The LC is the well-established gold standard therapy for gallstone disease. Gallstone disease is one of the most common surgical conditions diagnosed in the United States, affecting 0.60-1.39% of the general population per year and contributing significantly to healthcare expenditure [1]. Laparoscopic IPOM repair of ventral hernias has also gained tremendous popularity in the present era of minimally invasive surgery. It was introduced in 1993 by Karl LeBlanc and Booth, who first described the approach with the insertion of an intraperitoneal mesh without closure of the hernia defect [2].
Ventral hernia repair represents a significant fiscal burden on healthcare, with around 300,000 ventral hernia repair operations performed each year in the United States. There is an estimated annual increase in this number of 11,000 [3]. Since, both gallstone disease and ventral hernia are highly prevalent, they may occur concomitantly. However, the concurrent performance of both LC and IPOM for co-existing gallstone disease and ventral hernia is, at first glance, against established principles of surgery, as it is an ‘unholy’ combination of a clean (IPOM) and a clean-contaminated (LC) operation.
At the present Institute, performing LC and IPOM in the same sitting is the treatment of choice for carefully selected patients. The present retrospective study aimed to evaluate the short- and long-term results in patients who underwent concurrent LC and IPOM.
Materials and Methods
This retrospective observational study was conducted at the Department of General and Laparoscopic Surgery, Dr. L H Hiranandani Hospital, Mumbai, India from August 2005 to July 2024. The study population comprised patients who had undergone LC and IPOM in the same sitting for concurrent gallstone disease and ventral hernia. Since, this was a retrospective study, prior clearance from the Institutional Ethics Committee was not applicable.
Inclusion criteria:
Absence of acute cholecystitis-no tenderness in the right hypochondriac region with a normal liver profile and total leukocyte count;
Absence of obstructed and/or strangulated hernia;
Absence of known coagulation disorders;
Medically fit and stable patients {American Soceity of Anaesthesiologists (ASA) I, controlled ASA II and III}.
Exclusion criteria:
Acute cholecystitis;
Obstructed/strangulated ventral hernia;
Acute urinary tract infection;
Patients with known coagulation disorders.
Study Procedure
A total of 15 patients were included in present study, all operated on by a single surgeon. All patients were assessed for fitness for surgery on an outpatient basis. The specific preoperative investigations included urinalysis, an Ultrasonography (USG) scan of the abdomen, liver profile, and a complete blood count, in addition to other routine biochemical investigations.
Operative technique: The surgeries were performed under general anaesthesia for all patients. They were placed in a supine position with the right hand tucked in by the side of the patient to facilitate the IPOM part of the surgery. Two monitors (one on the patient’s right and the other on the left) were used. A prophylactic antibiotic of third-generation cephalosporin (Ceftriaxone 1 gm) was administered intravenously to each patient just before the start of surgery.
Separate trolleys were prepared for the two procedures, meaning that two sets of Maryland forceps, laparoscopic scissors, and graspers were kept ready on separate trolleys at the outset. In all patients, LC was performed first, followed by the IPOM. In all surgeries, the scrub nurse and the remaining surgical team changed gloves after the LC before initiating the IPOM, after cleansing both hands with Bactorub® to minimise the risk of cross-infection and contamination. A standard four-trocar approach was used for LC.
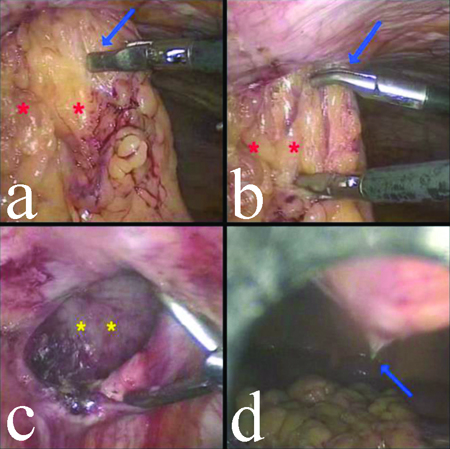
Pneumoperitoneum was established by the closed method using a Veress needle. In patients with an incarcerated umbilical hernia, the lateral 5 mm trocars for LC were inserted first, followed by the epigastric 10 mm trocar, under the vision provided by a 5 mm telescope inserted through the lateral 5 mm trocar. After this, the epigastric trocar was used as the 10 mm optic port, and the incarcerated contents were reduced using instruments introduced through the two right lateral 5 mm trocars, with the surgeon standing on the right-side of the patient [Table/Fig-1a,b]. Following the reduction of the hernia contents, the umbilical hernial defect was demarcated and measured [Table/Fig-1c]. The umbilical optic 10 mm trocar was then inserted [Table/Fig-1d], and the surgeon moved to the left-side while the camera was positioned at the umbilical trocar to proceed with the LC [Table/Fig-2a-d].
a,b) Incarcerated umbilical omentocele (red asterisks) being reduced (blue arrow); c) Umbilical hernia defect (yellow asterisks) after complete reduction of it’s contents; d) Insertion of supraumbilical trocar (blue arrow) after reduction of the hernial contents.
a) Cystic duct being clipped (blue arrow); b) Division of cystic artery between clips (blue arrow); c) GB being separated from the Gallbladder (GB) fossa on the liver (blue arrow); d) Haemostasis at the GB fossa (blue arrow).
