The employment of tourniquet to achieve bloodless surgical field is an essential step, especially in upper/lower extremity orthopaedic surgical procedures. However, tourniquet itself can lead to many possible problems, posing challenges to the anaesthesiologists. One such is exaggerated hypertensive response sometime after inflation of tourniquet, aptly termed as Tourniquet-induced Hypertension (TIH/T-HTN). It may not be evident in some patients, but if and once established, it becomes practically impossible to minimise/reverse it. This can be a nightmarish experience for the anaesthesiologist concerned. The authors hereby present one such case where, a young, healthy 25-year-old male posted for arthroscopy of right knee, who was administered subarachnoid block with dexmedetomidine as an adjuvant to bupivacaine. Within 35 to 40 minutes of inflating the torniquet, he developed severe hypertensive response, with blood pressures ranging from a Systolic Blood Pressure (SBP) of 190 to 210 mmHg and a Diastolic Blood Pressure (DBP) of 118 to 125 mmHg. It remained unresponsive to any form of treatment, including, the sedation with Inj. Midazolam or incremental doses of Inj. Labetalol. The hypertension persisted throughout the duration of surgery, while patient remained comfortably asleep. However, at the end of the surgical procedure, as soon as the tourniquet was deflated, the Blood Pressures (BPs), both SBP and DBP dropped to baseline values. Also, includes an in-depth review of the available literary evidence about this phenomenon and provided specific deductions and recommendations/remedial measures.
Case Report
A 25-year-old male weighing 72 kg presented with history of domestic fall one year back. There was no significant past medical history except for chronic alcohol consumption, about 250-300 mL daily for the last 4-5 years. Magnetic Resonance Imaging (MRI) confirmed Anterior Cruciate Ligament (ACL) tear with moderate effusion in the right knee joint and patient was posted for arthroscopic reconstruction of ACL.
Pre-anaesthetic examination was essentially normal, with Body Mass Index (BMI) of 22 kg/m2 and blood pressure of 110/86 mmHg. All the routine investigations were within normal limits. He was considered as American Society of Anaesthesiologists (ASA) I and planned under subarachnoid block.
On the operating table, patient was comfortable, with pulse rate of 89/min and blood pressure of 180/109 mmHg. After waiting for five minutes, the BP came perceptibly down, to 134/88 mmHg. Intravenous access was secured with 20 G cannula. Patient was made to sit up and under all sterile precautions, with median approach in L3-L4 space with help of 25 G Quincke’s needle to subarachnoid block was achieved using Injection Bupivacaine 0.5% heavy (3.4 mL)+dexmedetomidine (12 micrograms) for a total volume of 3.6 mL. The patient was then made supine and level of sensory block was achieved up to T10 segment.
The pulse rate gradually dropped and settled down between 52-58/min. However, blood pressure remained slightly on the higher side (130-135/80-84 mmHg). This trend continued throughout, application of tourniquet on the right thigh (which was not inflated yet), as well as during the painting, cleaning and draping of the area. The tourniquet was inflated to 280 mmHg.
After 35-40 minutes, blood pressure began to rise, reaching levels up to 210/125 mmHg (ranging between, SBP of 190-210 mmHg and DBP of 118-125 mmHg). The pulse rate varied between 48-89/min. Inj. Midazolam was administered in the incremental doses of 0.5 mg up to a total of 1.5 mg. Inj. Labetalol 20 mg was given in titrated incremental doses of 5 mg each was given over nearly 30-35 minutes. There was absolutely no decrease in the BP levels; however, the patient was comfortably sleeping and snoring.
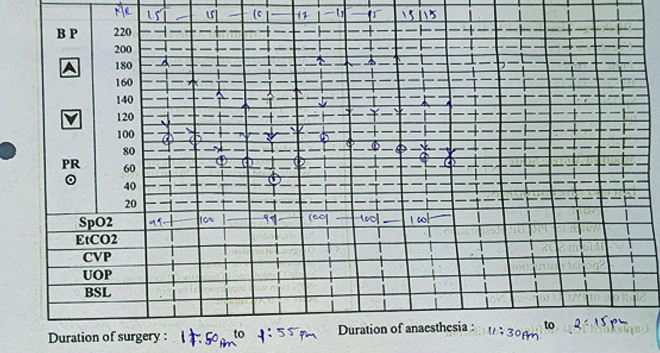
Blood pressure continued to rise relentlessly inspite the authors efforts to bring it down. At this point, the procedure was over and the tourniquet was deflated. Within 1-2 minutes, blood pressure decreased on its own to 136/78 mmHg and the pulse rate settled at 71/min [Table/Fig-1]. By the time the patient was shifted to Post Anaesthesia Care Unit (PACU), the BP and pulse had stabilised to 122/80 mmHg and 59/min, respectively.
