One of the most detrimental and severe presentations of Systemic Lupus Erythematosus (SLE) is Lupus Nephritis (LN), which is a type of glomerulonephritis. Type-IV Lupus Nephritis, or diffuse Lupus Nephritis, is a severe illness characterised by diffuse proliferative lesions. In this setting, the prognosis worsens if cellular crescent is present. It is divided into two types: diffuse segmental and the other being diffuse global. Wire-loop lesions could also be observed. There have been reports of Collapsing Glomerulopathy (CG) in SLE patients with Focal Segmental Glomerulosclerosis (FSGS). The collapsing variety of FSGS (cFSGS) is defined histopathologically by segmental or global glomerular capillary condensation and obliteration, the appearance of hyperplastic and hypertrophic podocytes, and substantial tubulointerstitial damage. Numerous aetiologies have been proposed, including viral infections such as Human Immunodeficiency Virus (HIV), Cytomegalovirus (CMV), Epstein-Barr virus, and Parvovirus B19, as well as medications and acute ischaemia. Patients infected with Coronavirus Disease-2019 (COVID-19) have an increased risk of acute renal injury as there is a systemic inflammatory cascade due to an acute infection, causing impairment of basic cellular activities in podocytes. Hereby, the authors present a case report of a 17-year-old female who experienced cardiac tamponade and seizures due to Posterior Reversible Encephalopathy Syndrome (PRES). Further investigation and kidney biopsy revealed she had lupus nephritis Stage-IV Diffuse Proliferative Glomerulonephritis (DPGN) but with the collapsing variety, which is a rare finding. Additionally, the patient tested positive for COVID-19, which may have contributed to the development of the collapsing type of DPGN.
Case Report
A 17-year-old female presented to the Emergency Department with gradually progressive dyspnoea {New York Heart Association (NYHA) class II to IV)} and sudden onset of left-sided chest pain lasting for one day. The chest pain rapidly progressed and was accompanied by palpitations. She did not experience orthopnoea or paroxysmal nocturnal dyspnoea. She denied any history of thyroid disorder, hypertension, diabetes mellitus, haemoglobinopathies, haemolytic anaemias, congenital heart diseases, autoimmune disease, or kidney disease.
On general examination, pallor, facial puffiness, and pitting pedal oedema were present [Table/Fig-1]. Other findings such as malar rash, icterus, cyanosis, clubbing, and generalised lymphadenopathy were absent. During the physical examination, the patient was afebrile, with a blood pressure of 90/50 mmHg, a pulse rate of 128/min, and a respiratory rate of 32/minute. Jugular Venous Pressure (JVP) was raised and measured to be 13 cm of water.
Face of the patient showing facial puffiness.

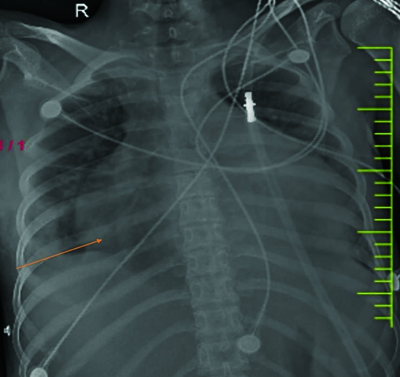
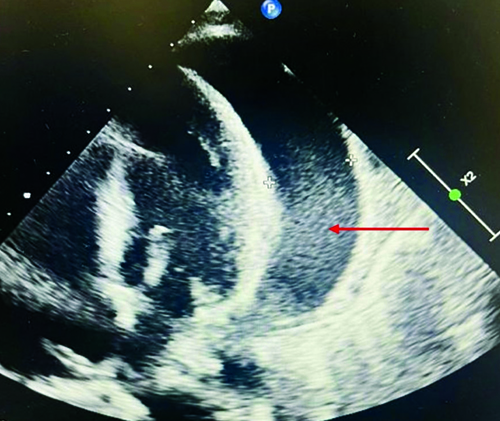
Cardiac examination revealed muffled S1 and S2 sounds. On respiratory system examination, bilateral crackles were observed. The abdomen and central nervous system appeared unremarkable. Due to chest pain and breathlessness, the patient underwent investigations, and a chest X-ray revealed cardiomegaly, as shown in [Table/Fig-2]. A 2D echocardiography was performed, which indicated massive pericardial effusion with a left ventricular Ejection Fraction (EF) of 40%, as shown in [Table/Fig-3]. Emergency pericardiocentesis was immediately performed, and approximately one liter of fluid was aspirated. Following the procedure, the patient experienced a drastic improvement in breathlessness and chest pain, and she reported feeling better.
