Breast Diffuse Large B-cell Lymphoma, Activated B-cell like Subtype: A Case Report
Sneha Samir Babaria1, Jinalben Shaileshbhai Patel2
1 Associate Professor, Department of Pathology, Dr. N. D. Desai Faculty of Medical Science and Research, Dharmsinh Desai University, Nadiad, Gujarat, India.
2 Senior Resident, Department of Pathology, Narendra Modi Medical College, Maninagar, Ahmedabad, Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sneha Samir Babaria, 903, Shyamvrund Appt., Anandnagar Road, Ahmedabad, Gujarat, India.
E-mail: sneha_babaria@yahoo.com
Primary Breast Lymphoma (PBL) is an uncommon form of Non Hodgkin Lymphoma (NHL) that arises within the breast tissue, representing less than 1-2% of all cases of NHL and under 0.5% of all breast cancers. Most PBL cases are of the B-cell type, accounting for up to 50% of all PBL. Diffuse Large B-cell Lymphoma (DLBCL) of the breast is a rare subtype of NHL, with a common age of presentation in females being 50-60 years. It typically presents as a painless breast mass without pathognomonic radiologic findings. Authors hereby, report a case of a 43-year-old female who complained only of heaviness in the right breast, followed by a discretely palpable lump upon examination. High-grade NHL was diagnosed via core needle biopsy and turned out to be DLBCL, Activated B-cell (ABC)-like subtype, as determined by Immunohistochemistry (IHC). This study emphasises that histopathological analysis of core needle biopsy with IHC is paramount for establishing the diagnosis and distinguishing it from other benign and malignant breast conditions. By sharing this case, authors aimed to contribute to the growing knowledge of this rare entity, which has steadily increased over the past four decades, to ensure timely and accurate diagnosis for the implementation of appropriate therapy.
Breast lymphoma, Non hodgkin lymphoma, Primary breast lymphoma
Case Report
A 43-year-old female presented to the breast clinic with a complaint of heaviness in the right side of her breast for five days. On physical examination, a discrete, non tender mass was palpated in the lower central quadrant of the right breast. The mass was firm and mobile. Her temperature, blood pressure, heart rate and respiratory rate were within normal limits. There was no history of tuberculosis, asthma, diabetes mellitus or hypertension. Additionally, there was no family history of breast carcinoma. Laboratory tests were within normal limits.
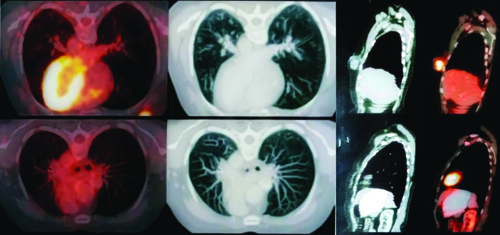
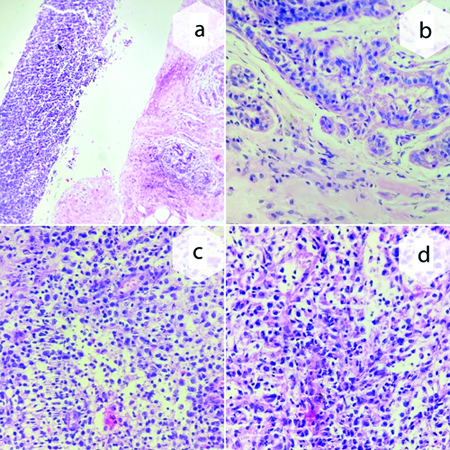
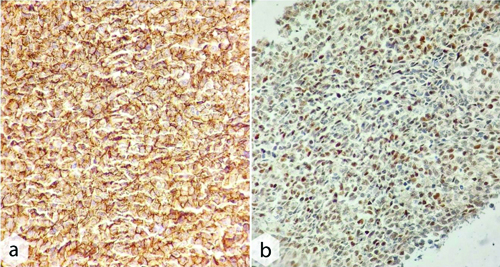
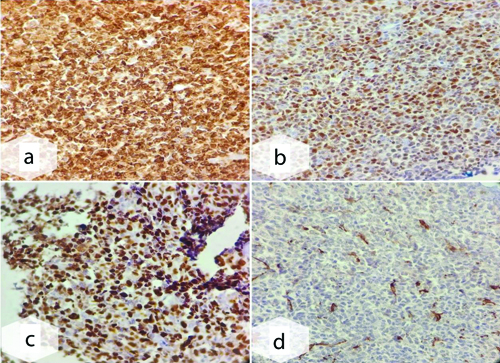
Further evaluation with mammography and ultrasound revealed an irregularly shaped, heterogeneous, non parallel lesion in the lower central segment at 6 o’clock, measuring approximately 3.8×2.2×1.9 cm in diameter. A Breast-Imaging Reporting and Data System (BIRADS) category IV was assigned. No suspicious calcifications or associated lymphadenopathy were noted. A Positron Emission Tomography-Computed Tomography (PET-CT) scan revealed a nodular lesion in the lower central quadrant of the right breast, which appeared lymphomatous. There was no evidence of significantly enlarged right axillary lymph nodes. The left breast and axilla were normal. The upper retroperitoneal lymph node appeared lymphomatous. No evidence of metabolically active disease was seen elsewhere in the body [Table/Fig-1]. Based on the clinical presentation and imaging findings, malignant lymphoma and invasive carcinoma were considered. An Ultrasonography (USG)-guided core needle biopsy of the breast mass was performed. The histopathology results showed diffuse infiltration of large atypical lymphoid cells within the breast tissue. The tumour cells had round to oval nuclei, irregular nuclear membranes, many prominent nucleoli, and vesicular chromatin. High-grade non Hodgkin Lymphoma (NHL) was suggested [Table/Fig-2]. An Immunohistochemistry (IHC) panel for lymphoma was advised for further evaluation. Tumour cells were positive for CD20, C-MYC, BCL-2, Ki-67, and MUM-1, and negative for CD10, CD3, Cyclin D1, and TdT, consistent with a diagnosis of breast lymphoma, DLBCL, ABC-like (by Hans Algorithm) [Table/Fig-3,4]. Bone marrow aspiration and biopsy were performed to rule out infiltration in the bone marrow, which was normocellular with adequate trilineage haematopoiesis, without any infiltration by abnormal cells and marrow fibrosis. Six cycles of combination chemotherapy containing Rituximab, Cyclophosphamide, Adriamycin, and Vincristine were administered, followed by G-CSF injection after each session. Chemotherapy was given, and the patient was followed, but she succumbed within six months.
FDG Positron emission tomography demonstrates Fluorodeoxyglucose (FDG) 2.7×2 cm hypermetabolic mass in the right breast in a lower central quadrant.
Sections showing breast parenchyma diffusely infiltrated by markedly atypical, medium to large-sized lymphoid cells (H&E, a-4x, b,c,d-40x).
Breast Diffuse Large B-Cell Lymphoma (DLBCL) Activated B Cell (ABC) type; (a) CD 20 stain, neoplastic cells are strong, homogenous positive; (b) C-MYC stain, 45% neoplastic cells show overexpression of MYC. (Immunohistochemistry (IHC) stain, a,b, 10X).
Breast Diffuse Large B-Cell Lymphoma (DLBCL) Activated B Cell (ABC) type; (a) BCL 2 stain, positive in >50% neoplastic cells; (b) MUM 1 stain, strongly positive in atypical cells; (c) Ki-67 stain, positive, 90% neoplastic cells showing high proliferation index; (d) CD 10 stain, negative in tumour cells (Immunohistochemistry (IHC) stain, a-d, 10X).
Discussion
The PBL is an uncommon form of NHL that arises within breast tissue. It represents less than 0.5% of all breast cancers and constitutes less than 1-2% of all cases of NHL. PBL is characterised as a malignant primary lymphoma that develops in the breast in the absence of any previously identified lymphoma sites [1]. More than 90% of reported cases are of B-cell origin, with DLBCL being the most common type (above 50%) [2]. It typically presents as a painless breast mass without pathognomonic radiologic findings. Diagnosing it can be challenging due to its rarity and similarities to other benign and malignant breast conditions [3].
A study conducted by Peng F et al., concluded that the overall incidence of PBL has steadily increased over the past four decades [4]. The diagnostic criteria for defining PBL are: the presentation site is the breast, lymphomatous infiltrate is closely related to breast tissue, disseminated disease beyond the ipsilateral axillary lymph nodes is absent and there should be no previously diagnosed lymphoma [5]. Most PBLs are of B-cell type, accounting for up to 50% of all PBL cases [6]. According to a population-based study by Jia Y et al., and a review by James ER et al., DLBCL of the breast is a rare but prevalent subtype of NHL that affects the largest percentage of white individuals (81.3%). The median age of presentation in females is 70 years [2,7]. Additionally, Jia Y et al., observed that 96.4% of the patients were females [7].
On the other hand, the patient in this instance was Asian and younger than the average age. Females generally present with painless breast lumps, swelling, and/or enlarged axillary lymph nodes [7,8]. Findings from this case align with those of previous studies [7,8]. Systemic symptoms like fever and weight loss are less common. Among the subtypes of DLBCL, germinal center B-cell and ABC-like are the more common subtypes that differ in treatment [9]. Treatment of DLBCL generally involves a combination of chemotherapy, radiation therapy and in a few cases, surgery [10]. Normal chemoimmunotherapy (RCHOP) is the treatment for the germinal center B-cell subtype. ABC-like tumours yield poor results with standard therapy, so Lenalidomide, bortezomib, and ibrutinib should be added to the treatment plan [11].
