The extraction of a lower impacted third molar is a very prevalent routine practice. Following the surgical procedure, inflammation ensues, leading to substantial postoperative discomfort attributed to pain, swelling, and trismus, with pain identified as the primary contributor. The literature presents a myriad of modalities to mitigate these inflammatory reactions, encompassing minimally traumatic techniques, the use of medications like local anaesthetics, corticosteroids, analgesics, diverse suturing techniques, suture materials, and physical therapeutic measures [1]. Local anaesthetics play a pivotal role as fundamental elements in managing postoperative pain.
Ropivacaine, an extended-release amide-based local anaesthetic composed solely of the S (-) enantiomer, was designed to address potential toxicity issues. Its mode of operation involves temporarily blocking the entry of sodium ions, thereby halting the transmission of nerve impulses. Additionally, its effect is heightened through dose-dependent suppression of potassium channels. The decreased lipid solubility of Ropivacaine correlates with a reduced risk to the central nervous system and heart. Due to its lower lipophilicity compared to bupivacaine and its reduced inclination to enter large motor fibres covered by a sheath of myelin, Ropivacaine selectively targets the A-delta and C nerve fibres responsible for pain transmission, rather than the A β fibres involved in motor function [2].
Levobupivacaine, the S (-)-enantiomer, was developed in response to research indicating higher cardiotoxicity with the racemic R (+) enantiomer. Classified as a long-acting amino-amide local anaesthetic drug within the n-alkyl substituted pipecoloxylidide family, Levobupivacaine demonstrated reduced negative inotropic effects compared to bupivacaine. When administered intravenously at doses exceeding 75 mg, it exhibits less QTc interval prolongation and fewer Electroencephalogram (EEG) changes indicative of central nervous system depression. Levobupivacaine emerges as a viable option, as emphasised [3]. The process involves blocking voltage-sensitive ion channels in neuronal membranes, thereby halting the transmission of nerve impulses. This leads to localised and reversible anaesthesia.
Utilising a sciatic nerve block, Levobupivacaine extends the duration of postoperative analgesia, resulting in reduced consumption of analgesics [4]. In peripheral nerve blocks, Levobupivacaine demonstrates somewhat greater efficacy compared to Ropivacaine [5]. Following day-care arthroscopic knee surgery, Levobupivacaine provides superior postoperative pain relief, characterised by a prolonged time until the of rescue analgesics and a reduced overall need for postoperative analgesia compared to Ropivacaine [6]. In peri-bulbar block applications, Levobupivacaine at 0.5% exhibits effective anaesthesia in comparison to 0.75% Ropivacaine [7]. Local tissue infiltration with Levobupivacaine proved to be more efficient than Ropivacaine in mitigating postoperative pain associated with Laparoscopic cholecystectomy [8]. Levobupivacaine consistently induces an extended motor and/or sensory block [3].
The absence of conclusive evidence comparing the anaesthetic efficacy of Levobupivacaine and Ropivacaine in impacted mandibular third molar surgery had prompted the commencement of this study. The main goal of present research was to assess and compare the anaesthetic potency of 0.5% Levobupivacaine and 0.5% Ropivacaine in cases of impacted mandibular 3rd molar extraction.
Materials and Methods
A prospective, randomised, triple-blind trial was conducted in the Department of Oral and Maxillofacial Surgery at Sharad Pawar Dental College and Hospital, India from November 2023 to May 2024. The study was conducted in adherence to the Helsinki Declaration and its subsequent revisions, or similar ethical standards, and followed the Institutional Ethical guidelines specified by the Institutional Ethics Committee (IEC) (DMIMS(DU)/IEC/2022/771). The trial was registered on the Clinical Trail Registry of India (CTRI) website (CTRI/2023/10/059014). Written informed consent was obtained from all participants before conducting the study.
Inclusion criteria: Inclusion criteria comprised individuals categorised as American Soceity of Anaesthesiology (ASA) Grade 1, aged 18-40 years, with complaints of atleast one symptomatic impacted mandibular third molar of moderate difficulty (as per Modified Pederson’s Scoring) [9].
