Pericardial Effusion as a First Symptom of Thymoma: A Case Report
Suprit Malali1, Sourya Acharya2, Samarth Shukla3, Sunil Kumar4, Priti Mishra5
1 Junior Resident, Department of Internal Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Medical Education and Research, Sawangi, Meghe, Wardha, Maharashtra, India.
2 Professor, Department of Internal Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Medical Education and Research, Sawangi, Meghe, Wardha, Maharashtra, India.
3 Professor, Department of Pathology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Medical Education and Research, Sawangi, Meghe, Wardha, Maharashtra, India.
4 Professor, Department of Internal Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Medical Education and Research, Sawangi, Meghe, Wardha, Maharashtra, India.
5 Senior Resident, Department of Pathology, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Medical Education and Research, Sawangi, Meghe, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Suprit Malali, Junior Resident, Department of Internal Medicine, Jawaharlal Nehru Medical College, Datta Meghe Institute of Higher Medical Education and Research, Sawangi, Meghe, Wardha-442004, Maharashtra, India.
E-mail: supritbm@gmail.com
Thymomas, which account for 25% of all mediastinal tumours, primarily originate from the anterior mediastinum and tend to grow slowly, often being incidentally discovered during radiographic investigations. The clinical spectrum of thymoma ranges from asymptomatic incidental findings to the development of paraneoplastic syndromes and symptoms caused by local or metastatic involvement. Myasthenia Gravis symptoms may also be present, and in some cases, manifestations can arise due to pressure on adjacent structures. However, pericardial effusion as an initial and early presenting feature of thymoma remains extremely rare. In advanced and disseminated cases, pericardial and pleural effusions may occur. Therefore, it is crucial to consider the possibility of a concealed cardiac silhouette mimicking pericardial effusion in asymptomatic patients, ensuring a comprehensive evaluation. The current report represents a case study of a 56-year-old female patient with a history of subacute and progressive dyspnoea. Despite no significant positive clinical findings upon general and systemic examination, the diagnostic work-up revealed a modest pericardial effusion attributed to an unexpected thymoma. The present case highlights the unusual clinical manifestation, emphasises the diagnostic challenges involved, and underscores the importance of considering thymoma in the differential diagnosis of pericardial effusions.
Dyspnoea, Mass, Mediastinal, Myasthenia gravis
Case Report
A 56-year-old female patient, a homemaker with no co-morbidities, presented with a four-month history of dyspnoea. Initially, she experienced dyspnoea during routine activities but gradually progressed to experiencing dyspnoea even during minimal exertion tasks {New York Heart Association (NYHA) grade 2-3} [1]. She did not experience dyspnoea at rest and was not taking any medication for it. The patient had no prior history of fever, cough, haemoptysis, oedema, paroxysmal nocturnal dyspnoea, orthopnea, or platypnea. Physical examination revealed afebrile status, blood pressure of 100/60 mmHg, a regular pulse rate of 104 beats per minute, and no signs of pallor, icterus, cyanosis, or oedema. The Jugular Venous Pressure (JVP) was not elevated (11 cm). Cardiovascular examination revealed soft first and second heart sounds without murmurs, and respiratory examination revealed bilateral equal air entry and normal vesicular breath sounds with no added adventitious sounds. Abdominal examination disclosed soft, tender hepatomegaly.
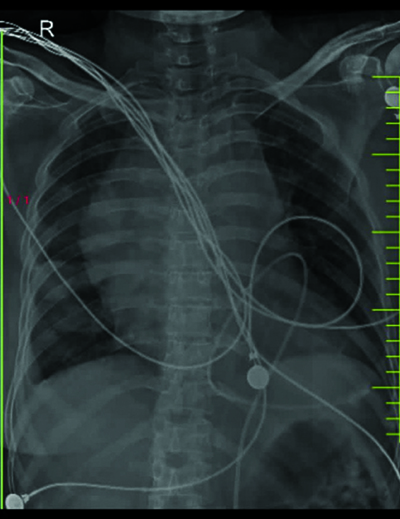