The patient in this case received only standard chemotherapy, which may explain the limited survival. Prognosis is variable based on disease stage and subtype. The treatment response is usually poor, particularly for the ABC-like subtype [10,11]. Despite the young age, the survival of the present case was poor, which was inconsistent with the findings of Jia Y et al., who reported that overall survival was prolonged in younger patients (<70 years old) [7].
This case presented findings from a complaint of heaviness in the right breast in a relatively young female, followed by a discretely palpable lump upon examination. Radiologically, this appeared as an irregular, nodular lesion without calcification, suggestive of lymphomatous involvement. High-grade NHL was diagnosed via core needle biopsy, revealing DLBCL, ABC-like subtype, based on IHC. Despite the absence of metastasis, the prognosis for the patient was poor.
Present case explored the clinical presentation, diagnostic evaluation and management of a patient with breast lymphoma, thereby contributing to the increasing understanding of this rare condition. Authors emphasised the significance of including breast lymphoma in the differential diagnosis when identifying breast masses. This study highlighted the necessity of using core needle biopsy and IHC for an accurate and timely diagnosis, which is crucial for administering appropriate treatment.
Conclusion(s)
It is important to consider breast lymphoma in the differential diagnosis of breast masses, especially in cases where there is a painless palpable mass that mimics breast carcinoma. Mammographically, lymphoma can be suspected, in contrast to invasive carcinoma, as it typically presents as a round to oval tumour with circumscribed or indistinct margins and without calcification. A histopathological study with IHC is paramount for establishing the diagnosis and identifying the lymphoma subtype for treatment planning, as it differs from invasive carcinoma. PBL has a poor prognosis.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Oct 09, 2024
Manual Googling: Dec 03, 2024
iThenticate Software: Dec 14, 2024 (8%)
[1]. Sakhri S, Aloui M, Bouhani M, Bouaziz H, Kamoun S, Slimene M, Primary breast lymphoma: A case series and review of the literatureJ Med Case Rep 2023 17(1):29010.1186/s13256-023-03998-837370180PMC10304384 [Google Scholar] [CrossRef] [PubMed]
[2]. James ER, Miranda RN, Turner SD, Primary Lymphomas of the breast: A reviewJPRAS Open 2022 32:127-43.10.1016/j.jpra.2022.01.00435402679PMC8987598 [Google Scholar] [CrossRef] [PubMed]
[3]. Pereira R, Costa LA, Rosa JE, Duarte I, Locally advanced primary breast lymphoma: A rare case reportEgypt J Radiol Nucl Med 2023 54(1):8610.1186/s43055-023-01034-9 [Google Scholar] [CrossRef]
[4]. Peng F, Li J, Mu S, Cai L, Fan F, Qin Y, Epidemiological features of primary breast lymphoma patients and development of a nomogram to predict survivalThe Breast 2021 57:49-61.10.1016/j.breast.2021.03.00633774459PMC8027901 [Google Scholar] [CrossRef] [PubMed]
[5]. Moura C, Leite MI, Parreira R, Medeiros A, Primary breast lymphomaJ Surgical Case Reports 2020 2020(1):rjz40510.1093/jscr/rjz40531976067PMC6970344 [Google Scholar] [CrossRef] [PubMed]
[6]. Joks M, Myśliwiec K, Lewandowski K, Primary breast lymphoma–a review of the literature and report of three casesArch Med Sci 2011 7(1):27-33.10.5114/aoms.2011.2060022291729 [Google Scholar] [CrossRef] [PubMed]
[7]. Jia Y, Sun C, Liu Z, Wang W, Zhou X, Primary breast diffuse large B-cell lymphoma: A population-based study from 1975 to 2014Oncotarget 2017 9(3):3956-67.10.18632/oncotarget.2328529423097PMC5790514 [Google Scholar] [CrossRef] [PubMed]
[8]. Alkerata A, Al-Janabi MH, Ahmad YI, Jbeili SS, Ahmad IY, Primary breast lymphoma: A rare case reportInt J Sur Case Reports 2024 122:11012010.1016/j.ijscr.2024.11012039098174PMC11359985 [Google Scholar] [CrossRef] [PubMed]
[9]. Tran MG, Cortes G, Choi HW, Young JJ, Tsai IS, Case-based review of breast lymphomasCurrent Radiology Reports 2024 12(5):41-50.10.1007/s40134-024-00425-8 [Google Scholar] [CrossRef]
[10]. Sun Y, Joks M, Xu LM, Chen XL, Qian D, You JQ, Diffuse large B-cell lymphoma of the breast: Prognostic factors and treatment outcomesOnco Targets and Therapy 2016 9:2069-80.10.2147/OTT.S9856627103833PMC4827925 [Google Scholar] [CrossRef] [PubMed]
[11]. Mamgain G, Singh PK, Patra P, Naithani M, Nath UK, Diffuse large B-cell lymphoma and new insights into its pathobiology and implication in treatmentJ Family Med Prim Care 2022 11(8):4151-58.10.4103/jfmpc.jfmpc_2432_2136353039PMC9638643 [Google Scholar] [CrossRef] [PubMed]