Synovial haemangioma is a benign vascular neoplasm that commonly affects the knee joint. It is often underdiagnosed as a cause of chronic knee pain, leading to delays in the management of this rare tumour. Magnetic Resonance Imaging (MRI) and arterial Doppler serve as vital diagnostic modalities that aid in the diagnosis of synovial haemangioma. Here, the authors present a case of a 15-year-old male who had experienced swelling and pain in his left knee joint for the past 13 years without receiving any prior treatment. The patient’s parents reported no history of trauma. Following further investigations, an MRI of the left knee showed evidence of T1 hypointense and T2 moderate Short Tau Inversion Recovery (STIR) hyperintense soft-tissue lesions involving the anterior and posterior recess of the synovium of the knee joint with finger-like projections, which is considered one of the definitive findings of synovial haemangioma. The patient underwent Ultrasound (USG)-guided sclerotherapy using sodium tetradecyl sulfate, after which he experienced rapid relief of his symptoms. Sodium tetradecyl sulfate acts by damaging the endothelium of the feeder vessel, resulting in a thrombus, which later leads to fibrous tissue formation around the feeder vessel. Thus, blood flow is redirected to the healthy veins, resulting in the shrinkage of the haemangioma. The present case report highlights the importance of ultrasound-guided sclerotherapy as a valuable treatment modality in the management of synovial haemangioma.
Case Report
A 15-year-old male presented to the Orthopaedics Outpatient Department (OPD) with complaints of chronic, dull aching pain as well as non progressive swelling in his left knee joint for the past 13 years without receiving any prior treatment. The patient’s parents reported no history of trauma. The patient’s Body Mass Index (BMI) was 19.1 kg/m2, weight was 43 kg and height was 150 cm.
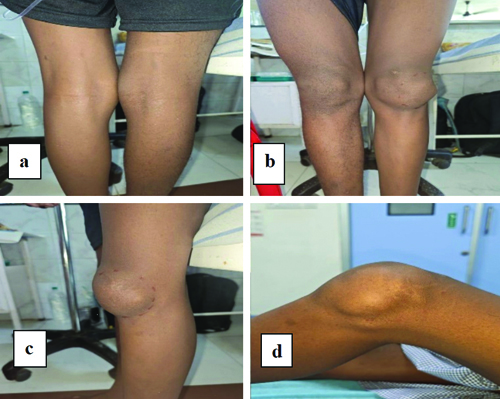
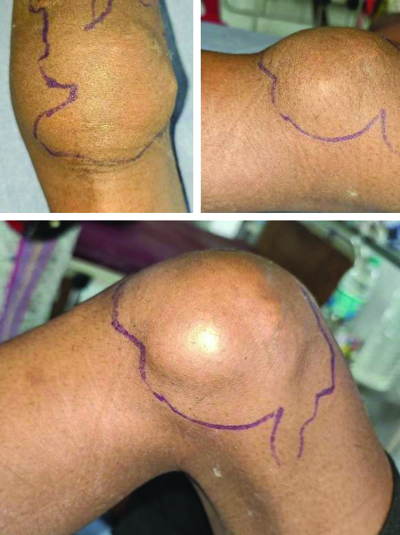
A non tender, soft, palpable 10×7 cm mass was observed on the medial aspect of the left knee during the physical examination. The mass was more prominent during full flexion. No effusion was found in the knee, and there were no signs of instability in the joint. The patient demonstrated normal strength in the lower extremities and had a full range of motion in the knee [Table/Fig-1a-d].
Clinical picture of left knee swelling: a) Posterior aspect of the knee; b) Anterior aspect of the knee; c) Lateral aspect of the knee; d) Knee in flexed position.
On local examination, negative results were noted in both McMurray’s and Apley’s tests. No differences in leg length or presence of cutaneous lesions were observed. The patient’s laboratory test results were within the normal range. The patient’s medical, developmental and family history were unremarkable.