Exclusion criteria: Exclusion criteria encompassed individuals with a history of drug dependence, systemic diseases such as Hypertension (HTN), Diabetes Mellitus (DM), blood disorders, immunocompromised conditions, chronic smoking habits, allergies to the local anaesthetic agents used, pregnancy or nursing, use of oral contraceptives, ongoing treatment with antibiotics or anti-inflammatory drugs, history of drug dependence any local infections such as pericoronitis or pterygomandibular space infection, chronic facial pain on the intervention side, radiological signs of proximity to the inferior alveolar canal, or psychiatric illnesses.
Post-enrollment exclusion criteria involved individuals for whom the Inferior Alveolar Nerve Block (IANB) technique failed or required repeat administration, or those experiencing prolonged paresthesia during the nerve block exceeding 12 hours postsurgery.
Sample size calculation: The sample size was calculated using the Cochran formula:
n=Zα2/2 P (1-P)/E2Where Zα/2 is the level of significance at 5%, i.e., a 95% Confidence interval=1.96, P=proportion of impaction at transverse=2=0.02 [10], E=margin of error=5=0.05. Therefore, n=1.96×0.02×(1-0.02)/0.052=30.11, indicating that 30 patients were needed in each group.
Study Procedure
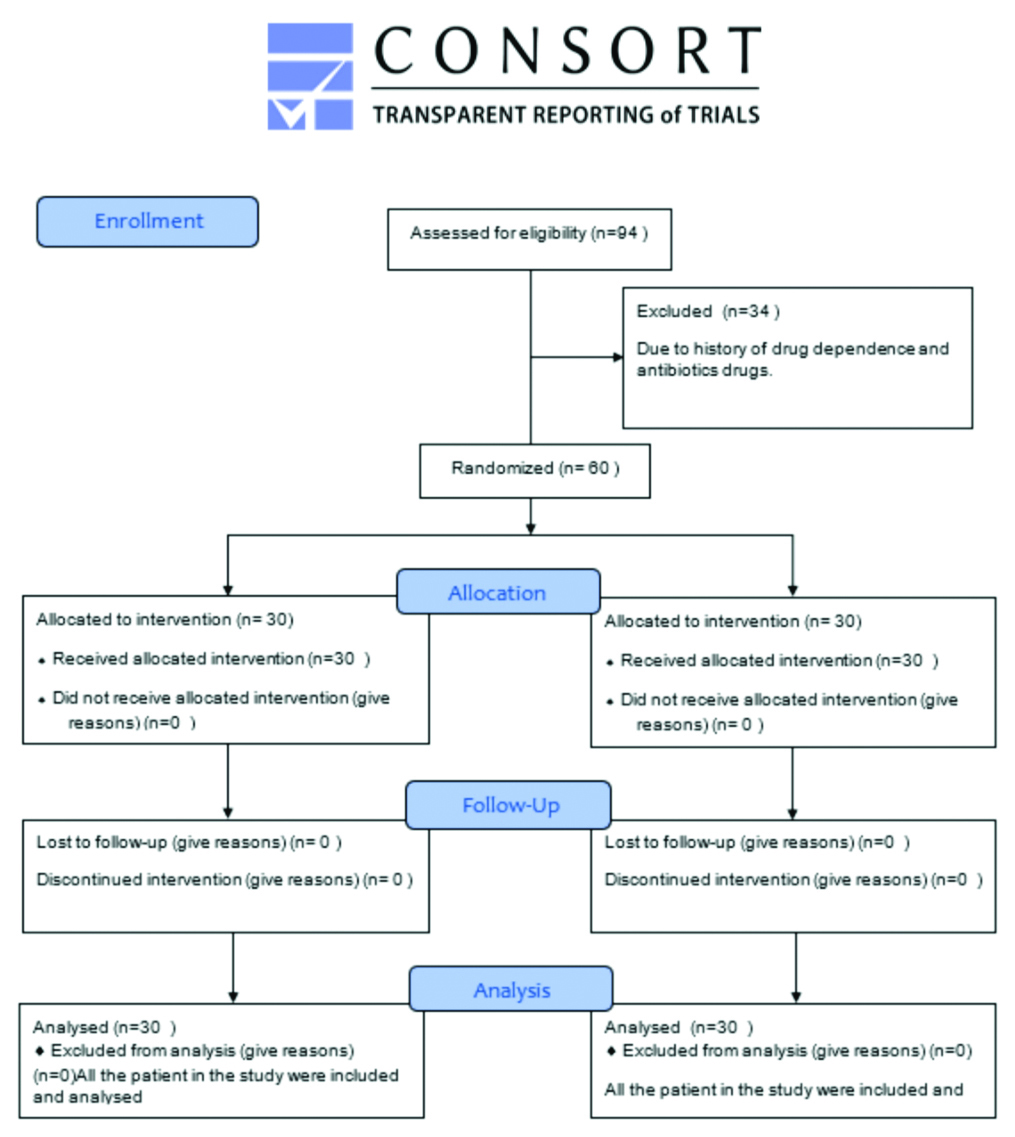
The study employed a triple-blind methodology to ensure that the subjects, the administering clinician of the local anaesthetic, and the evaluator were unaware of the specific drug being used. An independent researcher, trained for this purpose, provided the local anaesthesia to the surgeon, who then administered it without knowledge of the solution’s identity, maintaining detailed records throughout. A total of 94 patients were included in the study, of which 34 were excluded due to a history of drug dependence. A total 60 systemically healthy patients aged 18-40 years reporting to the Outpatient Department (OPD) of oral and maxillofacial surgery were included in the study. The study included two groups: Group A, who were injected with 0.5% Levobupivacaine, and Group B, who were injected with 0.5% Ropivacaine [Table/Fig-1] [11].
