Scrub typhus is a zoonotic disease caused by Orientiatsutsugamushi. The bacterial infection is spread via Trombiculidae mites. A 50-year-old male patient was admitted with a complaint of fever, cough, breathlessness, and irrelevant talk for five days. The patient was chronic alcoholic and hypertensive for one year. After investigation patient was positive for scrub typhus. The patient had hepatitis, renal failure, thrombocytopenia, and right lower lobe pneumonia. The cause of thrombocytopenia in scrub typhus individuals could be the development of Thrombotic Thrombocytopenic Purpura (TTP), Disseminated Intravascular Coagulation (DIC), and thrombotic microangiopathy. In scrub typhus patients, TTP and Multiple Organ Dysfunction Syndrome (MODS) can be avoided with early diagnosis and effective treatment. Further research is warranted in such conditions to understand the molecular mechanism as well as to prevent mortality.
Bacteria, Hepatitis, Mites, Pneumonia, Renal failure
Case Report
A 50-year-old male patient was brought to the hospital by his son with a complaint of fever, cough, breathlessness, and irrelevant talk since five days. The patient was having the habit of drinking alcohol for three years. The patient was hypertensive for one year and was taking (tab amlo 5 mg/od) for the same while asking questions from the son, the patient was found to have high-grade fever which was associated with chills and rigours, productive cough with yellow expectoration. The patient had been drinking alcohol every day, and the last intake was five days prior to the onset of symptoms. The patient is farmer by profession.
On examination, the patient was conscious, irritable, disoriented, and febrile (102°F), pulse rate of 118 beats/min, regular, blood pressure was 130/80 mm of Hg and with respiratory rate of 30/min. The patient had pallor, icterus, and pitting pedal oedema. On systemic examination, cardiovascular examination- s1s2 heard, respiratory examination- bilateral air entry was present, tubular type of bronchial breathing heard in right axilla and mammary region, inspiratory crepitations were heard in the same region, central nervous system- conscious, irritable, disoriented, flapping tremors present, per abdomen was soft, non tender. Routine blood investigations were done [Table/Fig-1].
Routine blood investigations report.
| Test | Values | Normal values |
|---|
| Hb (g/dL) | 7.4 | 13.8-17.2 |
| WBCs (/cumm) | 2800 | 4000-11000 |
| Platelets (/cumm) | 79,000 | 150,000-400,000 |
| Mean corpuscular volume (fL) | 96 | 80-100 |
| Haematocrit (%) | 22.2 | 40-54 |
| Urea (mg/dL) | 90 | 5-20 |
| Creatinine (mg/dL) | 2.9 | 0.7-0.13 |
| Sodium (mmol/L) | 135 | 135-145 |
| Potassium (mmol/L) | 3.5 | 3.5-5.2 |
| Alkaline phosphatase (U/L) | 148 | 44-147 |
| Alanine transferase (U/L) | 1042 | <50 |
| Aspartate transferase (U/L) | 1500 | 17-59 |
| Albumin (g/dL) | 1.9 | 3.5-5.5 |
| Total bilirubin (g/dL) | 7.4 | 0.1-1.2 |
| Conjugated bilirubin (mg/dL) | 6.3 | <0.3 |
| Unconjugated bilirubin (mg/dL) | 1.1 | 0.2-0.8 |
| Ammonia (mg/dL) | 77 | 9-30 |
| C-reactive protein (mg/L) | 69.689 | 8-10 |
| Lactate dehydrogenase (U/L) | 314 | 140-280 |
| Calcium (meq/L) | 7.8 | 4.3-5.3 |
| Magnesium (meq/L) | 1.5 | 0.85-1.10 |
| Phosphorus (meq/L) | 3.5 | 1.12-1.45 |
| Prothrombin time (seconds) | 16.9 | 11-13.5 |
| Activate partial thromboplastin time (seconds) | 38.7 | 21-35 |
| International normalised ratio | 1.45 | 2.0-3.0 |
A fever profile was sent and it came out positive for scrub typhus IgM. Cerebrospinal Fluid (CSF) analysis was sent which revealed transparent colour fluid, Red Blood Cells (RBC)- 0/High Power Field (HPF), White Blood Cells (WBCs)- 4 cells/cumm, predominantly lymphocytes, adenosine deaminase was 3.531 U/L, glucose- 64 mg/dL, LDH- 70 U/L, protein- 45 mg/dL, pH- 7.2.
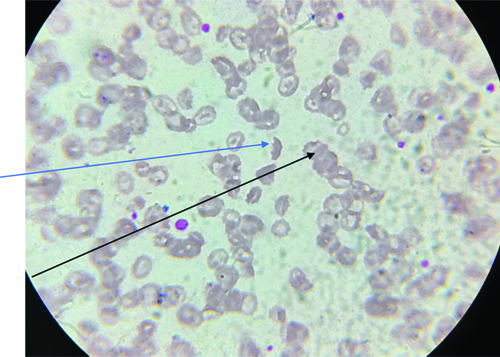
Peripheral smear was suggestive of the presence of plenty of target cells and occasional schistocytes [Table/Fig-2].