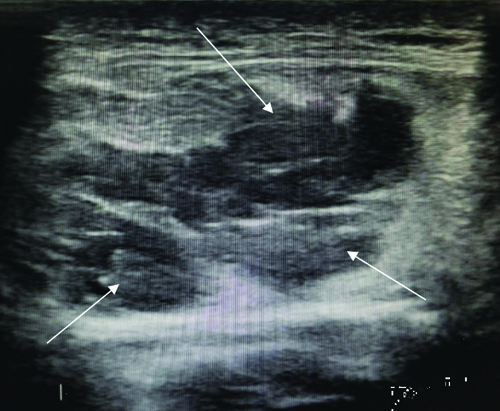
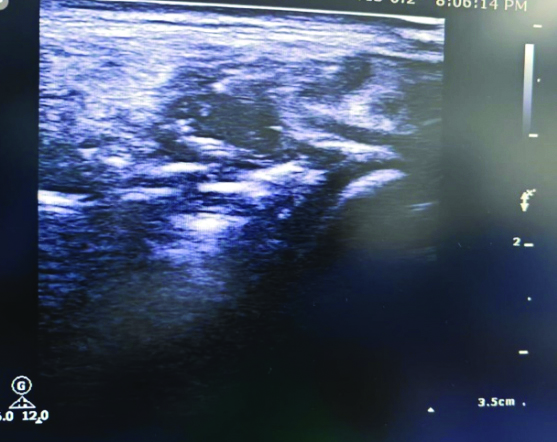
A venous Doppler examination of the left lower limb revealed multiple dilated venous channels in the anterior aspect of the left knee, necessitating further investigation into the underlying etiology [Table/Fig-2]. An arterial Doppler study of the left lower limb showed normal findings.
Venous doppler showing multiple dilated venous channels (white arrows).
A spiral Computed Tomography (CT) angiogram of the lower limbs was obtained using 80 mL of non ionic contrast medium, with multiplanar and volume-rendered reconstructions generated. The examination revealed a distinctly identifiable soft-tissue density lesion measuring 9×7.5×6 cm with a phlebolith, predominantly located on the lateral aspect of the left knee joint. This lesion involved the lateral patellar retinaculum, and extended into the patellofemoral and lateral tibiofemoral joint space and Hoffa’s fat pad. Postcontrast imaging demonstrated delayed lesion enhancement, raising the possibility of a slow-flow vascular malformation, potentially a haemangioma [Table/Fig-3].
CT angiogram showing the soft-tissue density lesion with a phlebolith (white arrows).
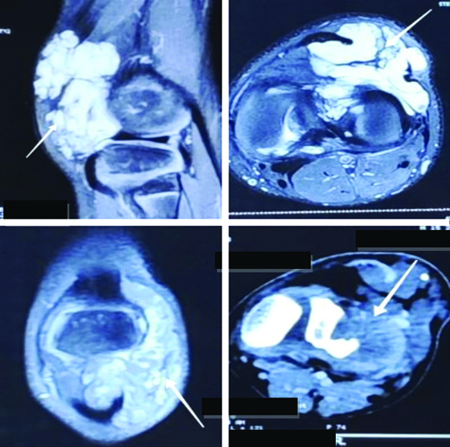
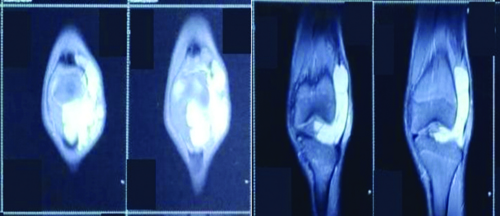
The MRI findings showed evidence of a T1 hypointense and T2 moderately hyperintense soft-tissue lesion, discernible within the anterior and posterior recesses of the synovium of the knee joint, characterised by finger-like projections [Table/Fig-4]. The anterior part of the lateral meniscus exhibited a hyperintense lesion of the same type, which did not affect the joint effusion [Table/Fig-5].
Evidence of T1 hypointense T2 moderate STIR hyperintense soft-tissue lesions involving the anterior and posterior recess of the synovium of the knee joint at finger-like projections.