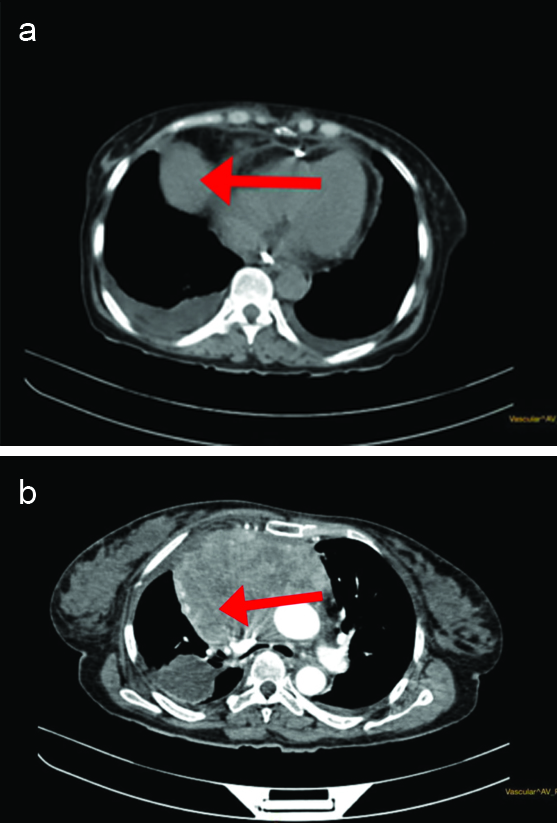
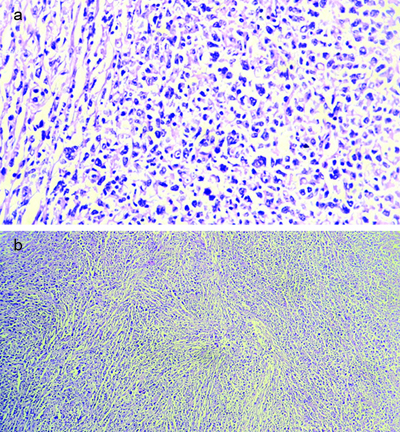
Laboratory findings showed a haemoglobin level of 12 g/dL, an elevated Erythrocyte Sedimentation Rate (ESR) of 42 mm in the first hour, C-reactive Protein level of 34 g/dL, and a Total Leukocyte Count (TLC) of 6,700/mm3. An Electrocardiogram (ECG) showed sinus tachycardia with low-voltage complexes. Chest X-ray revealed mediastinal widening and cardiomegaly. Notably, [Table/Fig-1] a chest Computed Tomography (CT) scan unveiled a significant anterior mediastinal mass accompanied by a minor pericardial effusion [Table/Fig-2a,b]. A 2D Echocardiogram (Echo)-guided pericardiocentesis extracted 1,200 cc of haemorrhagic fluid with a pericardial fluid hematocrit value of 38.6%. Additionally, a Ultrasonography (USG)-guided biopsy of the mediastinal tumour confirmed the diagnosis of thymoma [Table/Fig-3a,b].
Chest X-ray showing cardiomegaly and mediastinal widening.
High Resolution Computed Tomography (HRCT) thorax and CT pulmonary angiography.
Showing a well-defined large minimally and heterogeneously enhancing soft-tissue attenuation space-occupying lesion notes in anterior mediastinum suggestive of thymic neoplasia, irregular thickening of the pericardium with moderate pericardial effusion with bilateral minimal pleural effusion
Slides show the presence of partial capsule; cells are polygonal in shape with scanty cytoplasm. Sections also show intersecting fibrous bands and the presence of lymphocytes (thymocytes). Features suggestive of thymoma (Haematoxylin and Eosin 40x and 10x, respectively).
A multidisciplinary team, including Cardiovascular and Thoracic Surgeons (CVTS), advised against tumour resection due to substantial pleural and pericardial involvement, categorising the patient’s case as Stage III, denoting pleural and pericardial invasion. Consequently, the patient was initiated on chemotherapy employing the Cyclophosphamide, Adriamycin and cis-Platinum (CAP) regimen, which included cyclophosphamide (500 mg/m2), adriamycin (20 mg/m2/day 24-hour infusion), and cis-Platinum (30 mg/m2).
The patient failed to attend the scheduled follow-up appointment for radiotherapy.
DISCUSSION
In the present case, the present patient exhibited a rare clinical entity, presenting with bilateral mild pleural effusion and spontaneous, asymptomatic pericardial effusion, as supported by a review of the existing literature [1-3]. Thymomas are rare mediastinal tumours, with an incidence of 0.15 cases per 100,000 individuals [2].
Patients with thymoma may be asymptomatic or experience pressure-related symptoms such as chest pain, dysphagia, dyspnoea, and Superior Vena Cava (SVC) syndrome. Pericardial effusion, an early sign observed in approximately 20% of cases, was also present in the patient [3].
A retrospective study reported that pericardial disease can be the initial presentation of an underlying malignancy in approximately 7.5% of cases. This suggests that a significant proportion of patients presenting with pericardial disease may have an underlying malignancy. However, it is important to note that this figure is not absolute certainty and may vary in different clinical contexts [4].
Another study investigated the likelihood of detecting neoplastic disease when pericarditis or a small pericardial effusion is the initial presentation. The present study found that the probability of identifying a neoplastic condition in such cases was relatively lower, ranging from 4% to 7%. However, it is worth noting that the likelihood of uncovering neoplastic disease increased substantially in cases involving large pericardial effusions, with a range of 23% to 33% [5]. In the present case, the patient had a moderate pericardial effusion, posing a diagnostic dilemma.
