Radiology is an important field in modern medicine that provides non invasive insights into the human body, facilitating accurate diagnoses and guiding treatment plans. The history of radiology dates back to the discovery of X-rays by Wilhelm Conrad Röntgen in 1895, which revolutionised medical imaging [1]. Over the years, advancements such as Computed Tomography (CT), Magnetic Resonance Imaging (MRI) and ultrasound have made it indispensable in contemporary healthcare. The healthcare sector in Saudi Arabia is recognised as one of the most advanced in the Middle East. Despite the sector’s growth, only 42 radiologists are serving a population of 383,051 in the Northern region of Saudi Arabia, translating to a ratio of one radiologist for every 9,120 individuals [2]. This indicates that relatively few medical graduates are choosing radiology as a specialty, despite its critical role in modern healthcare. Meanwhile, in other regions, such as Ireland, radiology is becoming more popular among medical students, with 27% of them choosing it as a future specialty [3].
The decision-making process regarding specialty choice among medical students is a multifaceted phenomenon influenced by various personal, educational and societal factors [4]. Additionally, a lack of knowledge and the emergence of Artificial Intelligence (AI) have given rise to various misconceptions among medical students. There are also gender disparities, as research indicates that only 1.2% of male and 0.8% of female Saudi medical graduates consider choosing radiology as a specialty, primarily due to a lack of interesting cases (36.5%) and the level of difficulty (33%) [5]. Conversely, another study found that 3.8% of females and 3.3% of males opted for radiology, with a higher Grade Point Average (GPA) (90%) and advice from a doctor (85%) identified as key contributing factors [6]. Other factors influencing the decision-making process include high salary, fewer working hours and flexibility in job practice. Some studies have reported that the lack of direct patient contact and the increasing use of technology are the main reasons for aversion to radiology [7]. There are speculations that AI could replace radiologists, potentially leading to a 50% reduction in medical student interest in this specialty [8]. This concern was also noted by Gong B et al., who reported that one-sixth of medical students, although interested in radiology, did not apply for radiology training due to AI [9]. Another study showed the opposite, indicating that radiologists often choose this field because of the lesser contact with patients [10]. Sindi MA et al., found that 5.2% of residents opted for radiology, primarily due to the good reputation of their training centre (23%) [11]. Students stated they chose radiology because it posed an intellectual challenge, while those who did not choose radiology cited a lack of patient interaction and a saturated job market as their reasons [12].
The existing literature on medical students’ perspectives regarding the choice of radiology as a specialty reveals several significant gaps. There is a lack of focused research on Northern Saudi Arabia that accounts for regional, cultural, economic and educational factors that may influence specialty choices. Although some studies have mentioned gender differences in interest towards radiology, there is insufficient exploration of how cultural norms and societal expectations in Saudi Arabia affect female medical students’ choices [13]. Additionally, there is a gap in understanding how the medical curriculum influences students’ perceptions of radiology. Investigating the role of educational programs and mentorship in shaping interest could inform strategies to promote radiology as a viable specialty [14]. Addressing these gaps could lead to a more comprehensive understanding of the factors influencing medical students’ choices regarding radiology as a specialty in Northern Saudi Arabia, ultimately guiding efforts to enhance recruitment and education in this essential field.
The primary goal of this study was to analyse and identify the key factors that significantly shape the decision-making process of medical students during their clinical years at Northern Border University regarding the selection of their future medical specialty. The aim was to discover ways to make radiology more engaging for medical students, thereby encouraging them to consider it as a potential field of specialisation in their future careers.
Materials and Methods
This was a cross-sectional study conducted at the College of Medicine, Northern Border University, Arar, Kingdom of Saudi Arabia (KSA), from June to August 2024, after obtaining approval from the Local Committee of Bioethics (67/24/H).
Informed consent was obtained and a convenience sampling technique was applied to select the study population.
Inclusion criteria: Medical students both male and female, in their clinical years (i.e., 4th, 5th, and 6th years) at the College of Medicine at Northern Border University in KSA were included in this study.