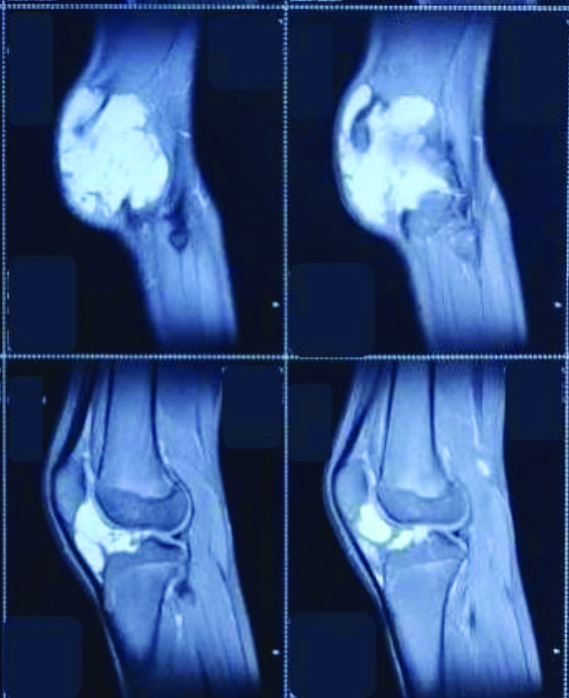
The front part of the lateral meniscus exhibits a hyperintense lesion of the same type, which does not affect the joint effusion.
The patient was initially treated with oral analgesics, ibuprofen 200 mg twice a day and was subsequently scheduled for ultrasound-guided sclerotherapy. Informed consent was obtained from the parents prior to commencing the procedure.
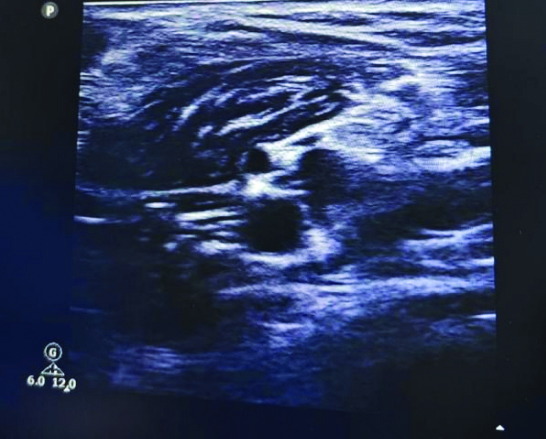
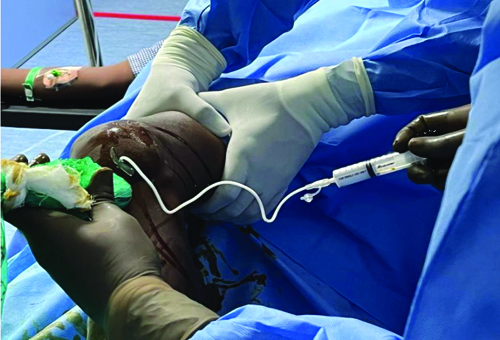
During the surgical intervention, under ultrasound guidance, multiple venous pouches with phleboliths were visualised [Table/Fig-6,7], and each pouch was filled with sodium tetradecyl sulfate using a 24-gauge needle [Table/Fig-8]. After the procedure, the patient’s limb was elevated, and they were given a single dose of Low Molecular Weight Heparin (LMWH) along with limb compression using a crepe bandage. The patient commenced mobilisation on the second postoperative day. A knee brace was applied postoperatively to facilitate early mobilisation. The patient was discharged with a prescribed course of oral anticoagulants, rivaroxaban 10 mg once daily and grade 2 compression stockings.
Multiple venous pouches with phleboliths.
Multiple venous pouches with phleboliths.
Showing USG-guided sclerotherapy.
Three days after the treatment, the patient reported reduced pain and diminished swelling, particularly during knee flexion [Table/Fig-9].
Clinical image of the left knee captured during the follow-up period after sclerotherapy.
