as their effects on the body. As a result, the elderly often experience inappropriate medicine use, illogical prescribing, Adverse Drug Reactions (ADRs), and non compliance due to economic and health concerns [4]. Therefore, it is essential to address these issues and develop strategies for prescription medication for the elderly.
Rational prescribing ensures that pharmaceuticals are suitable for their specific clinical indications, at the appropriate dosage, for a sufficient duration, and at the most cost-effective price for both the patient and the community. Drug utilisation studies support this. According to the World Health Organisation (WHO), drug utilisation encompasses various aspects of drug management in society, including prescription, dispensing, ingestion, marketing, distribution and usage. It primarily focuses on the subsequent health, societal and economic outcomes. These studies are essential because they encourage us to think critically about new drugs that come to the market, the wide range of prescription and usage patterns for drugs, concerns about delayed ADRs, and how the costs of drugs and therapies are increasing [5,6].
Pharmacoeconomics is a recently developed field of health economics that compares multiple medications, instruments/products, or therapies. It calculates expenses and outcomes related to effectiveness and quality of life. These investigations ensure the scientific and competent utilisation of scarce resources to enhance the effectiveness of healthcare facilities in underdeveloped nations [7,8]. Implementing a cost-effective treatment for diabetes mellitus will not only encourage patients to follow the appropriate prescriptions but also improve patient adherence, resulting in fewer individuals discontinuing treatment due to financial considerations. This, in turn, will lead to reduced diabetes complications and an improved quality of life, thereby enhancing the effectiveness of therapy.
In a study conducted in northern India, the cost per unit reduction in fasting glucose was as low as INR 10.46 for oral antidiabetic medications and as high as INR 217.38 for injectables [9]. Another study from southern India found that the most economical combination therapy was glimepiride and metformin, reporting a percentage cost variation of 5.88% for three-drug combinations and 177.57% for two-drug combinations [10]. The cost variation was highest among the different formulations and combinations of injectable antidiabetics [10,11]. Given the large variation in the study findings, which differ across various geographies within India, present study was designed as a drug utilisation study in diabetic patients who visit our hospital. The primary objective of this study was to assess the patterns of drug utilisation and the economic aspects of antidiabetic medications in individuals with diabetes mellitus.
Materials and Methods
The current study was a longitudinal study conducted between October 2017 and September 2019 (24 months) in the Department of Endocrinology at Maharaja Krushna Chandra Gajapati Medical College and Hospital, Berhampur, Odisha, India. The Institutional Ethics Committee (IEC) approved the study, as documented in letter No. 588/Chairman-IEC, M.K.C.G Medical College, Brahmapur-4. Written informed consent was obtained from each eligible subject before enrollment in the study.
Inclusion criteria: Diagnosed cases of T2DM aged 18 years and older, who had been on antidiabetic medications in the past three months, were included in the study.
Exclusion criteria: Pregnant women and patients in diabetic coma were excluded from the study.
Sample size calculation: According to a previous study by Gnanasegaran S et al., the proportion of patients receiving combination oral antidiabetics was 85.3%. Taking this effect size with an error of 7%, a power of 80%, and an alpha value of 0.05, the sample size was calculated to be 110 [10]. Considering a dropout and missing data rate of 20%, the final sample size was increased to 132. The sample size was calculated using OpenEpi.
The study subjects were recruited and enrolled from the Outpatient Department (OPD) of Endocrinology of the institute. A predesigned, pretested, semistructured questionnaire was used to collect data from the patients or their legally accepted relatives. Five subject experts assessed the content validity of the questionnaire. It was pretested on 15 subjects (10% of the total sample), and necessary modifications were made. The subjects included in the pretesting were excluded from the final analysis. Demographic data, such as age, sex, education, residence, lifestyle and monthly family income, were collected. Information regarding diabetes history, including the duration of the disease, and drug utilisation data, such as type of drug (single/combinations), dose, and routes of administration, were also recorded. Detailed treatment history, including the initiation of antidiabetics and any changes in treatment during the course, was documented. Subjects were followed-up at three and six months to assess changes in the type and doses of medication.