Chest X-ray Posterior Anterior (PA) view showing cardiomegaly.
A 2D echo showing massive pericardial effusion (red arrow).
Pericardial fluid analysis was conducted, and the examination revealed transudative fluid. As the patient was a young female, Anti-nuclear Antibodies (ANA) titers were tested and found to be 1:1000. Further work-up for SLE was performed, and the patient tested positive for the disease. All laboratory parameters are shown in [Table/Fig-4].
Laboratory parameters of the patient.
| Laboratory investigations | Value in the patient | Biological reference range |
|---|
| Haemoglobin | 7.4 | 13-15 g/dL |
| Total leucocyte count | 7400 | 4000-11000/cumm |
| Platelet | 1,10,000 | 1,50,000-4,50,000/cumm |
| Mean corpuscular volume | 80.5 | 79-100 fL |
| Urea | 28 | 9-20 mg/dL |
| Creatinine | 1.1 | 0.6-1.2 mg/dL |
| Sodium | 132 | 137-145 mmol/L |
| Potassium | 4.3 | 3.5-5.1 mmol/L |
| Alkaline phosphatase | 98 | 38-126 unit/L |
| Alanine transaminase | 12 | <50 U/L |
| Aspartate transaminase | 21 | 17-59 U/L |
| Total protein | 5.6 | 6.3-8.2 gm/dL |
| Albumin | 2.6 | 3.5-5 gm/dL |
| Total bilirubin | 0.7 | 0.2-1.3 mg/dL |
| Globulin | 3 | 2.3-3.5 gm/dL |
| Erythrocyte sedimentation rate | 80 | <15 mm/hr |
| Antinuclear antibody titre | 1:1000 | <1:80 |
| Activated partial thromboplastin clotting time | 30.1 | 29.5 control |
| Prothrombin time | 12.6 | 11.9 control |
| International normalised ratio | 1.16 | 0.8-1.2 |
Urine examination showed 2+ proteinuria and haematuria. On the 5th day of hospital stay, the patient experienced generalised tonic-clonic seizures accompanied by a diffuse headache and blurred vision. This was followed by a loss of consciousness for approximately 20 minutes.
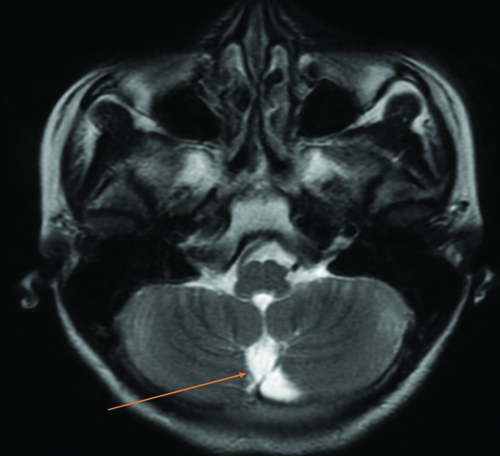
During examination, the patient’s blood pressure was measured at 170/100 mmHg when taken from the right arm in a supine position. Central nervous system examination results were within normal limits. Considering the severe headache and seizure, potential differentials such as cerebrovascular events (infarct or haemorrhage), neurocysticercosis, intracranial space-occupying lesion, and meningoencephalitis were considered. Magnetic Resonance Imaging (MRI) imaging of the brain was performed, revealing PRES on a T2-weighted image, as shown in [Table/Fig-5].
MRI of the brain reveals vasogenic oedema suggestive of Posterior Reversible Encephalopathy Syndrome (PRES) (orange arrow).
Due to the ongoing pandemic and the requirement of Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) testing, COVID-19 RT-PCR was conducted, and the result came back positive. The patient tested negative for HIV, Hepatitis B Virus (HBV), and Hepatitis C Virus (HCV).
The patient underwent further investigation for autoimmune disease. Her immunology profile indicated ds-Deoxyribonucleic Acid (DNA) positivity, strong positive nucleosomes, and positive histones.