Showing schistocyte (black arrow) and target cell (blue arrow).
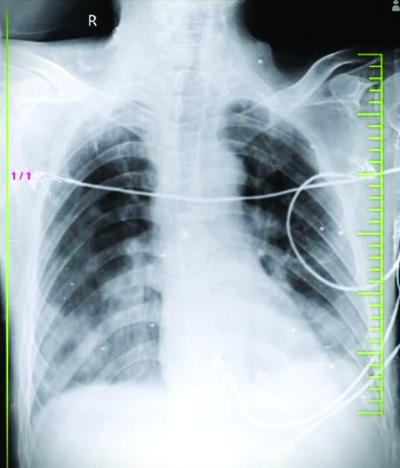
The chest X-ray revealed homogenous opacity in right lower lobe suggestive of consolidation [Table/Fig-3]. ECG was suggestive of sinus tachycardia. Ultrasonography of the abdomen and pelvis was suggestive of bilateral normal-size kidneys with raised renal cortical echotexture with maintained corticomedullary differentiation, ascites, Grade-1 fatty liver, and mild bilateral pleural effusion.
Showing right lower lobe radio-opacity.
The patient was started on supplemental oxygen support, higher injectable antibiotics such as inj. levofloxacin 500 mg i.v. OD alternate day, inj. ceftriaxone 1 gm i.v. BD, inj. doxycycline 100 mg i.v. BD, corticosteroid inj. dexamethasone 4 mg i.v. OD, and other supportive management. The patient’s relatives were explained about the need for plasmapheresis and other investigation but due to financial issues, it could not be done. The patient showed clinical improvement during the stay at the hospital and was given discharged after 12 days of hospitalisation One month later, the patient came for a follow-up visit. There were no significant complaints reported by the patient, and repeat Complete Blood Count (CBC), Liver Function Test (LFT), Kidney Function Tests (KFT), and chest X-ray results were all within normal limits.
Discussion
Scrub typhus is a zoonotic disease caused by Orientia tsutsugamushi, a gram-negative bacteria in the Rickettsiaceae family that is spread via Trombiculidae mites [1]. Humans are accidental hosts. Scrub typhus is common in tropical regions; its median mortality rate is 6% in unmanaged patients, 1.4% in managed patients, and can reach up to 70% in the absence of adequate care [2]. Scrub typhus patients typically present with cough, malaise, fever, myalgia, severe headache, lymphadenopathy, rash, and eschar. Sometimes, the patient can develop severe manifestations including DIC, meningoencephalitis, pulmonary oedema, shock, liver dysfunction, thrombocytopenia, and disseminated vasculitis which results in damage of several organs like the brain, kidneys, lungs, and liver, meninges, and skin [3,4]. There are very few case reports regarding thrombocytopenia and multiple organ dysfunction in scrub typhus.
Scrub typhus causes acute febrile illness which is common in tropical countries. One-third of the patients of scrub typhus can develop multiple organ dysfunction [5,6]. Scrub typhus incidences have been rising in India in recent years [7]. This patient had hepatitis, renal failure, thrombocytopenia, and right lower lobe pneumonia. A higher mortality rate was found in the patients with multiple organ dysfunction with scrub typhus [8]. The Karp genotype of orientia is usually associated with severe disease [9]. The onset of thrombotic microangiopathy, TTP, and disseminated intravascular coagulation, and are potential causes of thrombocytopenia in scrub typhus patients [10]. TTP is DIC, which comprises fever, microangiopathic haemolytic anaemia, thrombocytopenia, renal failure, and neurologic symptoms [11].
Since scrub typhus shared a similar clinical presentation with many endemic diseases like malaria, leptospirosis, dengue, hepatitis, and enteric fever it becomes difficult to differentiate from these. Many diagnostic modalities are now available to diagnose scrub typhus like immunofluorescence assay (direct and indirect), nucleic acid detection test, and serology test like ELISA for anti-orientia immunoglobulin G and M. In this case, immunoglobulin M came out to be positive [12,13].
The early diagnosis and initiation of antibiotics can prevent life-threatening complications. Doxycycline, chloramphenicol azithromycin, and tetracycline are effective in the management of scrub typhus [14].
Conclusion(s)
There have been very few case reports and literature available regarding TTP and MODS in scrub typhus positive individuals. In diagnosed cases of scrub typhus, treating physician should be alert to pick up early signs of mental obtundation, jaundice, purpura, and keen observation of daily laboratory parameters, especially pertaining to haematocrit, haemoglobin levels, platelet counts; so that microangiopathic haemolytic states complicating scrub typhus could be picked up early so that appropriate steps would be taken to prevent further catastrophe. In this case, the patient came late to the hospital hence multiple organ dysfunction with TTP had developed in the patient. But early initiation of aggressive treatment prevents grave consequences. Further research is also needed to understand the molecular mechanism, to prevent the consequences and decrease the mortality rate among scrub typhus patients.