Consodilated Standards of Reporting Trails (CONSORT) flowchart [11].
These 60 patients were randomly split into two groups using a lottery system (n=30). The parameters evaluated were:
Latency of anaesthesia: This was calculated from the time of deposition of local anaesthesia to the onset of the initial symptoms of anaesthesia, recorded subjectively by asking questions about lip and tongue numbness and objectively with the help of a running Moons probe on the gingiva. An independent researcher recorded the latency of mandibular anaesthesia at 30-second intervals.
Profoundness (Depth) of anaesthesia: This was determined by the pain experienced throughout the surgical procedures (including incision, flap elevation, bone guttering, and odontectomy/elevation). It was measured intraoperatively at each step mentioned above using a 10-unit Visual Analogue Pain Scale (VAS) [12]. The VAS consists of a 0-10 scale, where 0 indicates “No pain” and 10 indicates “Worst pain.”
Time to rescue analgesia: The duration was recorded from the onset of anaesthesia to the time when the first bout of pain occurred (VAS ≥4) postoperatively, at which point the patient consumed the rescue analgesic. This was considered the endpoint. Patients were asked to keep a record of this and were recalled for follow-up after one week.
Statistical Analysis
The software utilised for this analysis was Statistical Package of Social Sciences (SPSS) version 27.0 and GraphPad Prism version 7.0. All data were recorded in an MS Excel spreadsheet, and statistics were calculated. Statistical analysis was conducted using both descriptive and inferential statistics. Student’s unpaired t-test was used to calculate and compare the onset of anaesthesia and time to rescue analgesia, while Fischer’s-exact test was used for the profoundness of anaesthesia. A significance level of p<0.05 was employed for interpreting the results.