Exclsuion criteria: MBBS students in their first, second and third years from other colleges and students who did not give consent were excluded from this study.
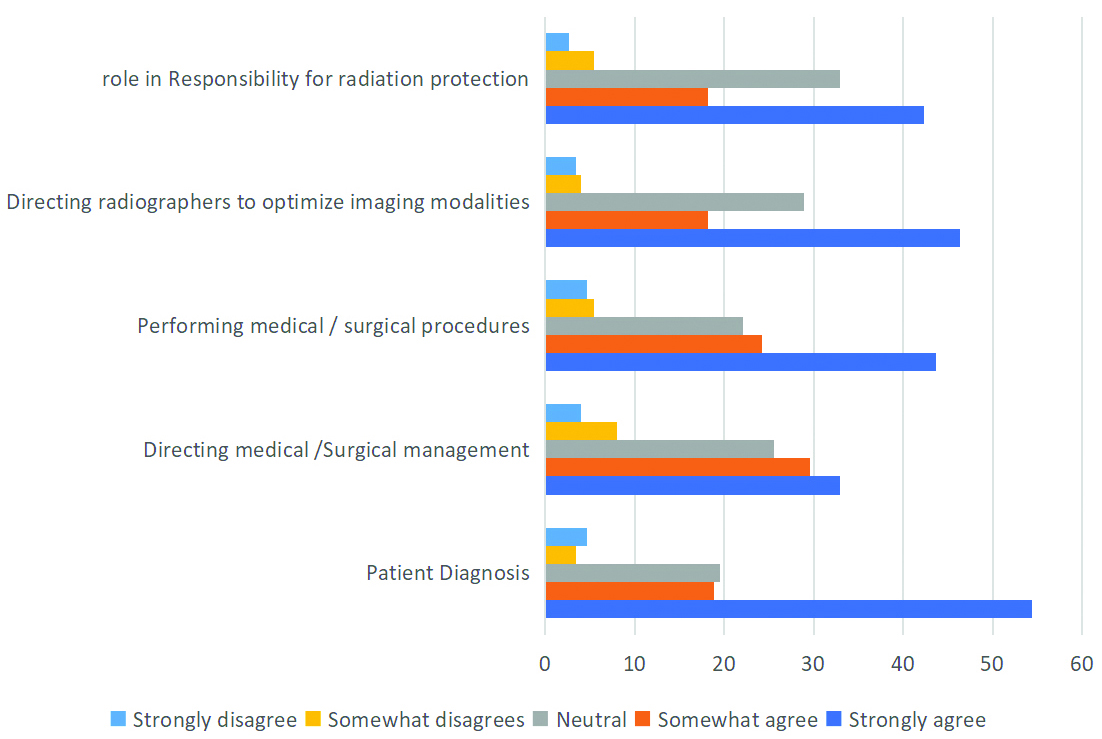
Sample size: The sample size was 149 participants, calculated using the formula:
at a 90% confidence level, with a 6% margin of error and an expected percentage for interest in radiology set at 27% [3].
Study Procedure
A questionnaire taken from a previous study was modified by an assistant professor/consultant radiologist and reviewed by a community medicine specialist to ensure the validity of the items, ensuring relevance and clarity [3]. A pilot study with a sample of 30 participants was then conducted and the face validity was analysed. The questionnaire was converted to an online Google Form and distributed to 155 students via WhatsApp, with 149 responses collected. All questions were analysed separately. Demographic data, including age and gender, were also collected.
Statistical Analysis
All the data were entered into SPSS Software version 22.0 and analysed. The normality of the data was checked using the Shapiro-Wilk test. Qualitative variables were presented as frequencies and percentages, while quantitative variables were presented as means with standard deviations. A p-value of ≤0.05 was considered statistically significant. Confounders such as age, gender and year of study were controlled for using stratification.