Discussion
Synovial haemangioma is a rare, noncancerous vascular abnormality of the synovial membrane, accounting for 1% of all haemangiomas [1]. It commonly affects young adults, particularly in the knee region. Most studies indicate that there is no gender preference; however, several studies have identified females as being more susceptible, while the present case report involved male child [2,3]. Depending on their location, haemangiomas can be classified into three categories: juxta-articular, which are located outside the joint capsule; intra-articular, which are located inside the joint capsule; and intermittent, which are located both inside and outside the joint capsule [3,4].
In children, the diagnosis of synovial haemangioma can be delayed for several years due to its rarity and non specific signs. However, the presence of an associated cutaneous haemangioma can facilitate early diagnosis [5]. Common clinical signs in children include variable symptoms, occasional painful lameness, limited knee movements, recurrent episodes of bleeding within the joint, and muscle weakness [5-7]. Similar symptoms were observed in the present case, with pain and swelling persisting for a long duration that was not resolved by Non Steroidal Anti-inflammatory Drugs (NSAIDs). The case presented with complaints for years, while other studies reported complaints ranging from a few months to years, indicating the delayed diagnosis of synovial haemangiomas [8-10].
Treatment options for synovial haemangioma include open surgical resection, radiotherapy, laser or holmium ablation, sclerosing agents, arthroscopic excision, embolisation, cautery and cryotherapy [8]. Recent studies have highlighted that the combination of arthroscopy with sclerotherapy is efficient in preventing recurrence and achieving good outcomes [Table/Fig-10] [2,4,6,7,10-13]. The authors followed-up with the administration of ultrasound-guided sclerotherapy, which yielded good results during the follow-up [14].
Comparison of the present case findings with similar studies [2,4,6,7,10-13].
| Authors | Age/Gender | Chief complaints | Duration | Physical and local examination | USG/Doppler study | CT angiogram | MRI | Treatment | Outcome |
|---|
| Present study | 15/M | Pain and swelling on left knee | 13 years | Soft, non tender palpable mass prominent during flexion, McMurray and Apley’s tests were negative | Multiple dilated venous channels anterior to the knee, normal arterial study | Soft-tissue density lesion with phlebolith on lateral aspect of knee | T1 hypotense and T2 moderately hyperintense soft-tissue lesion, characterised by finger like projections | USG-guided sclerotherapy | Reduced pain and diminished swelling, particularly during knee flexion in 3 days |
| Zhang H et al., (2023) [2] | 19/M | Pain on right knee | 1 month | Knee joint appeared normal, with no redness, swelling. Tenderness present around the medial aspect of the knee. Pain on hyperextension of knee | N/A | Normal study | T2-weighted MRI revealed a nodular signal shadow | Arthroscopic surgery | Discharged on the third postoperative day and patient was normal during 2nd week follow-up |
| Rishita et al., (2022) [6] | 13/M | Pain aggravated including prolonged walking, standing, squatting, and cross-leg sitting | 10 months | Soft swelling was observed around the anterior aspect of the knee, with the normal range of motion, and no limb length discrepancy and effusion were observed | N/A | N/A | In T1-weighted imaging low to intermediate signals were noted whereas in T2-weighted imaging bright signals were noted | Total synovectomy | Reduced pain and diminished swelling prominence during the follow-up period |
| Kumar I et al., (2024) [7] | 7/M | Pain and swelling on left knee with recurrent effusion | 3 years | A soft, non tender, palpable mass was present and the mass appeared more pronounced on flexion with near normal range of movement | N/A | N/A | Vascular synovial tumour | Open excision with partial synovectomy | At 18 months follow-up, normal limits including no past recurrent effusion |