Results
A total of 94 patients were assessed for eligibility, and 34 were excluded from the study due to a history of drug dependence and antibiotic use [Table/Fig-1]. This left two groups: Group Levobupivacaine (A), injected with 0.5% Levobupivacaine, and Group Ropivacaine (B), injected with 0.5% Ropivacaine for the extraction of impacted mandibular third molars. The subjects were age and gender-matched (p=0.89). In Group B, 16 (53.33%) patients were in the age group of 18-27 years, and 11 (36.67%) were in the age group of 28-37 years. In Group A, 17 (56.67%) patients were in the age group of 18-27 years, and 11 (36.67%) were in the age group of 28-37 years. The mean age of subjects in the study sample was 27.26±6.13 years in Group B and 27.23±5.24 years in Group A. The overall mean age of subjects was 27.23±5.24 years [Table/Fig-2]. The study population comprised 26 (43.33%) males and 34 (56.67%) females. Group B had 11 (36.67%) males and 19 (63.33%) females, while Group A had 15 (50%) males and 15 (50%) females [Table/Fig-3].
Displays age-wise distribution in two groups.
| Age in years | Group A | Group B | Total |
|---|
| 18-27 years | 17 (56.67%) | 16 (53.33%) | 33 (55%) |
| 28-37 years | 11 (36.67%) | 11 (36.67%) | 22 (36.67%) |
| >37 years | 2 (6.67%) | 3 (10%) | 5 (8.33%) |
| Total | 30 (100%) | 30 (100%) | 60 (100%) |
| Mean±SD | 27.23±5.24 | 27.26±6.13 | 27.23±5.24 |
| Range | 19-40 y | 18-40 y | 18-40 y |
Displays the gender-wise distribution in two groups.
| Gender | Group A | Group B | Total |
|---|
| Male | 15 (50%) | 11 (36.67%) | 26 (43.33%) |
| Female | 15 (50%) | 19 (63.33%) | 34 (56.67%) |
| Total | 30 (100%) | 30 (100%) | 60 (100%) |
The mean latency of anaesthesia following administration of the anaesthetic solution in subjects of Group-B (Ropivacaine) was 192.33 seconds, while that of subjects in Group A (Levobupivacaine) was 104.06 seconds. Levobupivacaine demonstrated a significantly better latency of anaesthesia than Ropivacaine, which was found to be statistically significant (p=0.0001) [Table/Fig-4].
Displays the latency of anaesthesia in two comparative groups.
| Group | n | Mean (sec) | Std. Deviation | Std. Error mean | t-value | p-value |
|---|
| Group-A | 30 | 104.06 | 17.66 | 3.22 | 14.68 | 0.0001**, S |
| Group-B | 30 | 192.33 | 27.78 | 5.07 |
*Unpaired t-exact test; **p-value=0.0001
A few subjects experienced mild pain in both groups: Levobupivacaine and Ropivacaine, while reflecting on the flap, guttering of the bone, and third molar elevation/sectioning. The overall pain scores were always <4 on the VAS at all steps. However, the difference in pain intensity scores on the VAS between both groups at all time intervals was found to be statistically non significant (p=1.00) [Table/Fig-5].
Comparison of the profoundness (Depth) of anaesthesia of groups A and B.
| Pain score | Incision | Flap reflection | Tooth/Root sectioning | Bone guttering |
|---|
| Group-A | Group-B | Group-A | Group-B | Group-A | Group-B | Group-A | Group-B |
|---|
| No pain | 30 (100%) | 30 (100%) | 30 (100%) | 30 (100%) | 27 (90%) | 27 (90%) | 26 (86.67%) | 27 (90%) |
| Mild pain | 0 | 0 | 0 | 0 | 3 (10%) | 3 (10%) | 4 (13.33%) | 3 (10%) |
| Total | 30 | 30 | 30 | 30 | 30 | 30 | 30 | 30 |
| p-value | - | - | - | 1.00, NS, p>0.05 |
*Fisher’s-test; **p-value=1.00; NS
The time to rescue analgesia was found to be 501.83 minutes (approximately 8.36 hours) in the Ropivacaine group, while for the Levobupivacaine group, it was 656.50 minutes (approximately 10.9 hours). The difference between both groups was found to be statistically significant (p=0.0001) [Table/Fig-6].
