Case Report
A 42-year-old male, weighing 64 kg and measuring 166 cm tall, came into the Emergency Room complaining of difficulty breathing. During the history taking, it was noted that the patient was a daily labourer by profession, belonging to a lower socio-economic class. He reported having scattered episodes of fever for three days, which were intermittent in nature. He experienced a gradual increase in breathlessness and dyspnoea over the last three days. He has a history of chronic tobacco consumption but did not report any co-morbidities. He had no past history of hospitalisation or any surgical history.
On general examination, the patient appeared to be of average build. His vital signs showed a Heart Rate (HR) of 112 beats per minute and a Blood Pressure (BP) of 118/72 (88) mmHg. Upon evaluation in the casualty Department, the patient’s temperature was found to be high-grade at 102 degrees Fahrenheit. The patient displayed signs of intoxication and received a score of E4V4M5 on the Glasgow Coma Scale (GCS). He was severely tachypnoeic, with a respiratory rate of 35 breaths per minute, BP of 112/56 mmHg, pulse rate of 98 beats per minute, and oxygen saturation (SpO2) of 92% on room air. Clinical examination revealed reduced breath sounds and decreased resonance on percussion over the right chest. After receiving primary treatment, the patient was referred to the Respiratory Medicine Department.
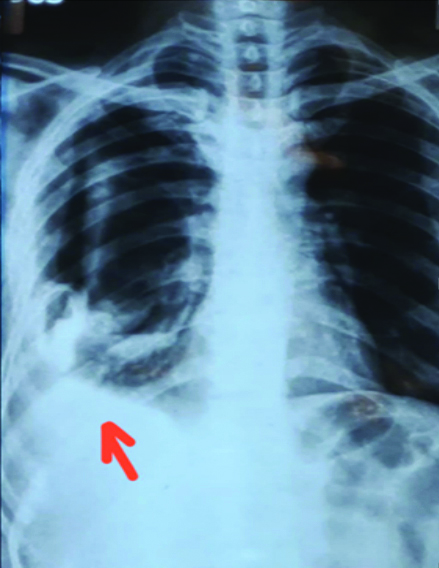
Ultrasonography and X-ray of the chest were advised [Table/Fig-1], which revealed a pleural effusion of approximately 300 mL. A CT scan was not performed due to the financial constraints of the patient and their relatives. A bedside pulmonary function test was conducted, which revealed a single breath count of 12 and a breath-holding time of 10 seconds. Arterial blood gas analysis showed a pH of 7.32, PaCO2 of 30 mmHg, PaO2 of 82 mmHg, and HCO3 of 2 mmol/L. Pleural tapping was performed, and the patient was planned for diagnostic thoracoscopy. All routine investigations were completed, revealing an increased total leukocyte count of over 20,000 cells per cubic millimeter, a normal coagulation profile, normal haemoglobin levels, and normal kidney and liver function tests. Diagnostic thoracoscopy revealed multiple loculated pus pockets in the right lung. After assessing the financial feasibility for the patient and the availability of senior consultants, a definitive management plan was developed and executed. After collecting specimens for culture and sensitivity, the patient was advised to undergo decortication of the lungs and was referred to the Cardiothoracic and Vascular Surgery Department.
Image showing the chest X-ray picture of patient. The arrow indicates the pathology in the right lungs.
The patient was scheduled for surgery and underwent pre-anaesthetic examinations. During these pre-anaesthetic check-ups, the patient was classified as American Society of Anaesthesiologists (ASA) classification III. The patient was febrile without any associated cold or cough. He had active complaints of dyspnoea and breathlessness, and his New York Heart Association (NYHA) classification was Class IV. The plan was for general anaesthesia with a right-sided DLT and the insertion of a cervical epidural catheter to manage intraoperative and postoperative analgesia.
