Case Report
A five-year-old male child visited the Kaumarbhritya (Paediatric) with the chief complaints of intermittent, severe, sharp pain in the epigastric and left hypochondriac regions, radiating to the back for the past 10 days. He had experienced nausea for the last four days, intermittent projectile vomiting, fever, and loss of appetite, along with sleeplessness for the past two days. He was diagnosed with Grahani Roga (Acute Pancreatitis) using ultrasonography and laboratory findings.
Ten days ago, the patient was apparently healthy, but he suddenly started experiencing abdominal pain, nausea, vomiting, discomfort, and anorexia. He commenced allopathic treatment with antibiotics, antacids, and supportive care (Nil per Os-nothing by mouth, and intravenous fluid hydration). He was provided with inj. Monocef 750 mg i.v for three days, inj. Tramadol 35 mg in a drip of 50 mL with normal saline intravenously twice a day for three days, inj. Paracetamol 150 mg intravenously as needed, syrup Ibugesic 8 mL orally as needed for three days, and syrup Rantac 5 mL orally twice a day for three days. He experienced some symptomatic relief from this treatment but stopped in the middle. His parents were not satisfied with the ongoing treatment, so they turned to Ayurveda modalities.
There was no history of diabetes mellitus/insipidus, hypertension, bronchial asthma, or hypothyroidism. There were no major illnesses in the family, except for constipation. Abdominal examination revealed notable tenderness to palpation, guarding, with no signs of peritoneal irritation, distention, or rigidity, and decreased bowel sounds. Seven days before admission, he presented with significant aggregation of symptoms, including severe continuous epigastric pain, nausea, and severe persistent projectile vomiting (5-6 episodes). He had a recent travel history. He had no history of hepatic disease, gallstones, or a family history of pancreatitis. Additionally, there is no history of trauma or surgery.
His personal history reveals a habit of frequently consuming packaged and fast foods, leading to constipation, irregular bowel movements with hard stools, and disturbed sleep. Physical examination findings showed mild abdominal tenderness and mild distention. His pulse was 80 beats per minute, respiratory rate 25 breaths per minute, and blood pressure was 100/60 mmHg. His weight was 16 kg, height was 106 cm, which is appropriate for his age and sex.
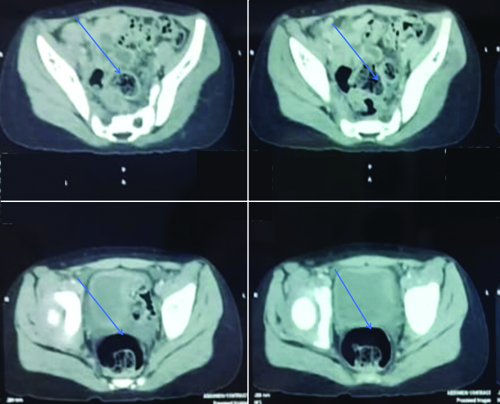
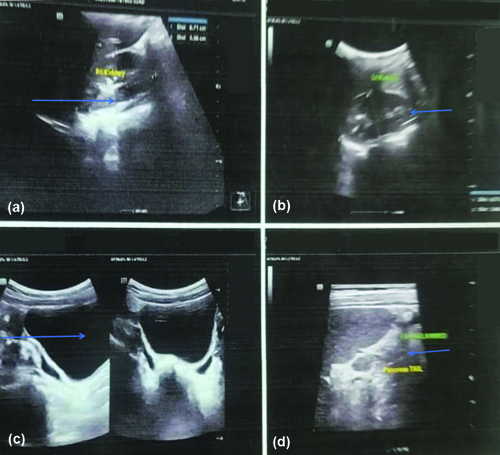
There was a significant increase in the laboratory values of serum amylase, serum lipase, serum alkaline phosphate, and aspartate aminotransferase. These are common biochemical markers in patients with acute pancreatitis [Table/Fig-1]. Contrast-enhanced Computed Tomography (CECT) revealed that the pancreas was minimally bulky in the body and tail regions, with a normal echo texture. There was a focal area of fat inflammation in the left lumbar region adjacent to the tail of the pancreas, suggesting acute pancreatitis [Table/Fig-2]. An abdominal ultrasound revealed an enlarged, heterogeneous pancreas with anterior bending and an irregular surface, encircled by peripancreatic fluid, as well as dilated pancreatic and common bile ducts. Several gallstones, each measuring an average of 6-7 mm, were also noted [Table/Fig-3a-d].