Displays the time to rescue analgesia of the drugs given in two groups.
| Group | n | Mean (in minutes) | Std. Deviation | Std. Error mean | t-value | p-value |
|---|
| Group-A | 30 | 656.50 | 29.21 | 5.33 | 12.28 | 0.0001, S |
| Group-B | 30 | 501.83 | 62.44 | 11.40 |
*Student unpaired t-test; **p-value is 0.0001
Discussion
The present study compared the effects of Levobupivacaine and Ropivacaine as local anaesthetics. It found that Levobupivacaine had a faster onset of anaesthesia than Ropivacaine, which was statistically significant. Both drugs showed similar effectiveness in achieving the depth of anaesthesia during surgery, with no statistically significant difference observed. However, the Levobupivacaine group exhibited a longer time to rescue analgesia compared to the Ropivacaine group, with a statistically significant difference.
The extended duration of anaesthesia observed with Levobupivacaine may be due to its inherent vasoconstrictive properties and strong affinity for binding to plasma proteins. In contrast, Ropivacaine has a weaker bond to the surrounding fat and tissues, making it more readily available to transfer to the nerve site. A similar study in 2015 compared the anaesthetic efficacy of 0.5% Ropivacaine and 2% lidocaine hydrochloride for lower third molar procedures and concluded that 0.5% Ropivacaine alone does not affect the cardiovascular system and has more beneficial effects than 2% lidocaine hydrochloride with adrenaline. These findings may be valuable for oral and maxillofacial surgeons seeking a local anaesthetic with minimal cardiovascular risk and without a vasoconstrictor for regional anaesthesia during lengthy procedures [13].
In another study conducted in 2021, three local anaesthetic agents-2% lidocaine hydrochloride with 1:80,000 adrenaline, bupivacaine, and Ropivacaine-were compared for their efficacy in pain control during tooth extraction. It was concluded that 0.75% Ropivacaine is a better anaesthetic compared to bupivacaine and lidocaine for pain control during third molar extractions, providing better intraoperative and postoperative pain control during extraction of posterior mandibular teeth [14].
The time to rescue analgesia is equal to the duration of postoperative analgesia, and the present study showed that the time for the consumption of rescue analgesics varied considerably. Levobupivacaine exhibited a prolonged time to require analgesia compared to Ropivacaine, which was statistically significant (p<0.05).
The time to require analgesia depends on several factors, including the extent of protein binding capacity, subjective response to the drug, tissue health at the drug deposition site, and the strength of the anaesthetic [15]. A study comparing the efficacy of 0.75% Levobupivacaine and 3% mepivacaine for pain control after surgical removal of impacted mandibular third molars found no significant differences in anaesthesia onset, duration of surgery, lip numbness, the timing of pain appearance, and analgesic consumption between the two groups. However, patients with Levobupivacaine anaesthesia had significantly lower pain scores at 1 and 2 hours postoperatively, suggesting that Levobupivacaine is a valid alternative to traditional local anaesthetics for the surgical removal of lower third molars [16].
The findings of the present study are consistent with previous research that evaluated the effectiveness of Levobupivacaine and Ropivacaine for managing pain following outpatient minimally invasive knee surgery. This research found that the time of the first analgesic request was longer for Levobupivacaine compared to Ropivacaine [6]. A similar study in 2018, which compared the impact of the two drugs in sciatic nerve block using the traditional Labat technique for foot and ankle surgical procedures, also showed that the time to require analgesia was longer for Levobupivacaine compared to Ropivacaine [4].