Laboratory parameters, including FBS and PPBS, were measured at baseline and at six months, along with a history of any complications related to diabetes. Drug utilisation data for current therapy were noted according to the WHO-ATC/DDD (World Health Organisation- Anatomic Therapeutic Chemical (ATC) and Defined Daily Dose (DDD) tool [12]. The cost of antidiabetics was calculated using the Odisha State Medical Corporation Limited Drug Procurement List (OSMCL) [13]. The economics of antidiabetics was measured by the ACER, calculated as the ratio of the cost of antidiabetic medications to the unit decrease in FBS and PPBS.
Statistical Analysis
The data were analysed using SPSS version 27.0. Frequencies and percentages were used to describe categorical variables, while mean and Standard Deviation (SD) were used for continuous variables. The comparison of the median of continuous variables at more than two different time points was calculated using the Friedman test, as the distribution of continuous variables was not normally distributed, as assessed by the Shapiro-Wilk test. A p-value <0.05 was considered statistically significant.
Results
A total of 132 diabetic patients were included in the final analysis. Most patients were male (65.9%) and aged 60 years or above (50.8%). The majority of patients were illiterate (79.5%) and resided in rural areas (94.7%). Most had some form of income (96.9%) and engaged in moderate housework (74.2%). The average monthly income of the patients was Rs. 2545.45±1412.13. Co-morbidities were present in 65.9% of the patients, and 48.5% had a duration of diabetes exceeding 18 months [Table/Fig-1].
Socio-demographic and baseline characteristics of the study population (N=132).
| Variables | n (%) |
|---|
| Age (years) |
| <60 | 65 (49.2) |
| ≥60 | 67 (50.8) |
| Gender |
| Male | 87 (65.9) |
| Female | 45 (34.1) |
| Education |
| Illiterate | 105 (79.5) |
| Literate | 27 (21.5) |
| Residency |
| Urban | 7 (5.3) |
| Rural | 125 (94.7) |