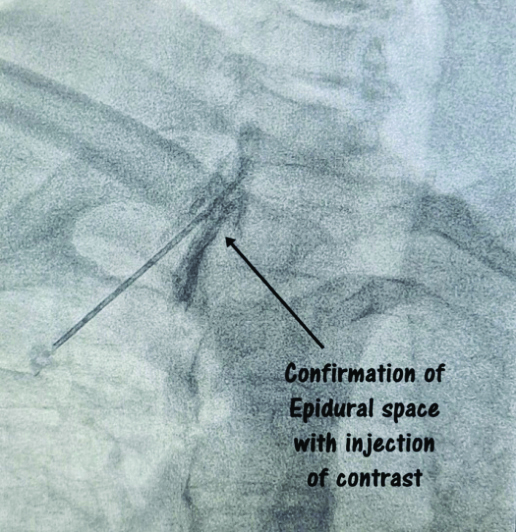
A day before the surgery, the patient was referred to an interventional radiologist for the insertion of an intercostal drain on the right side to drain pleural fluid. Under fluoroscopy guidance [Table/Fig-2], an 18 G Tuohy epidural needle [Table/Fig-3] was used, and an epidural catheter was secured at the C7-T1 vertebral level, following all aseptic precautions.
Image showing the needle reaching the epidural space.
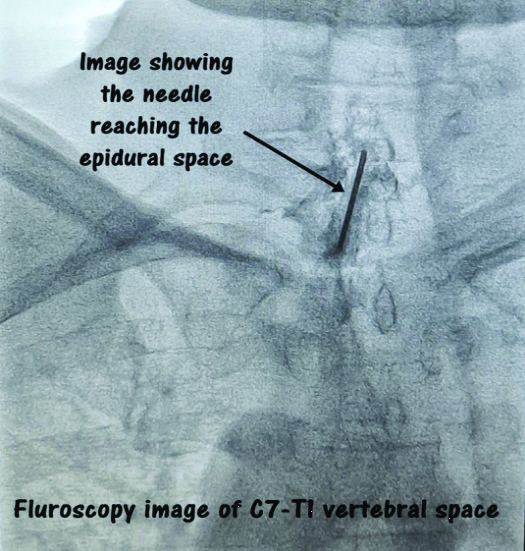
Fluoroscopic image showing needle at the epidural space. Epidural space was confirmed by the injection of contrast and its spread.
On the day of surgery, after obtaining consent for anaesthesia and the procedure, the patient was transferred to the operating theatre. A 7 French triple-lumen central venous catheter was placed in the right internal jugular vein under local anaesthesia and ultrasound guidance.
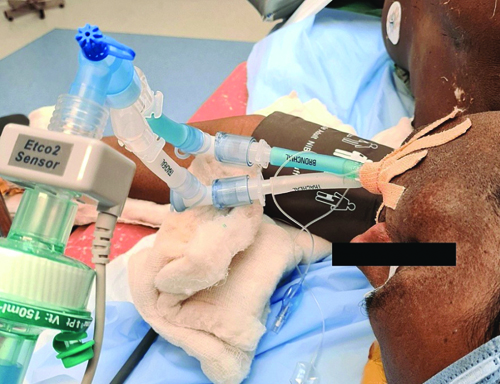
General anaesthesia was induced with an injection of glycopyrrolate (0.2 mg i.v.), midazolam (1 mg i.v.), fentanyl (100 mcg i.v.), propofol (100 mg i.v.), and vecuronium (8 mg i.v.), along with epidural anaesthesia using an injection of 240 mg bupivacaine (0.25%) in 10 mL for analgesia and improved haemodynamics. The patient was maintained on top-up doses of vecuronium (1 mg i.v.) every 30 minutes and sevoflurane. A 39-number right-sided DLT was inserted into the trachea, and the position of the tube [Table/Fig-4] was confirmed with a fiber optic bronchoscope. The end-tidal CO2 was continuously monitored. After confirmation, the tube was fixed.
Image showing 39 no. Double Lumen Tube (DLT) and left lateral position of the patient.
After induction, the patient was placed in the left lateral position and handed over to the surgeons for the further procedure. Once the surgeons requested it, the bronchial end of the tube was clamped to isolate the right side of the lungs while continuing to ventilate the left-side. The tidal volume was reduced to 5 mL/kg of body weight. The peripheral SpO2 of the patient was closely monitored, and whenever it fell below 92%, the surgeons were informed, and one-lung isolation was stopped, allowing for normal ventilation to resume.