Results
The study included 149 participants, with a gender distribution of 56 males (37.58%) and 93 females (62.42%), indicating a higher proportion of females. The age distribution revealed that 61 participants (40.94%) were aged 18-21 years, while 88 participants (59.06%) were aged 22-25 years. No participants were in the 26-30 or over 30 age categories. In terms of academic year, 68 participants (45.64%) were in their 4th year, 43 (28.86%) were in their 5th year and 38 (25.5%) were in their 6th year, showcasing broad representation across different study years. Among the participants, 61 (40.94%) expressed interest in the medical field, 39 (26.17%) in surgery and 49 (32.89%) in both areas. Regarding interest in a specific specialty, 57 participants (38.26%) confirmed they had a preference, while 20 (13.42%) did not and 72 (48.32%) were uncertain.
The specialties of choice revealed that, 15 participants (10.01%) selected anaesthesia, 13 (8.72%) chose emergency medicine and 20 (13.42%) opted for cardiology. Other notable choices included cardiac surgery (9 participants, 6.04%), radiology (16 participants, 10.74%) and gynaecology and obstetrics (21 participants, 14.09%) [Table/Fig-1].
Demographic characteristics of the study population.
| Variable | n (%) |
|---|
| Gender | Males | 56 (37.58) |
| Females | 93 (62.42) |
| Age (years) | 18-21 | 61 (40.94) |
| 22-25 | 88 (59.06) |
| 26-30 | 0 |
| >30 | 0 |
| Year of study | 4th | 68 (45.64) |
| 5th | 43 (28.86) |
| 6th | 38 (25.5) |
| Field of interest | Medical | 61 (40.94) |
| Surgical | 39 (26.17) |
| Both | 49 (32.89) |
| Interest in particular specialty | Yes | 57 (38.26) |
| No | 20 (13.42) |
| May be | 72 (48.32) |
| Specialty of choice | Anaesthesia | 15 (10.01) |
| Emergency medicine | 13 (8.72) |
| Cardiology | 20 (13.42) |
| Cardiac surgery | 9 (6.04) |
| Radiology | 16 (10.74) |
| Gynaecology and Obstetrics | 21 (14.09) |
| Pulmonology | 7 (4.69) |
| Paediatrics | 23 (15.44) |
| Psychiatry | 6 (4.03) |
| Dermatology | 2 (1.34) |
| Community medicine | 1 (0.67) |
| Ear, Nose and Throat | 4 (2.68) |
| Ophthalmology | 5 (3.36) |
| Endocrinology | 1 (0.67) |
| Neurology | 1 (0.67) |
| Pathology | 2 (1.34) |
| Orthopaedic surgery | 1 (0.67) |
| Plastic surgery | 2 (1.34) |
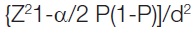
Factors influencing the choice of radiology among participants included academic examination results, with 29 participants (19.46%) reporting a strong influence and 48 (32.21%) reporting a moderate influence. Competition for training strongly influenced 28 participants (18.79%), while patient contact was significant for 43 participants (28.86%), who reported a strong influence. Family expectations impacted 46 participants (30.87%) and income affected 42 (28.19%). Interest in acute patient management was a strong factor for 36 participants (24.16%) and current exposure to the field influenced 35 participants (23.49%). Length of training was a strong influence for 36 participants (24.16%), while work/life balance was critical for 60 participants (40.27%) [Table/Fig-2]. Mentor influence and potential litigation affected decisions for 27 participants (18.12%) and 24 participants (16.11%), respectively. The working environment was notably influential for 54 participants (36.24%). The Chi-square test found no significant association between gender and choice of specialty [Table/Fig-3].
Factor affecting the choice of taking radiology as a specialty (%).
Association between the interest in choosing a speciality and gender.
| Gender | May be | Yes | No | Chi-square statistics | p-value |
|---|
| Female | 50 (44.96±0.57) | 33 (35.58±0.19) | 10 (12.48±0.49) | 3.3272 | 0.18 |
| Male | 22 (27.06±0.95) | 24 (21.42±0.31) | 10 (7.52±0.82) |
[Table/Fig-4] shows that 76 students had exposure to the radiology module and 59 participants stated that modular teaching played a role in their inclination towards radiology. Among the 149 participants, 74 felt that they had “too little” exposure to radiology, while 27 felt that they had “too much” exposure.