Laboratory investigations.
| Laboratory test | Values | Reference range | Lab values after 21 days |
|---|
| Serum amylase (U/L) | 1724 | 20-110 | 37 |
| Serum lipase (U/L) | 1200 | <200 | 64 |
| Serum triglycerides (mg/dL) | 155 | <150 | - |
| Serum alkaline phosphate (IU/L) | 278 | 64-300 | - |
| Neutrophils (%) | 78.6 | 60% | - |
| Total bilirubin (mg/dL) | 2.0 | 0.1-1.2 | - |
| Direct bilirubin (mg/dL) | 1.1 | 0.3 | - |
| Aspartate aminotransferase (U/L) | 178 | 8-33 | 10 |
| Haemoglobin (mg/dL) | 11.5 | 13.2-16 | |
| Alanine aspartate aminotransferrase (ALT) (IU/L) | 666 | 7-35 | 28 |
| Serum calcium (mg/dL) | 8.1 | 9.0-10.8 | - |
| Serum albumin (g/dL) | 3.6 | 3.5-5.0 | - |
Showing Contrast-enhanced Computerised Tomography (CECT).
Ultrasonography of abdomen and pelvis.
Differentiating between acute pancreatitis and other conditions like acute ulcer disease, cholangitis, cholecystitis, biliary colic, and duodenal ulcer can be challenging, as these conditions can present with similar symptoms. Acute pancreatitis was differentiated from other conditions by using typical clinical features, diagnostic criteria, and the Atlanta criteria. The diagnosis of pancreatitis was confirmed by meeting all three of the Atlanta criteria: the presence of symptoms consistent with pancreatitis (such as gastric pain), elevated serum amylase levels (three times above the normal value), and radiological features indicative of acute pancreatitis, as observed in the abdominal ultrasound [1].
Management
Management was divided into two parts: Shodhana Chikitsa and Shamana Chikitsa, along with dietary modification [Table/Fig-4,5]. The Shodhana plan involved the use of Matrabasti for Shodhana treatment. Matrabasti (100 mL) was administered with Dashmool oil after meals daily for eight days. The patient approached the Department with complaints of epigastric pain, nausea, and vomiting, and was diagnosed with acute pancreatitis. He was treated with Shodhana and Shamana Chikitsa.
Details of Shamana and Shodhana chikitsa.
| No. | Aushadi (internal medicine) | Dose and duration | Time | Annupana |
|---|
| 1 | Avipattikar Choorna | 1 gm continued for 21 days | After meal at night | Lukwarm water |
| 2 | Sutshekhar Rasa | 250 mg for 21 days | BD 1/2 hr before meal | Lukwarm water |
| 3 | Amlaki Choorna | 1 gm daily for 21 days | OD 1/2 hrs Breakfast | Honey or water |
| 4 | Shankhvati | 250 mg for 21 days | BD after meal | Lukewarm water |
| 5 | Yashtimadhu Choorna | 1 gm for 21 days | BD after meal | Takra |
| 6 | Tab. Mentocalm | 1 tab BD for 21 days | After meal | Water |
Pathya/Apathya (Do’s and Don’t).
| Types | Pathya (Do’s) | Apathya (Don’t) |
|---|
| Cereals | Old shali rice | Wheat |
| Pulses | Green gram (mudga), Pigeon pea, masura | Peas (matara) |
| Fruits and vegetables | Water chestnut (singhada) banana, jambo (jambu) | Garlic (Lahasuna) |
| Other | Without cream curd, goats milk, clarified butter, sesame oil | Betel nut, sour vinegar (kanji) jaggery, sour food |
| Honey, soup (yusa), butter milk, cumin, coriander | Spicy food |
| Life style | Therapeutic emesis (vaman) | Night awakening, suppression of natural urges, physical exercise |
After 7-8 days of treatment, the patient started responding and the symptoms gradually decreased. After a complete 21 days of treatment, there was a significant reduction in laboratory values: serum amylase was 37 U/L, serum lipase was 64 U/L, serum aminotransferase was 10 U/L, and Alanine Aspartate Aminotransferase (ALT) was 28 IU/DL. On follow-up after 21 days, the patient was completely cured of all symptoms, and no recurrence was observed. After three months of follow-up, the parents expressed high satisfaction with the treatment provided, with no adverse effects observed.
Discussion
Pancreatitis is a condition where inflammation of the pancreas leads to severe abdominal pain, nausea, vomiting, fever, and anorexia. The severity of symptoms not only disturbs the overall quality of life but also affects the parents of the patient. This patient experienced episodes of recurrent abdominal pain. The diagnosis was confirmed as Grahani Roga (Acute Pancreatitis) through radiological and laboratory investigations. Pancreatitis is primarily an inflammatory condition. Grahani Roga falls under Pittaj Vikara.