Blood loss and haemodynamics were closely monitored, and fluid replacement was performed according to calculations. The total blood loss was calculated to be 800 mL, against the allowable blood loss of 700 mL. One unit of Packed Red Blood Cells (PRBC) was transfused over two and a half hours. Post-procedure, the patient was reversed with an injection of neostigmine (2.5 mg), extubated on the table, and sent to the intensive care unit for further monitoring. The patient was followed-up postoperatively, and timely top-up injections of bupivacaine (0.125%, 8 mL) were given every 12 hours for two days. On postoperative day three, the epidural catheter was removed. On day seven, the patient was transferred out of the ICU to the ward and discharged on postoperative day 11. Following the successful decortication of the lung abscess using OLV facilitated by a DLT, the patient showed significant clinical improvement. Postoperatively, the patient was extubated in the intensive care unit within 12 hours, maintaining stable oxygenation and haemodynamic parameters. A multidisciplinary approach, including pulmonology, infectious disease specialists, and thoracic surgeons, was pivotal in managing the patient’s recovery.
The postoperative chest X-ray showed adequate lung re-expansion, and follow-up imaging with Computed Tomography (CT) confirmed the resolution of the abscess and atelectasis. Pulmonary function tests performed three weeks postsurgery showed improved lung volumes compared to preoperative values. Antibiotic therapy was continued for six weeks based on intraoperative cultures, which identified a polymicrobial infection responsive to the regimen.
At the six-month follow-up, the patient reported a full return to baseline physical activity without dyspnoea or recurrent symptoms. Serial imaging during this period confirmed the absence of any residual abscess or significant fibrosis. The present case highlights the role of OLV with DLT as a vital technique in thoracic surgeries for severe infections, ensuring optimal surgical exposure while minimising intraoperative complications.
Discussion
The OLV is a critical technique for thoracic surgeries, particularly in procedures requiring lung isolation, such as decortication for a lung abscess. The present case highlights the successful use of a DLT to achieve OLV in a challenging clinical scenario, demonstrating both the efficacy and the associated considerations of this approach.
The use of a DLT remains the gold standard for achieving OLV due to its ability to provide selective lung isolation, protect the non-operative lung from contamination, and ensure adequate ventilation during complex thoracic surgeries [1]. In present case, the patient had a large lung abscess that required meticulous management to prevent spillage of infectious material into the contralateral lung. The strategic placement of a DLT, as reported, played a pivotal role in maintaining surgical and anaesthetic safety.
The DLT is a technique widely utilised in thoracic surgery, particularly in operations that require a calm lung on the operating side using OLV. There has been an increase in the number of patients presenting with problematic airways, making it difficult to perform oral intubation as usual [2]. Anaesthesiologists who must administer OLV as part of the surgical process face a challenging issue when confronted with such cases. Bronchial blockers have been used to separate the lungs in various surgical procedures. The DLT offers several advantages over bronchial blockers in this context. Firstly, a DLT can be inserted more quickly and with less effort compared to bronchial blockers [3]. This is because its position is nearly equivalent to that of a standard endotracheal tube. Therefore, any practitioner who already has experience with the insertion of an endotracheal tube can easily learn how to insert a DLT. Second, the cost of a DLT is significantly lower than that of bronchial blockers, and it is covered by Taiwan’s national health insurance program. Third, the likelihood of the DLT being dislodged from its intended position is lower than with bronchial blockers due to its solid structure, which helps prevent unwanted movement, and it can be securely attached to the lips using adhesive tape. In contrast, bronchial blockers have a higher-risk of becoming dislodged when subject to inflation and deflation. Fourth, a DLT features cuffs for re-inflation with a greater capacity, allowing for effective management of airway pressure even when the lung on the surgical side is being re-inflated. Finally, fiberoptic bronchoscopy is not required to confirm the accurate placement of the DLT [4]. This is a crucial point to consider because the Fiberoptic Bronchoscope (FOB) is an expensive piece of equipment that may not be available in all operating rooms. If the FOB is not accessible, we can confirm the position of the DLT by listening to the patient’s breathing with a stethoscope and performing auscultation. On the other hand, the use of the FOB is almost always necessary to ensure the accurate placement of bronchial blockers [5].
The OLV, however, is not without challenges. The ventilation-perfusion mismatch that occurs during OLV can lead to hypoxemia, a known complication. Piccioni F et al., observed that OLV contributes to Postoperative Pulmonary Complications (PPCs) in a significant proportion of cases, particularly after major lung resections. Strategies to mitigate these risks include the use of intraoperative lung-protective ventilation strategies, adequate oxygenation, and continuous monitoring of haemodynamics and gas exchange [6].