Benign thymic tumours can lead to pericardial effusions due to their mass effect, as shown in research conducted by Nishi T et al., [6]. Due to the rarity and histological diversity of thymoma, the Masaoka staging system is widely used for classification and prognostication [7]. It significantly contributes to treatment decision-making. In the present patient’s case, the tumour invasion into adjacent organs categorised it as Stage III (pleural and pericardial invasion).
Complete surgical excision remains the primary therapeutic approach for resectable thymomas. High-risk tumours at stages I and II {Tumour, Node, Metastasis (TNM) Staging} typically require postoperative radiotherapy following tumour resection [8]. For stage IIIA tumours, surgical management, either initially or following neoadjuvant chemotherapy, is recommended. Stage IIIB tumours may require a combination of radiation, chemotherapy, and/or surgery. In the present case, chemotherapy was prioritised due to the Stage III classification. Ongoing phase II studies suggest that immunotherapy with Pembrolizumab holds promise for thymic tumours [9].
CONCLUSION(S)
The patient presented with a rare clinical phenomenon of bilateral mild pleural effusion accompanied by spontaneous and asymptomatic pericardial effusion. It is crucial to maintain awareness of atypical presentations like this, which manifest as pericardial effusion, in order to facilitate prompt diagnosis and initiation of therapeutic interventions. The present case report emphasises the importance of excluding alternative causes of massive pericardial effusions, such as idiopathic, drug-induced, tuberculosis-related, or radiation-induced pericarditis. Instead, it highlights the significance of considering thymoma as a potential differential diagnosis in cases of pericardial effusion. The optimal management approach for thymoma with pericardial effusions remains uncertain. These cases tend to have a less favourable prognosis with a higher recurrence rate. Continued reporting of similar case studies is crucial to enhance the understanding of the presentation and clinical bahaviour of these tumours.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Aug 14, 2023
Manual Googling: Nov 16, 2023
iThenticate Software: Nov 18, 2023 (3%)
[1]. Zhang R, Ma S, Shanahan L, Discovering and identifying New York Heart Association classification from electronic health recordsBMC Med Inform DecisMak 2018 18(Suppl 2):4810.1186/s12911-018-0625-730066653PMC6069768 [Google Scholar] [CrossRef] [PubMed]
[2]. Khan A, Jain AG, FaisalUddin M, Khetpal N, D’Souza J, Cardiac tamponade in the setting of a thymomaCureus 2019 11(6):e495210.7759/cureus.4952 [Google Scholar] [CrossRef]
[3]. Moady G, Daud E, Galilee R, Sabo E, Mazareb S, Atar S, Pericardial effusion in a young man: A rare presentation of thymomaIsr Med Assoc J 2020 22(5):328-29. [Google Scholar]
[4]. Shomron BH, Ijan B, Victor G, Large symptomatic pericardial effusion as the presentation of unrecognised cancer: A study in 173 consecutive patients undergoing pericardiocentesisMedicine (Baltimore) 2006 85(1):49-53.10.1097/01.md.0000199556.69588.8e16523053 [Google Scholar] [CrossRef] [PubMed]
[5]. Ceuninck MD, Demedts I, Trenson S, Malignant cardiac tamponadeActa Cardiol 2013 68(5):505-07.10.1080/AC.68.5.299447424283112 [Google Scholar] [CrossRef] [PubMed]
[6]. Nishi T, Takamori S, Muta F, Yoshiyama K, Iwasaki Y, Shirouzu K, Nonmalignant pericardial effusion associated with thymic cancerGen Thorac Cardiovasc Surg 2010 58(5):239-42.10.1007/s11748-009-0506-120449715 [Google Scholar] [CrossRef] [PubMed]
[7]. Masaoka A, Staging system of thymomaJ Thorac Oncol 2010 5(10 Suppl 4):S304-12.10.1097/JTO.0b013e3181f20c0520859124 [Google Scholar] [CrossRef] [PubMed]
[8]. Detterbeck FC, Stratton K, Giroux D, The IASLC/ITMIG Thymic Epithelial Tumours Staging Project: Proposal for an evidence-based stage classification system for the forthcoming (8th) edition of the TNM classification of malignant tumoursJ Thorac Oncol 2014 9(9 Suppl 2):S65-72.10.1097/JTO.000000000000029025396314 [Google Scholar] [CrossRef] [PubMed]
[9]. Giaccone G, Kim C, Thompson J, Pembrolizumab in patients with thymic carcinoma: A single-arm, single-center, phase 2 studyLancet Oncol 2018 19(3):347-55.10.1016/S1470-2045(18)30062-729395863 [Google Scholar] [CrossRef] [PubMed]