| Occupation |
| Employed | 128 (96.9) |
| Dependent | 4 (3.1) |
| Life style |
| Mild/moderate work | 98 (74.2) |
| Sedentary | 34 (25.8) |
| Duration of diabetes |
| ≤18 months | 68 (51.5) |
| >18 months | 64 (48.5) |
| Co-morbidities |
| Present | 87 (65.9) |
| Absent | 45 (34.1) |
Laboratory parameters for diabetes, such as FBS, PPBS, and Glycosylated Haemoglobin (HbA1c), significantly decreased from baseline measurements to those taken at three months and six months (p-value <0.001) [Table/Fig-2].
Laboratory parameters at different time intervals (N=132).
| Parameters | Baseline | 3 months | 6 months | p-value |
|---|
| FBS (mg/dL) | 152.88±18.65 | 131.22±15.53 | 109.42±14.59 | <0.001** |
| PPBS (mg/dL) | 269.64±36.21 | 204.70±34.06 | 135.24±27.95 | <0.001** |
| HbA1c (%) | 8.91±0.84 | 7.36±0.79 | 5.95±0.65 | <0.001** |
**Friedman test was applied; FBS: Fasting blood sugar; PPBS: Postprandial blood sugar; HbA1c: Glycosylated haemoglobin
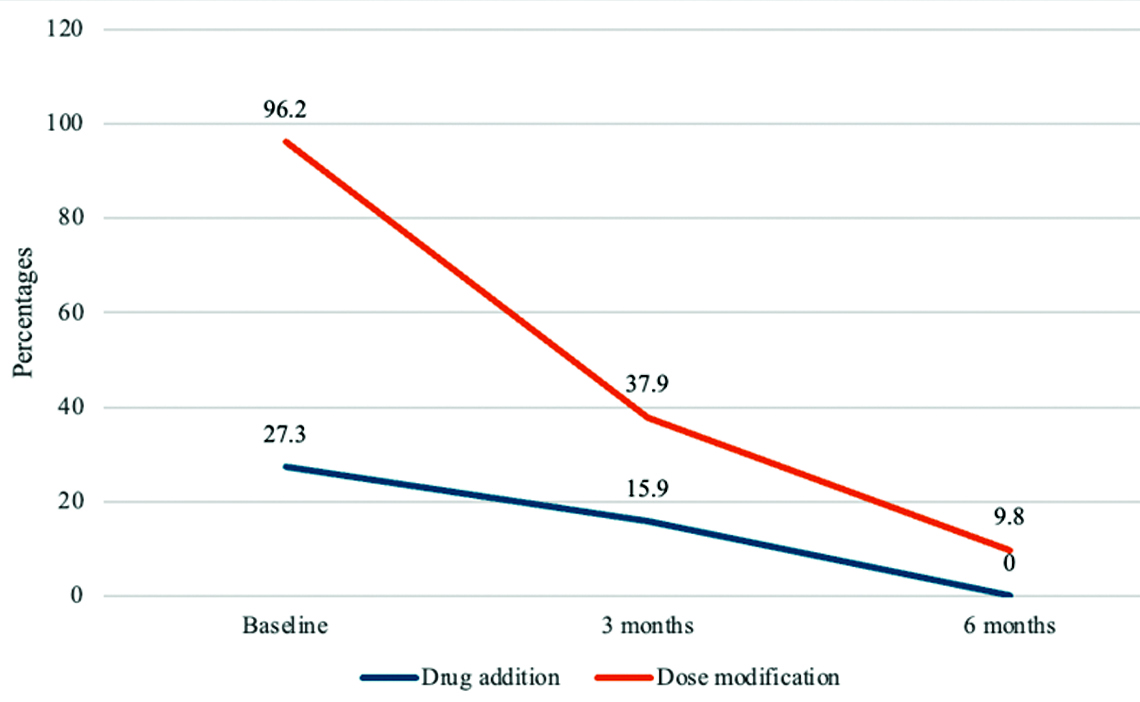
The dose modification was highest at baseline (96.2%), primarily involving an increase in the concurrent medication dose. At the three-month follow-up, the dose modification was 37.9%, which decreased to 9.8% at six months. All dose modifications made at the three- and six-month follow-ups involved increasing the doses of concurrent medications [Table/Fig-3].
Change in medications and dose of medication through time among the study population (N=132).
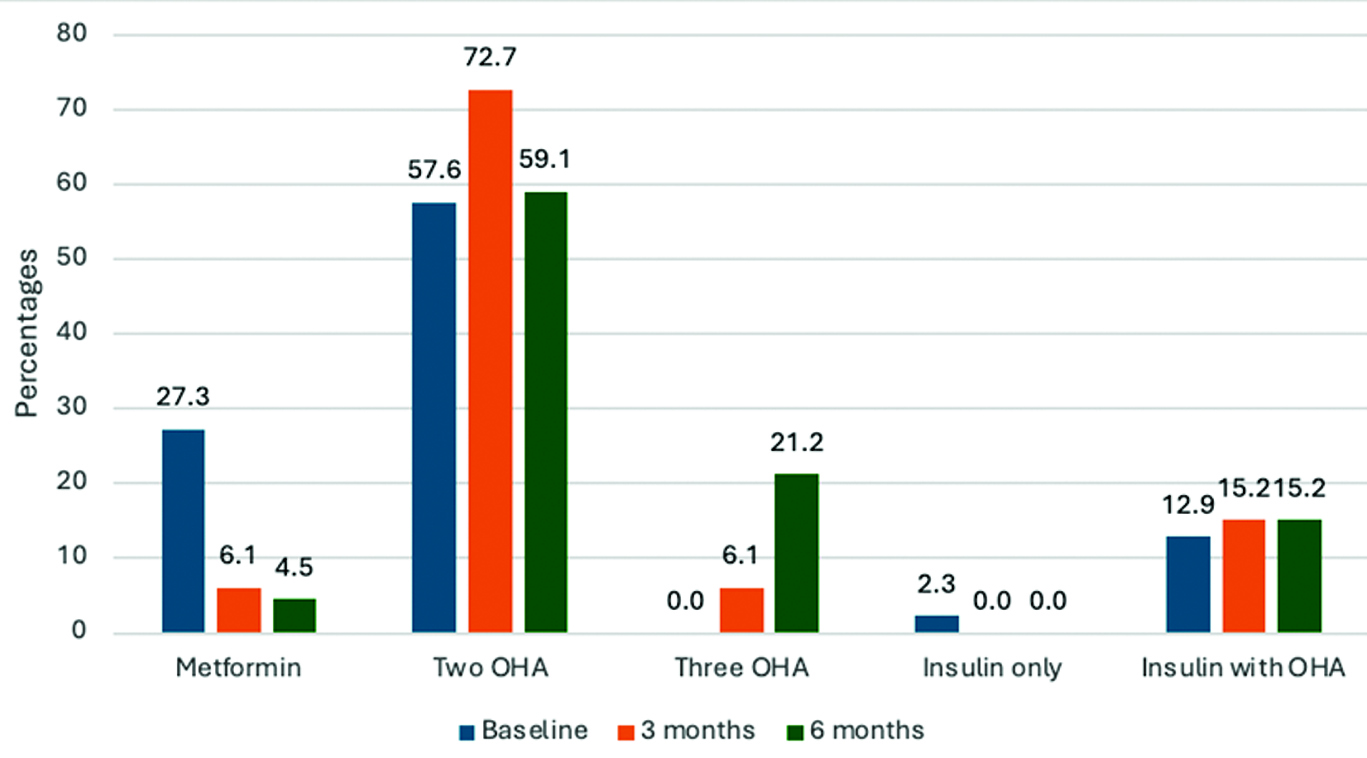
At baseline, 36 (27.3%) of the patients were prescribed only one Oral Hypoglycaemic Agent (OHA), which was metformin; 76 (57.6%) were prescribed metformin with one additional OHA; 17 (12.9%) had insulin with an OHA; and the remaining 3 (2.3%) were prescribed only insulin. The number of patients prescribed two OHAs was highest at the three-month follow-up, at 96 (72.7%), while the proportion slightly decreased to 78 (59.1%) at six months. Eight (6.1%) patients were given three OHAs, which increased to 28 (21.2%) at six months. All subjects who were prescribed only insulin at baseline (3, or 2.3%) were changed to insulin with an OHA at three months (20, or 15.2%) and remained unchanged at six months [Table/Fig-4].