The Samprapti Ghataka Vighatana (breaking the aetiopathogenesis) was taken into consideration, and a plan for Mrudu Virechana (mild purgation) using Avipattikar Churna was established. Mridu Virechana pacifies the vitiated Pitta, making it effective for this patient [2]. The principles of treatment include Mridu Virechana (mild purgation) and the use of formulations that are hepatostimulant (Yakrutottejaka) and pancreatic-protecting (Pramehaaghna) [3].
Grahani Roga is a common Gastrointestinal (GI) tract disorder that negatively impacts day-to-day functioning. The primary functional component of Mahasrota, situated between Amashaya (stomach) and Pakwashaya (large intestine), is called Grahani. It is also referred to as the Pittadhara Kala, where Jatharagni (digestive fire) resides. Its primary role is to retain the ahara (food) until the end of Avasthapaka (digested food) and then transfer it to Pakwashaya (large intestine) [4].
The pathophysiology of pancreatitis can be linked to VatajaGrahani Dosha. Considering the prominence of Dhatu and Dosha (body tissue), the main goals of therapy were to control the signs, protect the pancreatic structure and function from further alterations, and return the biochemical values to normal [5].
Action of Internal Medicine
Avipattikar Choorna: In clinical practice, Grahani disease is a commonly seen condition. The primary pathogenic mechanism behind the emergence of this disease is believed to be the excess formation of vitiated Pitta (Pitta Drava Guna Vriddhi) as a result of inappropriate food and lifestyle behaviours [6]. For its efficient administration, traditional Ayurvedic formulations like Avipattikar Choorna and Sutasekhar Rasa are frequently administered in combination. For the treatment of Urdhwaga Amlapitta, Avipattikar Choorna and Sutasekhar Rasa work incredibly well together, and there are no adverse effects from either medication. Additionally, patients who adhere to the Pathya (recommended regimen) and avoid the Apathya (prohibited foods and behaviours) recover more quickly and have a lower likelihood of recurrence [7].
Sutasekhar Rasa: Ayurvedic practitioners employ Sutasekhar Rasa, a formulation that is useful in treating conditions such as hyperacidity in Amlapitta, digestive impairment in Agnimandya, diarrhoea in Atisara, abdominal lumps in Gulma, cough in Kasa, malabsorption syndrome in Grahani, and tuberculosis in Rajayakshma. In the literature, there are four different formulations with the same name and one Laghu Sutasekhar Rasa. Of all these, the Sutasekhar Rasa, as described in Yoga Ratnakara, is well-known and has been used in medicine and trade [8].
Amlaki Choorna: Fruit extracts from E. officinalis have been shown to have strong immunomodulatory effects. Amalaki has demonstrated mild cytoprotective efficacy as well as immunostimulant action. Nevertheless, Amalaki Choorna and Amalaki Swaras must be triturated in order to obtain the desired pharmacological activity [9].
Shankh Vati: A well-known traditional Ayurvedic medicine called Shankh Vati is frequently used to treat a variety of ailments, including stomach pain, constipation, haemorrhoids, acid reflux disease, and hyperacidity caused by digestive problems [10]. There are fifteen variations of Shankh Vati that can be found in various Ayurvedic texts. The variations share the same ingredients: Shankha Bhasma, Hingu, Vatsanabha, Trikatu, Kshara, and Lavana, best for gastric pain management [11].
Yashtimadhu Choorna, derived from Yastimadhu (Glycyrrhiza Glabra), is used in the treatment of chronic acidity, ulcers, and chronic bronchial conditions. Yashtimadhu is known to balance both Vata and Pitta doshas. Studies conducted on modern scientific parameters have proven the healing, anti-inflammatory, and anti-ulcer properties of Yashtimadhu [12].
Takra: Based on the systems and areas of the Gastrointestinal (GI) system affected, GI diseases can be classified as Functional Gastrointestinal Disorders (FGIDs) in the absence of an organic cause. Probiotics, often referred to as “good” or “helpful” bacteria, support gut health. Probiotics have been thoroughly researched in relation to GI illnesses such as antibiotic-associated diarrhoea and infectious gastroenteritis. Takra can be regarded as an ayurvedic probiotic as it is fermented and has been used for generations in treating conditions like Grahani. According to thorough studies, Takra offers several advantages, particularly in boosting beneficial bacteria in the GI tract, which in turn reduces harmful bacteria and is crucial for maintaining tract health. Including Takra in regular meals supports intestinal immunity and helps prevent GI illnesses [13,14].
Sutshekhar Rasa is considered the best Pittashamaka medicine in Ayurveda. Matrabasti with til taila acts as Vatashamana. Pain is mostly associated with Vata Dosha, so the use of Matrabasti has been found to be effective. Sankh Vati is effective in alleviating abdominal pain due to its Ushna Guna. Amlaki Churna and Yashtimadhu Churna are used as Rasayana drugs. Yashtimadhu Churna is an excellent Ropak dravya, and its healing properties help reduce inflammatory conditions and alleviate pain.