| Arslan H et al., (2015) [10] | 23/M | Pain and swelling in the knee | 18 months | In the knee mild swelling, on palpation, there was mild pain | Elevated perfusion as well as a solid, hypoechoic, soft-tissue mass | No significant findings | Intra-articular nodular soft-tissue fills the medial suprapatellar bursa, also extending into the vastus medialis | Arthroscopic surgery | Reduced pain and diminished swelling during the followup period |
| Guler I et al., (2015) [12] | 19/M | Swollen and painful knee | N/A | Tenderness and swelling in the anterior knee | N/A | N/A | A large lesion has been filling the suprapatellar bursa. Hyperintense is associated with the muscles along with involving hypointense linear structures inside the center on proton density and T2-weighted fat-saturated images | N/A | N/A |
| Abdulwahab AD et al., (2021) [4] | 21/F | Swelling with increasing pain and tenderness | 6 months | Focal tender swelling including no ulceration, no skin discolouration, and no erythema | Mild joint effusion | N/A | T1-weighted and T1-weighted fat-saturated images, mass was iso intense on T1W1 | Arthroscopic surgery | No proof of any pain, swelling, or restricted joint motion had been found at the follow-up examination |
| Sanghi AK et al., (2015) [11] | 7/F | Not able to walk, as well as, a reduced range of motion | N/A | Node on suprapatellar soft-tissue mass Solid, as well as, lobulated vascular mass in the suprapatellar knee | N/A | Suprapatellar mass demonstrating heterogeneous signal including improvement | Arthroscopic surgery | No evidence of recurrence during the follow-up examination |
| Tohma Y et al., (2019) [13] | 41/M | Painful swelling with a bump | 30 years | Occasional pain during knee moving | Normal study | N/A | Homogeneous with lower intensity on T1-weighted sequences, as well as, igh intensity on T2-weighted sequences | Complete excision | Became asymptomatic after surgery |
Synovial haemangioma can be diagnosed using MRI, angiography, Doppler ultrasonography and arthroscopic techniques [6]. The presence of phleboliths is highly suggestive of synovial haemangioma. Synovial haemangiomas can exhibit non specific signs such as demineralisation, thickening of bone and soft tissues, and early maturation of the physeal plate [7,8]. An iso or hypoechoic mass with venous-type vascularisation and posterior reinforcement in Doppler ultrasonography are suggestive of haemangioma [9,10]. The findings from the Doppler examination showed the presence of multiple dilated veins, indicating vascularisation, which is a specific sign of synovial haemangioma [6].
The MRI has long been the preferred method for diagnosing synovial haemangioma. MRI typically shows a poorly defined mass of variable size, which can be either periarticular or intra-articular. The T1 signal images are iso or hypointense, while T2 images are hyperintense and enhance after gadolinium injection [13]. The images may reveal the presence of fibrous or greasy septations centrally, and the vascular structures may correspond to serpiginous formations within the lesion. Variables such as precise location and extent can be identified using MRI [11,14]. We can isolate and demarcate the feeder vessels, which assists in carrying out preoperative targeted embolisation through arteriography. Selective embolisation can potentially eliminate the need for surgery.
There is some ambiguity surrounding the treatment of synovial haemangioma. Some of the mentioned treatments include arthroscopic excision, open excision of large tumours, sclerotherapy and selective embolisation [12,13]. However, based on the present case patient’s experience, sclerotherapy has proven beneficial with good clinical outcomes.
Conclusion(s)
Synovial hemangioma must be considered when treating patients with persistent knee pain and nonspecific symptoms to avoid delays in diagnosis. MRI is a vital tool in the diagnosis, as it reveals the characteristic lace-like pattern of the hemangioma. Angiography aids in identifying feeder vessels for potential embolisation. Synovial hemangioma should be treated promptly, as it can cause arthropathy through repeated bleeds and may even infiltrate muscle, fat, and bone. This case illustrates the use of sclerotherapy as a management option for synovial hemangioma.