Assessment of previous exposure of radiology or radiologist of study population.
| Yes | No | Do not know |
|---|
| Exposure to radiology module | 76 (51.01) | 42 (28.19) | 31 (20.80) |
| Role of Modular teaching in inclination towards radiology | 59 (39.60) | 42 (28.19) | 48 (32.21) |
| Mode of exposure |
| Radiology module | Elective module | Other module | Personal experience |
| Positive exposure | 59 (39.60) | 23 (15.43) | 24 (16.11) | 43 (28.86) |
| Level of exposure |
| How much exposure you think you have to radiology? | Too less | Too much | Medium |
| 74 (49.67) | 27 (18.12) | 48 (32.21) |
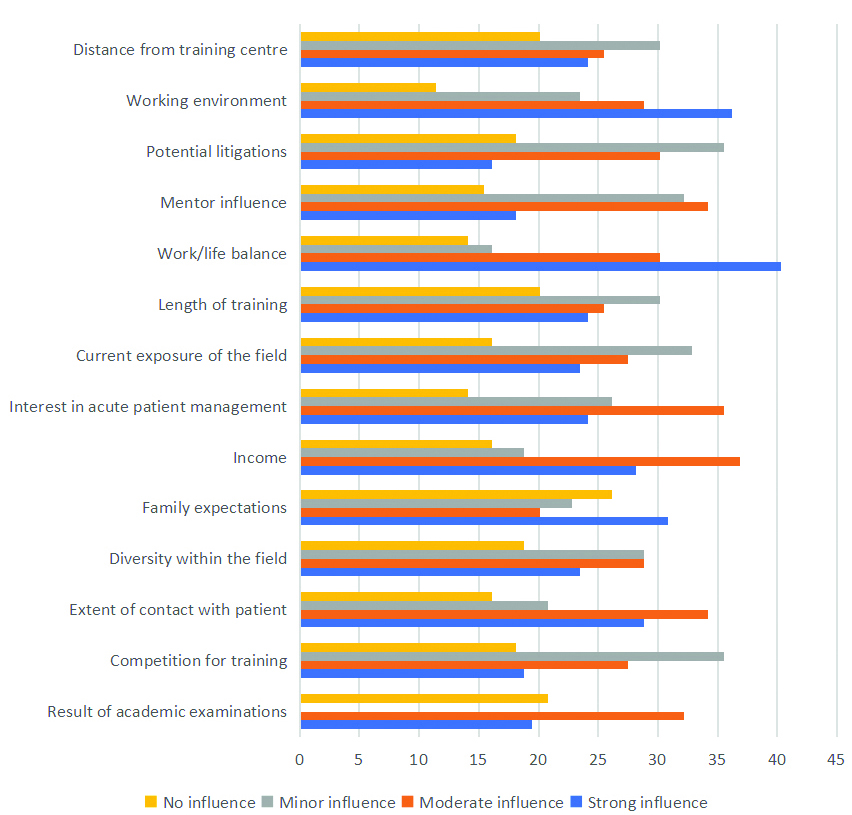
The assessment of medical students’ knowledge regarding the radiologist’s role indicated varying degrees of understanding across key responsibilities. For patient diagnosis, 81 participants (54.36%) strongly agreed and 28 (18.79%) somewhat agreed. In terms of directing medical or surgical management, 49 participants (32.89%) strongly agreed and 44 (29.53%) somewhat agreed. Regarding the performance of medical or surgical procedures, 65 students (43.62%) strongly agreed, with 36 (24.16%) somewhat agreeing. Additionally, 69 participants (46.31%) strongly acknowledged that radiologists direct radiographers in optimising imaging modalities, while 27 (18.12%) somewhat agreed. Concerning radiation protection responsibilities, 64 students (42.28%) strongly agreed and 26 (18.12%) somewhat agreed, underscoring the significance of this role in their understanding of radiology [Table/Fig-5].