Conclusion(s)
Virechana (purgation) played a crucial role in the management of Grahani Roga (Acute Pancreatitis). Shamana Aushadhi, along with Pathya and Apathya according to Dosha-Dushya samurshana, was effective in treating the patient. From present case study, it can be concluded that Grahani Roga (Acute Pancreatitis) was effectively managed by Virechana as shodhana chikitsa and Shamana Chikitsa, along with Pathya and Apathya, without any complications or side effects. No adverse drug reactions were observed, and the patient was satisfied with the treatment.
[1]. Pfleger R, Niknejad M, Shah V, Revised Atlanta classification of acute pancreatitisReference article, Radiopaedia.org (Accessed on 02 Aug 2024)10.53347/r-28902 [Google Scholar] [CrossRef]
[2]. Sokiya G, Painuly P, Negi M, Sharma G, An Ayurvedic approach towards management of acute pancreatitis: A case studyJ Ayurveda Integr Med Sci 2012 9(4):310-15.Available from: https://doi.org/10.21760/jaims.9.4.5210.21760/jaims.9.4.52 [Google Scholar] [CrossRef]
[3]. Patil S, An ayurvedic management of pancreatitis with special reference to grahani- A case studyInternational Journal of Creative Research Thoughts 2024 12(3):1143-62. [Google Scholar]
[4]. Chakraborty S, Das A, Management of grahani roga in ayurveda: A case studyWorld Journal of Pharmaceutical Research 2021 9(15):953-61.10.20959/wjpr202015-19220 [Google Scholar] [CrossRef]
[5]. GaMne R, Wajpeyi SM, Nara V, Mandal S, Role of Madhutailik basti and Shaman chikitsa Section in the management of acute on chronic pancreatitis: Internal medicine: A case reportJ Clin Diagn Res 2024 18(5):OD04-06.10.7860/JCDR/2024/68122.19360 [Google Scholar] [CrossRef]
[6]. Jain S, Chawardol SG, Jain J, Dwivedi OP, Management of Grahani Roga by Ayurveda principles and life style modificationJ Drug Delivery Ther 2018 8(6):393-96.10.22270/jddt.v8i6.2061 [Google Scholar] [CrossRef]
[7]. Chaturvedi A, Nath G, Yadav VB, Antiwal M, Shakya N, Swathi C, A clinical study on Virechana Karma (therapeutic purgation) over the gut flora with special reference to obesityAyu 2019 40(3):179-84.10.4103/ayu.AYU_302_1933281395PMC7685265 [Google Scholar] [CrossRef] [PubMed]
[8]. Kumar A, Singhal T, Scientific explanation of mode of action of sutshekhar ras in amlapitta with special reference to acid peptic disorders: A reviewInt J Res Ayurveda Pharm 2018 9(5):47-49.10.7897/2277-4343.095154 [Google Scholar] [CrossRef]
[9]. Sharma OP, Sharma S, A critical review of Amalaki- (Emblica Officinalis Gaertn.) in classical texts and promote its use in our lifeInt J Ayur Pharma Res 2022 10(7):91-98.10.47070/ijapr.v10i7.2412 [Google Scholar] [CrossRef]
[10]. Kodlady N, Varieties in Shankha Vati- An Ayurvedic classical formulation for GIT disordersAnnals of Ayurvedic Medicine 2012 4(3):102-08.10.53730/ijhs.v6ns2.5138 [Google Scholar] [CrossRef]
[11]. Dukare P, Rathi B, Rathi R, Madan P, Therapeutic potential of formulations of Shankha Bhasma described in Bharat Bhaishajya RatnakarInternational Journal of Health Sciences 2022 6(S2):580-93.10.53730/ijhs.v6nS2.5036 [Google Scholar] [CrossRef]
[12]. Heliben JS, A comprehensive review on yashtimadhu (glycyrrhiza glabra linn.) from brihattrayi with special reference to KalpanaJ Pharma Sci Innov 2020 9(3):88-94.10.7897/2277-4572.093175 [Google Scholar] [CrossRef]
[13]. Zhang YJ, Li S, Gan RY, Zhou T, Xu DP, Li HB, Impacts of gut bacteria on human health and diseasesInt J Mol Sci 2015 16(4):7493-519.10.3390/ijms1604749325849657PMC4425030 [Google Scholar] [CrossRef] [PubMed]
[14]. Shaikh SD, Sun N, Canakis A, Park WY, Weber HC, Irritable bowel syndrome and the gut microbiome: A comprehensive reviewJ Clin Med 2023 12(7):2558Available from: https://doi.org/10.3390/jcm1207255810.3390/jcm1207255837048642PMC10095554 [Google Scholar] [CrossRef] [PubMed]