[1]. Diomeda F, Santaniello M, Bracciolini G, Ravelli A, Civino A, Intra-articular venous malformations of the knee: A diagnostic challengePediatr Rheumatol Online J 2021 19(1):15310.1186/s12969-021-00640-z34645460PMC8515759 [Google Scholar] [CrossRef] [PubMed]
[2]. Zhang H, Xu X, Peng Y, Knee joint pain caused by synovial haemangioma: A case reportInt J Surg Case Rep2023110:108737Epub 2023 Aug 2810.1016/j.ijscr.2023.10873737647756PMC10509879 [Google Scholar] [CrossRef] [PubMed]
[3]. Slouma M, Hannech E, Msolli A, Dhahri R, Kouki S, Metoui L, Synovial haemangioma: A rare cause of chronic knee painClin Case Rep 2022 10(7):10.1002/ccr3.6007Available from: https://doi.org/10.1002/ccr3.600710.1002/ccr3.600735846940PMC9272066 [Google Scholar] [CrossRef] [PubMed]
[4]. Abdulwahab AD, Tawfeeq DN, Sultan OM, Intra-articular synovial haemangioma: A rare cause of knee pain and swellingJ Clin Imaging Sci 2021 11:26Available from: https://doi.org/10.25259/jcis_129_202010.25259/JCIS_129_202033948341PMC8088478 [Google Scholar] [CrossRef] [PubMed]
[5]. Shyam K, Andrew D, Johny J, Progressively growing paediatric knee swelling: synovial haemangiomaBMJ Case Rep 2021 14:e242694Available from: https://doi.org/10.1136/bcr-2021-24269410.1136/bcr-2021-24269434551911PMC8461271 [Google Scholar] [CrossRef] [PubMed]
[6]. Rishita , Singh D, Singhvi A, Bharwani N, Jain H, Bhati M, Synovial haemangioma presenting as anterior knee pain- A case seriesJ Orthop Case Rep 2022 12(9):61-64.10.13107/jocr.2022.v12.i09.301836873337PMC9983408 [Google Scholar] [CrossRef] [PubMed]
[7]. Kumar I, Sanchay V, Ahmed W, Kumar S, Bhadani JS, Synovial haemangioma: An overlooked cause of chronic knee pain in childrenJ Orthop Case Rep 2024 14(10):184-87.10.13107/jocr.2024.v14.i10.485639381297PMC11458251 [Google Scholar] [CrossRef] [PubMed]
[8]. Levine BD, Motamedi K, Seeger LL, Synovial tumours and proliferative diseasesRheum Dis Clin North Am 2016 42:753-68.Available from: https://doi.org/10.1016/j.rdc.2016.07.00810.1016/j.rdc.2016.07.00827742025 [Google Scholar] [CrossRef] [PubMed]
[9]. Larbi A, Viala P, Cyteval C, Snene F, Greffier J, Faruch M, Imaging of tumours and tumour-like lesions of the kneeDiagn Interv Imaging 2016 97:767-77.Available from: https://doi.org/10.1016/j.diii.2016.06.00410.1016/j.diii.2016.06.00427397886 [Google Scholar] [CrossRef] [PubMed]
[10]. Arslan H, Islamoğlu N, Akdemir Z, Adanaş C, Synovial haemangioma in the knee: MRI findingsJ Clin Imaging Sci 2015 5:2310.4103/2156-7514.15612925973287PMC4421886 [Google Scholar] [CrossRef] [PubMed]
[11]. Sanghi AK, Ly JQ, McDermott J, Sorge DG, Synovial haemangioma of the knee: A case reportRadiol Case Rep 2015 2(2):33-36.10.2484/rcr.v2i2.6527303458PMC4891626 [Google Scholar] [CrossRef] [PubMed]
[12]. Guler I, Nayman A, Koplay M, Paksoy Y, Synovial haemangioma of the knee joint: magnetic resonance imaging findingsPol J Radiol 2015 80:450-52.10.12659/PJR.89506026491492PMC4596352 [Google Scholar] [CrossRef] [PubMed]
[13]. Tohma Y, Mii Y, Tanaka Y, Undiagnosed synovial haemangioma of the knee: A case reportJ Med Case Rep 2019 13(1):23110.1186/s13256-019-2107-731311579PMC6636119 [Google Scholar] [CrossRef] [PubMed]
[14]. Gopurathingal A, Paul N, Kaganur R, Jirel A, George J, Recurrent intra-articular synovial haemangioma - A case reportJ Orthop Case Rep 2022 12(11):91-94.10.13107/jocr.2022.v12.i11.342837013226PMC10066664 [Google Scholar] [CrossRef] [PubMed]