Knowledge about role of a radiologist among study population (%).
[Table/Fig-6] shows the factors for not considering radiology as a future specialty, which included the risk of radiation exposure and the high volume of patients as major concerns. A total of 61 students were aware of the difference between a radiologist and a radiographer, whereas 54 were not aware of this difference [Table/Fig-7].
Factors for not considering radiology as a future specialty.
| Strongly agree n (%) | Somewhat agree n (%) | Neutral n (%) | Somewhat disagrees n (%) | Strongly disagree n (%) |
|---|
| Interested but not wanting to do it | 31 (20.8) | 26 (17.5) | 70 (47.0) | 12 (8.1) | 10 (6.7) |
| Lack of appeal for physics and technology | 26 (17.5) | 24 (16.3) | 77 (52.4) | 16 (10.9) | 6 (4.0) |
| Risk of radiation exposure | 42 (28.2%) | 22 (14.8) | 68 (45.6) | 11 (7.4) | 6 (4.0) |
| Minimal patient interaction* | 32 (22.5) | 25 (16.8) | 67 (45.0) | 14 (9.4) | 9 (6.1) |
| Lots of patient interaction | 103 (69.1) | 15 (10.1) | 11 (7.4) | 11 (7.4) | 9 (6.1) |
| Competitive radiology training* | 33 (22.2) | 18 (12.1) | 71 (47.7) | 15 (10.1) | 11 (7.4) |
| Residence is far from specialised centres | 25 (16.8) | 24 (16.1) | 76 (51.0) | 12 (8.1) | 12 (8.1) |
| Radiology encompasses a diverse range of fields | 26 (17.5) | 20 (13.4) | 78 (52.3) | 16 (10.7) | 9 (6.1) |
| Interest in another specialty | 28 (18.8) | 31 (20.8) | 72 (48.3) | 14 (9.4) | 4 (2.7) |
| Peers in radiology | 22 (14.8) | 12 (8.1) | 71 (47.7) | 24 (16.1) | 20 (13.4) |
| Influence of AI | 29 (19.5) | 21 (14.1) | 77 (51.7) | 12 (8.1) | 10 (6.7) |
*Few questions were not answered by all respondents
Awareness about differences between radiology and radiologist along with prospects for choosing radiology as future specialty.
| Yes | 61 (40.94) |
| No | 54 (36.24) |
| Not sure | 34 (22.82) |
Discussion
Radiology is a crucial specialty in modern medicine, as it enables precise imaging of the body’s internal structures, aiding in the early detection and management of various conditions. Radiologists are essential in guiding treatment plans, performing minimally invasive procedures and improving patient outcomes. The specialty’s integration with advanced technologies, such as MRI, CT scans and ultrasound, underscores its importance in providing comprehensive healthcare. Additionally, radiology’s evolving landscape, including the incorporation of AI, continues to enhance its diagnostic capabilities and efficiency.
The findings of this study provide valuable insights into the factors influencing medical students’ decisions to pursue radiology as a specialty in Northern Saudi Arabia. The data suggest that several key elements play a significant role in shaping these decisions, including personal interest in the field, perceived lifestyle benefits and the influence of mentors and role models. The results of this study show that nearly half of the students, 72 (48.32%), are uncertain about their specialty choice, suggesting a need for more exposure and guidance. A significant number, 57 (38.26%), have a clear interest in a particular specialty, while a smaller group, 20 (13.42%), is not interested in any specific specialty. It correlates with the findings of existing literature that indicates more than 49% of students experience doubts and uncertainties about their career choices [14]. Although the present study reports that 76 participants (51.1%) had previous exposure to radiology, 74 (49.64%) believe they do not have enough knowledge about the field. As the teaching module is a major stimulus for inclination towards radiology, with 59 participants (39.59%) acknowledging its influence, further upgrades to enhance understanding of the various disciplines of radiology could streamline the decision-making process for medical students.