Changes in the type of medication among the study population through time (N=132).
The ACER for reducing a unit of FBS was higher compared to PPBS for all forms of the drug. The ACER at three months showed a constant increase from 24.56 for metformin only to 2709.26 for insulin with OHA for FBS, and from 7.83 for metformin only to 907.47 for insulin with OHA for PPBS. At the six-month mark, metformin only had a better ACER, followed by combinations of three OHAs and two OHAs per unit decrease in FBS and PPBS. Meanwhile, the ACER for insulin with OHA was considerably higher than that of other regimens at six months [Table/Fig-5].
Cost-effective analysis of antidiabetic drugs at different time points.
| Drugs (dose in mg) | N (%) at baseline | ACER at 3 months | ACER at 6 months |
|---|
| FBS | PPBS | FBS | PPBS |
|---|
| Only metformin | 36 (27.3) | 24.56 | 7.83 | 38.61 | 1.60 |
| Metformin and sulfonylurea | 76 (57.6) | 116.97 | 36.34 | 89.10 | 17.34 |
| Three OHA | 0 | - | - | 28.39 | 6.3 |
| Insulin only | 3 (2.3) | 291.84 | 86.12 | - | - |
| Insulin + OHA | 17 (12.9) | 2709.26 | 907.47 | 385.92 | 181.81 |
Discussion
According to the findings of the current study, metformin was the most commonly prescribed medication, both as a standalone treatment and in combination therapy. This finding was consistent with multiple previous research studies [14-16]. The guidelines from the European Association for the Study of Diabetes (EASD) and the American Diabetes Association (ADA) also support the use of metformin as the initial medication for treating T2DM. Metformin is favoured due to its minimal potential for hypoglycaemia, lower chance of weight gain, potential for weight reduction, improved cholesterol levels, and cost-effectiveness [17,18].