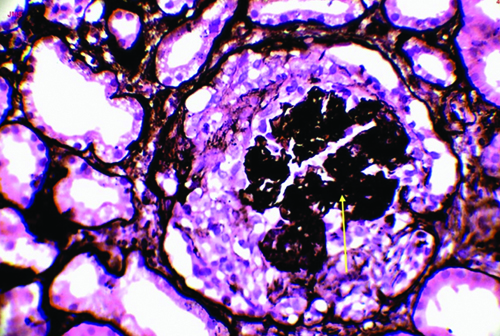
A diagnosis of SLE with multiple system involvement, including the central nervous system, cardiovascular system, and albuminuria, was made. Consequently, a renal biopsy was performed, revealing Class-IV proliferative lupus nephritis with moderate activity, along with a collapsing pattern of glomerular injury and focal vessel changes of lupus vasculopathy/thrombotic microangiopathy. Acute tubular injury with prominent cytoplasmic vacuolations was also observed, as shown in [Table/Fig-6].
Jones methenamine silver showing collapsing pattern of the tuft of the glomerulus (40X) (yellow arrow).
Treatment
The patient received treatment with Injection Methylprednisolone 500 mg once a day for three days, followed by Tablet Prednisolone 60 mg (one tablet) after breakfast in the morning for one month, with a subsequent tapering dose. Additionally, Injection Mannitol 100 mg was administered thrice a day, Injection Levetiracetam 500 mg twice a day, Tablet Telmisartan 40 mg once a day, and Tablet Cyclophosphamide 500 mg once every two weeks for six months. As a result of the treatment, the patient showed clinical improvement. She was followed-up for one month but was then lost to follow-up.
Discussion
Systemic Lupus Erythematosus (SLE) is an autoimmune disease that affects the entire body and can manifest in various ways, impacting nearly every organ [1,2]. Lupus Nephritis (LN) is one of the most significant manifestations, as untreated patients can progress to End-stage Renal Disease (ESRD). It is primarily triggered by a type-3 hypersensitivity reaction, leading to the attachment of anti-dsDNA antibodies to DNA and the formation of anti-dsDNA immunological complexes. These immune complexes deposit in the mesangium, subendothelial, and/or subepithelial regions near the glomerular basement membrane in the kidneys. The development of lupus nephritis initiates an inflammatory response that activates the complement system [3,4].
Type-IV lupus nephritis, also known as diffuse lupus nephritis, is a severe condition characterised by diffuse proliferative lesions. The presence of cellular crescents in this context worsens the prognosis [1]. Lupus Nephritis is divided into two types: diffuse segmental and diffuse global. Wire-loop lesions may be present. Immunofluorescence electron microscopy results indicate immunological deposits in the subendothelial area [2,3]. Collapsing Glomerulopathy (CG) is a specific type of proteinuric kidney disease. Clinically, patients present with acute kidney injury, haematuria, massive proteinuria, and a high-risk of rapidly progressing to permanent kidney failure. CG can be caused by a various factors, including viral infections such as HIV, CMV, Epstein-Barr virus, and parvovirus B19, as well as medications and acute ischaemia. In present case, it was associated with COVID-19 [4,5].
When haematuria, massive proteinuria, acute renal function impairment, and hypertension are present, LN should be considered clinically. Renal biopsy is essential for determining the extent of kidney abnormalities [6-8]. In young female patients presenting with PRES, SLE should be considered in the differential diagnosis. PRES can manifest with various clinical symptoms, including headaches, visual disturbances, seizures, and altered mental status [9,10]. Prompt diagnosis and treatment are crucial in PRES due to its reversible nature. Aggressive treatment, including the use of antihypertensive medications and osmotic agents to reduce cerebral oedema, is necessary to prevent a persistent neurological disability and seizures [11].
While PRES is associated with various disorders, further research is needed to fully understand the underlying pathophysiological mechanisms involved.
The most widely recognised theories focus on the rupture of the blood-brain barrier caused by increased intracranial pressures or endothelial damage [10,11]. Cardiac tamponade is a rare early symptom of SLE. Females are more commonly affected, and common co-existing symptoms include pleuritis, pleural effusion, and haematologic abnormalities [12]. In the differential diagnosis of pericarditis and cardiac tamponade, SLE should be evaluated, and appropriate rheumatologic disease testing should be conducted. In a case report by Abadeer K et al., a clinical case of CG associated with SLE showed a prompt response to mycophenolate and prednisone. The condition in their case started after the sudden discontinuation of an established mycophenolate treatment regimen. The patient presented with acute kidney injury due to biopsy-proven CG, suggesting that mycophenolate may play a role in the prevention and development of CG [13].
Conclusion(s)
The SLE can progress to Type-IV lupus nephritis with CG in the presence of COVID-19. In present case, the patient initially presented with cardiac tamponade, likely due to SLE, during hospital treatment. Additionally, she developed PRES. Further investigation through kidney biopsy revealed Type-IV lupus nephritis with CG, which was attributed to COVID-19. It is crucial to thoroughly evaluate all young females diagnosed with SLE, as it can lead to potentially life-threatening complications such as end-stage renal disease. Early detection and appropriate management are essential to prevent morbidity and mortality.