Villatoro T et al., have also recommended that early exposure to medical disciplines through simple interventions, such as introductory lectures and simulation exercises, can improve interest, knowledge and motivation [15]. Meanwhile, a significant majority of respondents, 81 (54.36%), strongly agree that radiologists play a crucial role in patient diagnosis, highlighting the importance of radiology in the diagnostic process. Similarly, a combined 131 respondents (62.42%) agree that radiologists are involved in directing medical or surgical management, indicating their integral role in treatment planning. However, despite this important contribution of radiology, the low inclination towards the specialty suggests that multiple factors are influencing the decision-making process of medical students [16]. The data reveals a diverse range of interests among medical students, with a notable inclination towards both medical and surgical fields. Popular specialties include paediatrics, gynaecology and obstetrics and cardiology, while radiology also attracts a fair number of students (16 participants, 10.74%). Efforts to promote less popular specialties could help balance the distribution of future healthcare professionals. Cross-sectional research conducted by Mann-Isah NA et al., on Saudi medical students also revealed that less than 10% of medical students are interested in radiology as their future specialty of choice [17]. The data indicates that various factors significantly influence medical students’ choice of radiology as a specialty. Academic performance is a moderate influence for 48 students (32.21%), while competition for training is a minor concern for 53 (35.57%).
Patient contact (78 participants, 63.08%) and diversity within the field (78 participants, 52.35%) are important, with over half of the students considering them strong and moderate influences. Family expectations (46 participants, 30.87%) and income (42 participants, 28.19%) are also notable factors, reflecting the impact of external pressures and financial considerations. Interest in acute patient management (36 participants, 24.16%) and current exposure to radiology (35 participants, 23.49%) play significant roles, highlighting the importance of practical experience. Work/life balance and the working environment are major influences, underscoring the need for a supportive and balanced professional life. Mentorship and potential litigation are moderate concerns, while the length of training is considered a minor factor. Work-life balance and interest in the subject are regarded as two important factors universally when choosing any subspecialty [18]. To improve students’ interest in radiology, several strategies can be implemented based on the data. Enhancing exposure and education through early and frequent radiology modules, as well as increasing clinical rotations, can provide students with a comprehensive understanding of the field. Establishing robust mentorship programs and highlighting successful radiologists as role models can inspire and guide students [19]. Addressing concerns about AI and job security, as well as radiation safety, can alleviate apprehensions. Promoting the potential for a balanced lifestyle and a positive work environment can attract students seeking work-life balance. Similarly, emphasising the high income potential and offering financial incentives, such as scholarships, can make the specialty more appealing. Educating students about the diverse opportunities within radiology, including subspecialties and research roles, can showcase the breadth of the field [20]. By implementing these strategies, medical schools and radiology departments can foster greater interest in radiology, ensuring a steady influx of passionate and well-informed future radiologists.
Limitation(s)
This study also has certain limitations. The research was limited to medical students in Northern Saudi Arabia, which restricts the generalisability of the findings. Secondly, the study relies on self-reported data, which can be subject to biases such as social desirability bias and recall bias. Students may have provided responses they believe are expected or may not accurately recall their experiences and influences. Longitudinal studies would be beneficial to understand how these factors evolve throughout medical education.
Conclusion(s)
This study identifies key factors influencing medical students’ decisions to pursue radiology in Northern Saudi Arabia, including personal interest, lifestyle benefits and the influence of mentors. Despite students having prior exposure to radiology, nearly half remain uncertain about their specialty choice, highlighting the need for better guidance. Radiology’s critical role in patient diagnosis and management is well recognised, but factors such as academic performance, patient contact, family expectations and income also play significant roles. Work-life balance and a supportive work environment are major influences. To attract more students to radiology, targeted educational initiatives, robust mentorship programs and early exposure are essential. Addressing concerns about AI, radiation safety and competitive training can further support informed career choices.
Authors’ contribution: The corresponding author is solely responsible for carrying out all research work.
*Few questions were not answered by all respondents