Alternative methods, such as bronchial blockers, are available for achieving lung isolation, particularly in anatomically difficult airways or in patients with prior airway pathologies. However, DLTs are preferred due to their reliability in achieving rapid lung isolation and ease of suctioning the isolated lung [7]. The present case further supports the clinical value of DLTs, as it allowed for efficient management of lung abscess drainage without intraoperative contamination.
Postoperative outcomes following OLV depend on various factors, including the patient’s baseline pulmonary function and intraoperative management. In the context of lung abscess decortication, preventing contralateral contamination is paramount. As demonstrated in present case and corroborated by previous reports, vigilant intraoperative monitoring and precise anaesthetic techniques are instrumental in reducing complications and promoting recovery [6].
The literature also underscores the importance of multidisciplinary collaboration between anaesthesiologists, surgeons, and critical care teams in ensuring optimal patient outcomes. Preoperative optimisation, intraoperative vigilance, and postoperative monitoring are essential for minimising PPCs and ensuring successful recovery [8].
Conclusion(s)
Decortication of the lungs has increasingly increased in recent times with more and more successful outcomes due to advancements in medical science and technology and the development of new anaesthetic techniques. OLV and isolation of lungs have become more sophisticated with the development of the latest DLT and fibreoptic bronchoscope. In present case report, author report successful anaesthetic management of a patient with a diagnosis of lung abscess posted for decortication of lungs. Proper preoperative assessment, appropriate planning for anaesthesia, and anticipating the complications help in the successful conduct of surgery with a favourable outcome.
[1]. Koo BS, Lee SH, Lee SJ, Jung WH, Chung YH, Lee JH, A case of one-lung ventilation using a single-lumen tube placed under fiberoptic bronchoscopic guidance in a 4-year-old child: A case reportMedicine (Baltimore) 2020 99(34):e2173710.1097/MD.000000000002173732846795PMC7447431 [Google Scholar] [CrossRef] [PubMed]
[2]. Satya-Krishna R, Popat M, Insertion of the double lumen tube in the difficult airwayAnaesthesia 2006 61(9):896-98.10.1111/j.1365-2044.2006.04754.x16922758 [Google Scholar] [CrossRef] [PubMed]
[3]. Shih CK, Kuo YW, Lu IC, Hsu HT, Chu KS, Wang FY, Application of a double-lumen tube for one-lung ventilation in patients with anticipated difficult airwayActa Anaesthesiol Taiwan 2010 48(1):41-44.10.1016/S1875-4597(10)60009-420434113 [Google Scholar] [CrossRef] [PubMed]
[4]. Zhang JH, Yang SM, How CH, Ciou YF, Surgical management of lung abscess: from open drainage to pulmonary resectionJ Vis Surg 2018 4:22410.21037/jovs.2018.10.14 [Google Scholar] [CrossRef]
[5]. Yang L, Wei X, Wang B, Dai R, Xiao F, Xu J, A comparison between bronchial blockers and double-lumen tubes for patients undergoing lung resection: A propensity score-matched cohort studyInt J Med Sci 2022 19(11):1706-14.10.7150/ijms.7583536237986PMC9553856 [Google Scholar] [CrossRef] [PubMed]
[6]. Piccioni F, Langiano N, Bignami E, Guarnieri M, Proto P, D’Andrea R, One-lung ventilation and postoperative pulmonary complications after major lung resection surgery. a multicenter randomized controlled trialJ Cardiothorac Vasc Anesth 2023 37(12):2561-71.Epub 2023 Apr 2710.1053/j.jvca.2023.04.02937730455PMC10133024 [Google Scholar] [CrossRef] [PubMed]
[7]. Liu Z, Yang X, Jia Q, One-lung ventilation in a patient with a large mass on the glottis: A case reportMedicine (Baltimore) 2018 97(36):e1223710.1097/MD.000000000001223730200151PMC6133415 [Google Scholar] [CrossRef] [PubMed]
[8]. Takechi K, Sanki Y, Abe K, Shimizu I, One-lung ventilation using a laryngeal mask airway and bronchial blocker in a patient with vocal cord cancer: A case reportJA Clin Rep 2022 8(1):2210.1186/s40981-022-00513-835298722PMC8931128 [Google Scholar] [CrossRef] [PubMed]