[1]. Anders HJ, Saxena R, Zhao MH, Parodis I, Salmon JE, Mohan C, Lupus nephritisNat Rev Dis Primers 2020 6(1):710.1038/s41572-019-0141-931974366 [Google Scholar] [CrossRef] [PubMed]
[2]. Muehlig AK, Gies S, Huber TB, Braun F, Collapsing focal segmental glomerulosclerosis in viral infectionsFront Immunol 2022 12:80007410.3389/fimmu.2021.80007435095882PMC8792967 [Google Scholar] [CrossRef] [PubMed]
[3]. Gasparotto M, Gatto M, Binda V, Doria A, Moroni G, Lupus nephritis: Clinical presentations and outcomes in the 21st centuryRheumatology (Oxford) 2020 59(Suppl5):v39-v51.10.1093/rheumatology/keaa38133280015PMC7751166 [Google Scholar] [CrossRef] [PubMed]
[4]. Pesce F, Stea ED, Rossini M, Fiorentino M, Piancone F, Infante B, Glomerulonephritis in AKI: From pathogenesis to therapeutic interventionFront Med (Lausanne) 2021 7:58227210.3389/fmed.2020.58227233738291PMC7960664 [Google Scholar] [CrossRef] [PubMed]
[5]. Emorinken A, Dic-Ijiewere MO, Izirein HO, Cardiac tamponade, an unusual first presentation of systemic lupus erythematosus: A case report in a rural tertiary hospitalCureus 2022 14(8):e2798910.7759/cureus.2798936120196PMC9469684 [Google Scholar] [CrossRef] [PubMed]
[6]. Sudan S, Kaur N, Anand S, Upadhyaya A, Taneja R, Posterior Reversible Encephalopathy Syndrome (PRES) in systemic lupus erythematosus: A rare presentationCureus 2022 14(11):e3137610.7759/cureus.3137636514640PMC9741921 [Google Scholar] [CrossRef] [PubMed]
[7]. Dubey A, Acharya S, Shukla S, Kumar S, Dodeja H, Autoimmune haemolytic anaemia, acute pericarditis with cardiac tamponade as presenting manifestations in systemic lupus erythematosus- A rare case reportJ Clin Diagn Res 2023 17(2):OD01-OD04.10.7860/JCDR/2023/57702.17389 [Google Scholar] [CrossRef]
[8]. Young M, Leslie SW, Renal Biopsy. [Updated 2023 Jul 24]In: StatPearls [Internet] 2025 Jan Treasure Island (FL)StatPearls PublishingAvailable from: https://www.ncbi.nlm.nih.gov/books/NBK470275/ [Google Scholar]
[9]. Hull KL, Adenwalla SF, Topham P, Graham-Brown MP, Indications and considerations for kidney biopsy: An overview of clinical considerations for the non-specialistClin Med (Lond) 2022 22(1):34-40.Epub 2021 Dec 1710.7861/clinmed.2021-047234921054PMC8813013 [Google Scholar] [CrossRef] [PubMed]
[10]. Gewirtz AN, Gao V, Parauda SC, Robbins MS, Posterior reversible encephalopathy syndromeCurr Pain Headache Rep 2021 25(3):1910.1007/s11916-020-00932-133630183PMC7905767 [Google Scholar] [CrossRef] [PubMed]
[11]. Dronamraju S, Gaidhane S, Somani A, Acharya S, Posterior reversible encephalopathy syndrome (PRES) presenting as Status Epilepticus in a case of Autoimmune Hemolytic Anemia (AIHA): A case reportAsian Journal of Medical Sciences 2021 12(6):122-26.10.71152/ajms.v12i6.3590 [Google Scholar] [CrossRef]
[12]. Zhang X, Wu W, Cardiac tamponade as the initial symptom due to systemic lupus erythematosus in a young man: A case reportMedicine (Baltimore) 2018 97(51):e1370810.1097/MD.000000000001370830572500PMC6320037 [Google Scholar] [CrossRef] [PubMed]
[13]. Abadeer K, Alsaad AA, Geiger XJ, Porter IE, Collapsing glomerulopathy in systemic lupus erythematosusBMJ Case Rep 2017 2017:bcr201621784010.1136/bcr-2016-21784028242801PMC5337646 [Google Scholar] [CrossRef] [PubMed]