The primary approach to treating diabetes in present study (76; 57.6%) and other investigations was combination therapy [19-21]. In contrast to previous studies where monotherapy was used as the primary treatment, the current study demonstrated a different approach [16]. A Fixed Drug Combination (FDC) enhances adherence to treatment protocols and potentially reduces treatment expenses. However, it may also increase the likelihood of experiencing negative medication responses and interactions [22]. The present analysis revealed that the combination of glimepiride and metformin was the most frequently prescribed, which aligns with the most preferred combinations in earlier studies [23,24].
Present study analysis showed a lower prescription rate (15%) for insulins, particularly newer insulins. Similar findings were observed in research conducted by Mathew OJ and Nduka SO and Sutharson L et al., where the prevalence rate was around 10% [25,26]. This was corroborated by the recent ADA guidelines, which advocate for the initiation of insulin therapy (with or without supplementary medications) in individuals newly diagnosed with Type 2 Diabetes (T2D) who have significant symptoms and/or elevated blood glucose levels or HbA1c, or if individuals with T2D are not achieving their desired glycaemic targets with Oral Antidiabetic Drugs (OADs) [18].
Cost-Effectiveness Analysis (CEA) is a widely used method of economic evaluation in medication therapy. It helps identify the cost discrepancies between treatments with comparable outcomes in a specific therapeutic domain. India, known as the global epicenter of diabetes, combined with the chronic nature of the disease, results in a substantial financial burden. The high cost of pharmaceuticals can affect patients’ adherence and lead to a decline in their medical wellbeing and overall quality of life. Reducing the expenses associated with diabetes treatment for patients would significantly impact healthcare expenditures in India.
The primary objective of pharmacoeconomic evaluation is not to directly influence the therapeutic choices made by physicians but rather to assist physicians, pharmacists and policymakers in making well-informed decisions regarding whether the cost and additional benefits of a new drug are significant within the allocated budget [5,6].
This study observed the highest average decrease in blood glucose parameters for PPBS compared to FBS. The findings of present investigation were corroborated by several studies conducted in India [20,27,28]. There was a significant variance in the average cost per unit reduction in FBS (ACER) of recommended antidiabetes medication regimens, ranging from 38.61 to 385.92. This variation was consistent with the findings of a previous study by Acharya KG et al., [20]. In present study, using a single drug called biguanide and a combination of two drugs called sulfonylurea and biguanide were the most cost-effective approaches in reducing FBS and PPBS. These findings align with previous studies [21,28]. The study by Acharya KG et al., found that the combination of sulfonylurea and biguanides was the most cost-effective [20]. Insulin monotherapy is more cost-effective than combining it with OHA, as demonstrated in a study conducted by Abdulganiyu G and Fola T [27].
Limitation(s)
Present study had a few limitations, as the research was carried out in a single-centre, tertiary care set-up, and the results may be applicable only to tertiary care settings. A multicentre study involving all types of healthcare centres may provide a broader perspective.
Conclusion(s)
Present investigation showed that rational prescribing effectively reduces blood sugar levels. Metformin and sulfonylureas were the predominant pharmaceuticals used for the treatment of diabetes. The cost-effectiveness study indicates that the financial burden of diabetes is substantial, especially when considering the socio-economic status of individuals.