Ropivacaine, a long-acting anaesthetic compared to lignocaine with adrenaline, provides prolonged anaesthesia and postoperative analgesia. It is safer for patients with cardiovascular problems as its impact on the cardiovascular system is not as pronounced as that of lignocaine hydrochloride [17]. The delayed onset of anaesthesia associated with Ropivacaine can be attributed to its significantly lower lipophilicity compared to levobupivacaine. This characteristic leads to a slower diffusion of the drug into the myelinated nerve fibres and poses challenges in inducing local vasoconstriction in the tissue surrounding the injection site. The latency of the drug depends on the pKa value (dissociation constant); the lower the pKa value, the shorter the time of onset. The rapid latency in Group Levobupivacaine group, compared with that of the Ropivacaine group, may also be due to their difference in pKa values. Levobupivacaine has a lower pKa value compared to Ropivacaine, which explains the rapid onset of action of Levobupivacaine [18].
Dhanrajani P et al., compared the efficacy of 0.25% bupivacaine with 0.5% bupivacaine and concluded that during the first few hours following surgery, bupivacaine 0.5% was statistically superior for pain management; however, at two and twenty-four hours, there was no discernible difference in pain management between the two dose strengths [19].
The findings of the present study were not consistent with the trial conducted by Brajkovic D et al., who evaluated anaesthetic parameters, postoperative analgesia and vasoactive properties of Levobupivacaine and bupivacaine for lower third molar surgery [20]. They concluded that Levobupivacaine 0.5% achieved superiority over bupivacaine 0.5% in the intensity of intraoperative anaesthesia and duration of postoperative analgesia for lower third molar surgery under mandibular nerve blocks [20].
Levobupivacaine has a shorter latency of anaesthesia than Ropivacaine. Mageswaran R and Choy YC, compared 0.5% Ropivacaine and 0.5% Levobupivacaine for infraclavicular brachial plexus and concluded that Levobupivacaine 0.5% achieved superiority over bupivacaine 0.5% in the intensity of intraoperative anaesthesia and duration of postoperative analgesia for lower third molar surgery under mandibular nerve blocks [21]. Samar P et al., concluded that there was an earlier onset of sensory and motor block and a prolonged duration of both sensory and motor blocks with the intrathecal administration of 3 mL of 0.5% isobaric Levobupivacaine compared to 3 mL of 0.75% isobaric Ropivacaine. Haemodynamic parameters were more stable with Levobupivacaine than with Ropivacaine and adverse effects were more common with Ropivacaine [22].
Kim HJ et al., evaluated the onset time for ultrasound-guided infraclavicular brachial plexus block using 0.375% Ropivacaine and 0.25% levobupivacaine. The findings indicated that the sensory latency time for Ropivacaine was shorter compared to Levobupivacaine (Group-R: 15 (15-22.5) minutes vs. Group-L: 30 (17.5-35) minutes) [23].
The profundity of anaesthesia is the depth of anaesthesia. The majority of the subjects from both groups did not experience the pain with a VAS score <4 during procedures such as incision, flap reflection, gutter creation in the bone, and tooth sectioning/elevation. In comparison, a few patients in both groups experienced mild pain. No significant difference (p>0.05) was observed between the two groups. These results indicate that Levobupivacaine demonstrates comparable potency and provides a depth of effect similar to that of Ropivacaine solution.
Limitation(s)
A split-mouth study design is desirable for assessing the potency of any local anaesthetic drug administered, but it is difficult to find a patient with a bilaterally similar impaction grade for the standardisation of the procedure. Further, studies taking into consider the number of analgesics consumed postoperatively would help quantify the analgesic efficacy of the drug. Multicentric trials with a larger sample size are needed. Additionally, in the present study, examining the effects of the plasma concentrations of Ropivacaine and Levobupivacaine on the cardiovascular system using impedance cardiography would have been more desirable.
Conclusion(s)
Both Levobupivacaine and Ropivacaine were comparable in terms of the depth of anaesthesia. However, Levobupivacaine showed better latency and a longer time to rescue analgesia, attributed to its higher lipophilicity, protein binding, and lower pKa compared to Ropivacaine. This suggests that Levobupivacaine is a valid alternative to traditional local anaesthetics for the surgical removal of lower third molars.
*Unpaired t-exact test; **p-value=0.0001
*Fisher’s-test; **p-value=1.00; NS
*Student unpaired t-test; **p-value is 0.0001