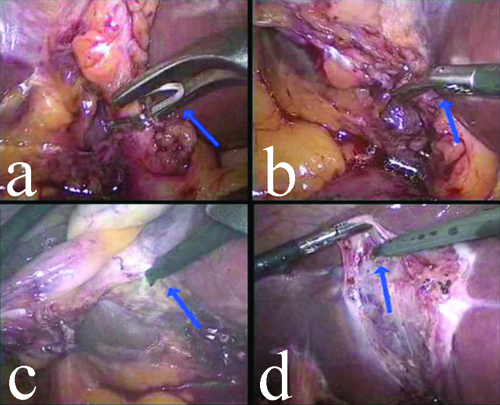
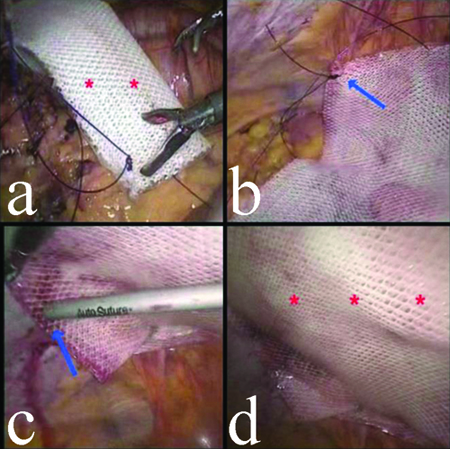
After completing the LC, the specimen was retrieved from the epigastric trocar in a retrieval bag. The surgeon then moved back to the right-side, and the camera was repositioned to the epigastric trocar. The umbilical trocar was removed, and the skin wound was sutured closed. A standard IPOM was then performed through the two right lateral 5 mm trocars using dual mesh (Parietex®, Covidien), a suture passer, four corner transfacial sutures, and an absorbable tacker [Table/Fig-3a-d]. In patients with uncomplicated ventral hernias, the LC was completed first, followed by the IPOM. Adhering to smart ergonomics, all patients in this series underwent both LC and IPOM through the same four standard LC trocars, without the insertion of any extra trocar in any of the 15 patients.
a) Rolled dual mesh (red asterisks) inserted into the abdomen; b) The corner transfascial sutures being pulled out (blue arrow); c) The mesh being tack-fixed to the parietes (blue arrow); d) Endresult with mesh in-situ (red asterisks).
The parameters studied included age range, sex ratio, duration of surgery, length of hospital stay, time to resumption of normal activities, the comparative cost of the concurrent approach versus two individual surgeries in different sittings, and intra- and postoperative complications. To calculate the comparative cost, three sets, each with two patients, were formed. One patient in each set underwent the two surgeries concurrently, while the second patient had the two surgeries performed in two different sittings. Both patients in each set were operated on within six months of each other. The total hospital bills of both patients from all three sets were obtained, and the difference in the figures was calculated, resulting in an average of the three figures.
Statistical Analysis
The statistical analysis was conducted using the Statistical Package for the Social Sciences (SPSS) version 22.0 software. Proportions, percentages, and means were calculated.
Results
Total of 15 patients constituting 9 females and 6 males with a diagnosis of gallstone disease and ventral hernia underwent concurrent LC and IPOM. The mean age of the patients was 55±12.36 years (range 35-77 years). The mean follow-up period was 112.29±61.12 months (range 17-226 months). Total 9 (60%) patients had an umbilical hernia, 2 (13.33%) had an incisional hernia, 1 (6.67%) had an epigastric hernia, and 3 (20%) had a paraumbilical hernia. Total 5 patients (33.33%) had an incarcerated umbilical omentocele, while the remaining 10 (66.67%) patients had uncomplicated ventral hernias. Several patients had co-morbidities such as hypertension (n=9), ischaemic heart disease (n=3), diabetes mellitus (n=7), hypothyroidism (n=4), and chronic obstructive pulmonary disease (n=2). The mean operating time was 62±11.26 minutes (range 48-70 minutes). The mean postoperative stay was 2.5±1.23 days (range 2-3.5 days). The mean duration to resumption of normal activities was 7±2.5 days (range 6-10 days) [Table/Fig-4].