**Friedman test was applied; FBS: Fasting blood sugar; PPBS: Postprandial blood sugar; HbA1c: Glycosylated haemoglobin
[1]. Fauci A, Kasper D, Longo D, Braunwald E, Hauser S, Jameson J, Harrison’s Principles of Internal Medicine 2018 20th edNew YorkMcGraw HIll [Google Scholar]
[2]. Goodman L, Gilman A, Brunton L, Lazo J, Parker K, Goodman & Gilman’s the Pharmacological basis of Therapeutics 2022 14th edNew YorkMcGraw Hill [Google Scholar]
[3]. Cho N, Shaw J, Karuranga S, Huang Y, da Rocha Fernandes J, Ohlrogge A, IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045Diabetes Res Clin Pract 2018 138:271-81.Available from: https://doi.org/10.1016/J.DIABRES.2018.02.02310.1016/j.diabres.2018.02.02329496507 [Google Scholar] [CrossRef] [PubMed]
[4]. Zaveri H, Mansuri S, Patel V, Use of potentially inappropriate medicines in elderly: A prospective study in medicine out-patient department of a tertiary care teaching hospitalIndian J Pharmacol 2010 42:95Available from: https://doi.org/10.4103/0253-7613.6449910.4103/0253-7613.6449920711374PMC2907023 [Google Scholar] [CrossRef] [PubMed]
[5]. Shalini S, Ravichandran V, Saraswathi R, Mohanty B, Dhanaraj S, Drug utilization studies – An overviewInt J Pharmaceutical Sci and Nanotechnology 2010 3:803-10.Available from: https://doi.org/10.37285/ijpsn.2010.3.1.210.37285/ijpsn.2010.3.1.2 [Google Scholar] [CrossRef]
[6]. Gama H, Drug utilization studiesArquivos de Medicina 2008 22:69-74. [Google Scholar]
[7]. Fox-Rushby J, Cairns J, Economic Evaluation 2005 1st edMaidenhead, Bershire, EnglandOpen University Press, McGraw-Hill Education [Google Scholar]
[8]. Rai M, Goyal R, Pharmacoeconomics in HealthcarePharmaceutical Med and Translational Clin Res 2017 :465-72.Available from: https://doi.org/10.1016/B978-0-12-802103-3.00034-110.1016/B978-0-12-802103-3.00034-1 [Google Scholar] [CrossRef]
[9]. Singh A, Dutta S, Varma A, Beg M, Kumar H, Kaur A, A drug utilization and pharmacoeconomic study of anti-diabetic drugs prescribed to type 2 diabetes mellitus patients visiting the medicine out-patient department of a tertiary care hospital of north IndiaInt J Basic Clin Pharmacol 2016 :1220-27.Available from: https://doi.org/10.18203/2319-2003.ijbcp2016221910.18203/2319-2003.ijbcp20162219 [Google Scholar] [CrossRef]
[10]. Gnanasegaran S, Gopal S, Murugesan S, Raj GM, Adhimoolam M, Evaluation of pattern of oral hypoglycaemic agents usage and their cost among type-2 diabetic patients in a tertiary care teaching hospitalJ Clin Diagn Res 2019 13(6):FC01-FC05.Available from: https://doi.org/10.7860/JCDR/2019/40807.1288610.7860/JCDR/2019/40807.12886 [Google Scholar] [CrossRef]
[11]. Phulpagare MB, Tiwari SA, Hiray RS, Cost excursion study of various insulin preparations available in IndiaJ Clin Diagn Res 2021 15(7):FC01-FC05.Available from: https://doi.org/10.7860/JCDR/2021/48116.1510710.7860/JCDR/2021/48116.15107 [Google Scholar] [CrossRef]
[12]. WHO Collaborating Centre for Drugs Statistics Methodology. ATC index with DDDs 2000 Oslo, Norway[Internet]. [cited 2024 Oct 15]. Available from: https://www.who.int/tools/atc-ddd-toolkit [Google Scholar]
[13]. Odisha State Medical Cooperation LtdApproved Rates & Firms for Supply of Drugs & Medical Consumables for the Year 2016-17 2017 :01-23. [Google Scholar]
[14]. Agarwal AA, Jadhav PR, Deshmukh YA, Prescribing pattern and efficacy of anti-diabetic drugs in maintaining optimal glycaemic levels in diabetic patientsJ Basic Clin Pharm 2014 5:79Available from: https://doi.org/10.4103/0976-0105.13973110.4103/0976-0105.13973125278671PMC4160724 [Google Scholar] [CrossRef] [PubMed]
[15]. Shah K, Solanki N, Rana D, Acharya K, Evaluation of antidiabetic prescriptions, cost and adherence to treatment guidelines: A prospective, cross-sectional study at a tertiary care teaching hospitalJ Basic Clin Pharm 2013 4:82Available from: https://doi.org/10.4103/0976-0105.12165310.4103/0976-0105.12165324808678PMC3979268 [Google Scholar] [CrossRef] [PubMed]