[1]. Tamura A, Ohashi N, Urakami H, Miyamura S, Classification of Rickettsia tsutsugamushi in a new genus, Orientia gen. nov., as Orientia tsutsugamushi combInt J Syst Bacteriol 1995 45(3):589-91.10.1099/00207713-45-3-5898590688 [Google Scholar] [CrossRef] [PubMed]
[2]. Taylor AJ, Paris DH, Newton PN, A systematic review of mortality from untreated scrub typhus (Orientia tsutsugamushi)PLoS Neglected Tropical Diseases 2015 9(8):e000397110.1371/journal.pntd.000397126274584PMC4537241 [Google Scholar] [CrossRef] [PubMed]
[3]. Rajapakse S, Weeratunga P, Sivayoganathan S, Fernando SD, Clinical manifestations of scrub typhusTrans R Soc Trop Med Hyg 2017 111(2):43-54.10.1093/trstmh/trx01728449088 [Google Scholar] [CrossRef] [PubMed]
[4]. Dogra S, Recent advances in understanding pathophysiology of scrub typhusJK Science 2010 12(2):70 [Google Scholar]
[5]. Mahajan SK, Mahajan SK, Neuropsychiatric manifestations of scrub typhusJ Neurosci Rural Pract 2017 08(03):421-26.10.4103/jnrp.jnrp_44_1728694624PMC5488565 [Google Scholar] [CrossRef] [PubMed]
[6]. Acestor N, Cooksey R, Newton PN, Menard D, Guerin PJ, Nakagawa J, Mapping the aetiology of non-malarial febrile illness in Southeast Asia through a systematic review-terra incognita impairing treatment policiesPLoS One 2012 7(9):e4426910.1371/journal.pone.004426922970193PMC3435412 [Google Scholar] [CrossRef] [PubMed]
[7]. Dhiman RC, Emerging vector-borne zoonoses: Eco-epidemiology and public health implications in IndiaFront Pub Health 2014 2:16810.3389/fpubh.2014.0016825325052PMC4179687 [Google Scholar] [CrossRef] [PubMed]
[8]. Thap LC, Supanaranond W, Treeprasertsuk S, Kitvatanachai S, Chinprasatsak S, Phonrat B, Septic shock secondary to scrub typhus: Characteristics and complicationsSoutheast Asian J Trop Med Public Health 2002 33(4):780-86. [Google Scholar]
[9]. Kelly DJ, Fuerst PA, Ching WM, Richards AL, Scrub typhus: The geographic distribution of phenotypic and genotypic variants of Orientia TsutsugamushiClin Infect Dis 2009 48(Suppl_3):S203-30.10.1086/59657619220144 [Google Scholar] [CrossRef] [PubMed]
[10]. Nguyen TC, Cruz MA, Carcillo JA, Thrombocytopenia-associated multiple organ failure and acute kidney injuryCrit Care Clinics 2015 31(4):661-74.10.1016/j.ccc.2015.06.00426410136PMC5281060 [Google Scholar] [CrossRef] [PubMed]
[11]. Go RS, Leung N, Vascular injury to the kidney [Internet]. 21st ed. Loscalzo J, Fauci A, Kasper D, Hauser S, Longo D, Jameson JL, editorsAccess Medicine 2022 New York, NYMcGraw-Hill Education[cited 2023 May 3] [Google Scholar]
[12]. Blacksell SD, Tanganuchitcharnchai A, Nawtaisong P, Kantipong P, Laongnualpanich A, Day NP, Diagnostic accuracy of the InBios scrub typhus detect enzyme-linked immunoassay for the detection of IgM antibodies in Northern ThailandClin Vacc Immunol 2016 23(2):148-54.10.1128/CVI.00553-1526656118PMC4744921 [Google Scholar] [CrossRef] [PubMed]
[13]. Rodkvamtook W, Zhang Z, Chao CC, Huber E, Bodhidatta D, Gaywee J, Dot-ELISA rapid test using recombinant 56-kDa protein antigens for serodiagnosis of scrub typhusJ Trop Med Hyg 2015 92(5):96710.4269/ajtmh.14-062725802430PMC4426586 [Google Scholar] [CrossRef] [PubMed]
[14]. Wee I, Lo A, Rodrigo C, Drug treatment of scrub typhus: A systematic review and meta-analysis of controlled clinical trialsTrans R Soc Trop Med Hyg 2017 111(8):336-44.10.1093/trstmh/trx06629253266 [Google Scholar] [CrossRef] [PubMed]