Patient demographics (N=15).
| Patient characteristics | N (%) |
|---|
| Total number of patients | 15 |
| M:F | 6:9 |
| Mean age (range) | 55 years (35-77 years) |
| Average duration of surgery (range) | 62 minutes (48-70 minutes) |
| Average hospital stay | 2.5 days |
| Average time to resumption of normal activities | 7 days |
| Reduction of cost by concurrent approach | 28% |
| Mean follow-up period (range) | 112.29 months (17-226 months) |
| Umbilical hernia | 9 (60%) |
| Incisional hernia | 2 (13.33%) |
| Epigastric hernia | 1 (6.67%) |
| Paraumbilical hernia | 3 (20%) |
| Uncomplicated ventral hernia | 10 (66.67%) |
| Complicated ventral hernia | 5-incarcerated omentocele (33.33%) |
Three patients developed small seromas at the umbilical trocar site three weeks post-surgery; these self-resolved over six weeks. No patient experienced significant postoperative bleeding or haematoma, and there were no cases of wound or mesh infection. Over a mean follow-up period of 112.29 months, none of the patients developed any recurrence of hernia. Two patients experienced minor bleeding at the epigastric trocar site during insertion, which was easily controlled. None of the patients had any major complications related to LC, such as internal haemorrhage or biliary leaks, and there were no incidents of iatrogenic bowel injury. Two patients have died, seven and 11 years after surgery, both due to myocardial infarction. The intra- and postoperative complications are summarised [Table/Fig-5]. The hospital cost was reduced by an average of 28% compared to a scenario where the two surgeries were performed separately on two different occasions at the present Institute.
Intraoperative, early and late postoperative complications.
| Variables | N (%) |
|---|
| Intraoperative complications |
| Port site bleeding | 2 (13.33%) |
| Significant haemorrhage | 0 |
| Enterotomy | 0 |
| Postoperative complications |
| A) Early | |
| Significant haemorrhage | 0 |
| Seroma | 0 |
| Bile leak | 0 |
| B) Late | |
| Seroma | 3 (20%) |
| Haematoma | 0 |
| Mesh infection | 0 |
| Surgical Site Infection (SSI) | 0 |
| Recurrence of hernia | 0 |
Discussion
The LC is considered a clean-contaminated surgery, while IPOM is classified as a clean surgery. The concurrent performance of both procedures, one after the other in the same sitting, defies established conventions and best practice guidelines in surgery. The obvious advantage of performing two such operations in separate sittings is the elimination of any chance of cross-infection, specifically mesh infection in the present case. On the other hand, the benefit of concurrent performance is the convenience for the patient of being treated for two different surgical conditions during one hospital stay and under a single session of anaesthesia.
Another relative advantage is the significant cost savings compared to undergoing the two surgeries in separate hospital stays. Due to the perceived reasonable risk of contamination and infection of the mesh prosthesis, concurrent LC and IPOM have not been extensively studied before. A review of the literature revealed only one published paper on the topic [4].
A summary of recent literature on concurrent LC and laparoscopic hernia repair is provided [Table/Fig-6] [1,4-7]. Although the present sample size is small, it is important to note that we did not have a single case of mesh infection. This underscores the significance of meticulous, rigorous, and strict patient selection for concurrent LC and IPOM. Additionally, it reinforces the idea that concurrent LC and IPOM are possible, feasible, and safe, and that with appropriate adherence to optimal ergonomic principles, it can be performed without the need for inserting any extra trocars beyond the standard four trocars used for LC, in most situations.
Review of recent literature on concurrent LC+Lap. hernia repair [1,4-7].
| Authors | Year of publication | Type of study/No. of patients/Combinations | Incidence of mesh infection | Conclusion(s) |
|---|
| Becker TP et al., [1] | 2023 | Retrospective comparative multicentre database study/167586 (total no, of patients)1821 patients- concurrent LC+Lap ventral hernia repairComparison of outcomes between 2 groups-1. ventral hernia repair alone vs 2. Lap ventral hernia repair+LC | 1.86% | 1. No significant difference in postoperative outcomes2. No difference in infection-related complications between the two groups3. No increased risks for patients undergoing concurrent ventral hernia repair+LC |
| Praveen Raj P et al., [4] | 2015 | Retrospective/246Concurrent IPOM+hysterectomy – 126 patientsConcurrent IPOM+LC – 120 patients | 0.8% | 1. Safe2. Acceptable morbidity3. Does not significantly alter the outcome of the procedure |
| Claus CMP et al., [5] | 2021 | Retrospective/46Concurrent LC+Lap. Inguinal hernia repair – 46 patients | 0 | 1. Safe procedure2. No increase in mesh infection3. Reduction of hospital costs and increase in patient satisfaction |
| Akay T et al., [6] | 2023 | Retrospective/38Concurrent LC+Transabdominal Preperitoneal (TPP) | 0 | 1. Safe2. No increase in mesh infection rates |
| Hayakawa S et al., [7] | 2018 | Retrospective/17Concurrent LC+TAPP | 0 | 1. Safe2. Recommended as standard surgical procedure |
Limitation(s)
It has a small sample size, and larger randomised studies are required to establish the findings of the present study. Additionally, it was conducted at a single centre by a single surgeon, which limits the generalisability of the results to other settings. The long follow-up period may have introduced recall bias in the present study. Furthermore, the absence of a control group creates a potential for bias in the results. In the absence of a control group, it is difficult to determine the true efficacy of the procedure.
Conclusion(s)
With appropriate case selection, concurrent LC and IPOM are practical, cost-effective, and safe procedures. Larger studies on the subject in the future will further validate the findings of the present study.