[16]. Dutta S, Beg MA, Anjoom M, Varma A, Bawa S, Study on drug prescribing pattern in diabetes mellitus patients in a tertiary care teaching hospital at Dehradun, UttarakhandInt J Med Sci Public Health 2014 3:1351-51.Available from: https://doi.org/10.5455/IJMSPH.2014.13082014110.5455/ijmsph.2014.130820141 [Google Scholar] [CrossRef]
[17]. Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Management of hyperglycaemic in type 2 diabetes: A patient-centered approach: Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD)Diabetes Care 2012 35:1364-79.Available from: https://doi.org/10.2337/DC12-041310.2337/dc12-041322517736PMC3357214 [Google Scholar] [CrossRef] [PubMed]
[18]. Elsayed NA, Aleppo G, Aroda VR, Bannuru RR, Brown FM, Bruemmer D, Pharmacologic approaches to glycaemic treatment: Standards of care in diabetes—2023Diabetes Care 2023 46:S140-57.Available from: https://doi.org/10.2337/DC23-S00910.2337/dc23-S00936507650PMC9810476 [Google Scholar] [CrossRef] [PubMed]
[19]. Tanwar S, Acharya A, Hasan N, Assessment of drug utilization pattern of antidiabetic drugs in type-2 diabetes outpatient of a tertiary care teaching hospital western RajasthanInt J Basic Clin Pharmacol 2021 10:368-72.Available from: https://doi.org/10.18203/2319-2003.IJBCP2021101710.18203/2319-2003.ijbcp20211017 [Google Scholar] [CrossRef]
[20]. Acharya KG, Shah KN, Solanki ND, Rana DA, Evaluation of antidiabetic prescriptions, cost and adherence to treatment guidelines: A prospective, cross-sectional study at a tertiary care teaching hospitalJ Basic Clin Pharm 2013 4:82-87.Available from: https://doi.org/10.4103/0976-0105.12165310.4103/0976-0105.12165324808678PMC3979268 [Google Scholar] [CrossRef] [PubMed]
[21]. George N, Ajith KP, Vijayalekshmi AS, Glycaemic control and cost-effectiveness attained by the drug utilization of oral antidiabetic agents in a tertiary care hospital in South IndiaInt J Basic Clin Pharmacol 2016 5:684-91.Available from: https://doi.org/10.18203/2319-2003.IJBCP2016150110.18203/2319-2003.ijbcp20161501 [Google Scholar] [CrossRef]
[22]. Bell D, Combine and conquer: Advantages and disadvantages of fixed-dose combination therapyDiabetes Obes Metab 2013 15:291-300.Available from: https://doi.org/10.1111/DOM.1201510.1111/dom.1201523013323 [Google Scholar] [CrossRef] [PubMed]
[23]. Alex SM, Sreelekshmi B, Smitha S, Jiji K, Menon AS, Devi PU, Drug utilization pattern of antidiabetic drugs among diabetic outpatients in a tertiary care hospitalAsian J Pharmaceutical and Clin Res 2015 8:144-46. [Google Scholar]
[24]. Sahoo J, Mohanty S, Kundu A, Epari V, Medication adherence among patients of type ii diabetes mellitus and its associated risk factors: A cross-sectional study in a tertiary care hospital of eastern IndiaCureus 2022 :14Available from: https://doi.org/10.7759/CUREUS.3307410.7759/cureus.33074 [Google Scholar] [CrossRef]
[25]. Mathew OJ, Nduka SO, Prescribing pattern of antihypertensive and antidiabetic agents in a secondary healthcare institution in NigeriaJ Pharmaceutical Sci Res 2013 5:12-17. [Google Scholar]
[26]. Sutharson L, Hariharan R, Vamsadhara C, Drug utilization study in diabetology outpatient setting of a tertiary hospitalIndian J Pharmacol 2003 35:237-40. [Google Scholar]
[27]. Abdulganiyu G, Fola T, Cost-effectiveness analysis of anti-diabetic therapy in a University teaching hospitalInt J Pharma Sci Res 2014 5:82-91. [Google Scholar]
[28]. Abdelaziz M, Shobha RH, Ravindranath S, Shaik R, Kasim M, Salam AA, Pharmacoeconomic evaluation of oral-hypoglycaemic agents at hospital in BangaloreIOSR J Pharmacy and Biological Sci (IOSR-JPBS) 2015 10:46-50.Available from: https://doi.org/10.9790/3008-1051465010.9790/3008-10514650 [Google Scholar] [CrossRef]