Blood pressure normalising within few minutes of deflation of torniquet.
The patient was monitored for two hours and, after an uneventful recovery, was transferred out of PACU. The Visual Analogue Scale (VAS) at that time was two and the patient remained pain-free until late evening. The patient remained haemodynamically stable throughout the postoperative period and was discharged from the hospital next afternoon.
Discussion
The process of exsanguination of the limb and an application of the tourniquet on the upper/lower extremity is an essential modality for minimising the blood-loss during surgery/trauma [1]. Originally, a screw-like device was invented in 1718 by a French surgeon Louis Petit to minimise blood loss during lower limb amputations. It derived the name from a French verb ‘tourner,’ which literally means ‘to turn [1,2].’ A version of rubber bandages was introduced in 1873 by Johann Friedrich August von Esmarch, which is still used today as Esmarch’s bandage [2,3]. The first pneumatic tourniquet was introduced by Harvey Cushing in 1904 and evolved into the modern-day pneumatic tourniquets [2]. In earlier years, tourniquets were also used for achieving Intravenous Regional Anaesthesia (IVRA/Bier’s Block) [4].
Few reported untoward effects are tourniquet pain, post-tourniquet-induced muscle/neurovascular injury, metabolic and electrolyte disturbances, rise in end-tidal Partial pressure of Carbon dioxide (PCO2) and, most importantly, hemodynamic disturbances in the form of rise in SBP, DBP, Mean Arterial Pressure (MAP) and heart rate [1,5-7]. Recently, a study confirmed significant rise in Intracranial Pressure (ICP) after deflation of tourniquets in patients where the Tourniquet Time (TT) exceeded 67.5 minutes [8].
A severe intraoperative hypertensive response to inflation of torniquet especially under neuraxial (spinal) anaesthesia, is an uncommon phenomenon. The commonality of chronology of events, as observed in the present case, BP generally starts rising anywhere between 35 to 60 minutes after the inflation of the tourniquet. The rise is seen in all the three forms of blood pressure-SBP, DBP and MAP-as well as heart rate, by more than 30% from the baseline and is generally not amenable to routine measures like, sedation or antihypertensives like β-blockers, α and β-blockers, or even centrally acting α2 agonists.
The striking finding is the spontaneous and complete disappearance of this response within few minutes of deflation of tourniquet, as was evident in the present case. Factors like, TT, patient factors like older age and pre-existence of hypertension have been suspected to be contributory. Tourniquet Pressure (TP) may not have much role to play, especially in the rise in ICP [8].
Bradford EMW (1969) first reported “haemodynamic changes associated with the application of lower limb tourniquets in patients undergoing orthopaedic procedures.” Apparently, on application of a lower limb tourniquet, there was congestion in the neck and face. She concluded that there was significant rise in central venous pressure and there was mild to moderate rise in SBP/DBP (18-19 mmHg). However, it should be noted that the surgeries were completed within 60 to 90 minutes. So mild to moderate rise may have been just the beginning of the process, which was aborted by the release of the tourniquet at the end of relatively quicker surgical procedures [9].
The first reported study was by Kaufman RD and Walts LF (1982). A retrospective review of total of 600 lower limb surgeries with inflation of tourniquet after anaesthetic (n=500) concluded that 55 (11%) showed a hypertensive response irrespective of the anaesthetic used (halothane, enflurane, nitrous oxide, narcotic, or regional), which disappeared after deflation. In comparison, in the control group where the tourniquet was not used (n=100), only 1 (1%) of the patients showed a hypertensive response. They postulated that this might be due to tourniquet pain, because of occurrence of both phenomena occurred after 45 minutes of tourniquet inflation. However, they did not provide any pertinent explanation. Nonetheless, they coined the term ‘Tourniquet-induced Hypertension’ (TIH) [10].
After encountering TIH and facing the mortality in elderly, obese and hypertensive patient for lower limb surgery under General Anaesthesia (GA), Valli H et al., conducted a study on 699 patients and found higher incidence of TIH associated with the factors like, older age, lower limb surgery, longer duration, GA, or Intravenous Regional Anaesthesia (IVRA), rather than spinal or brachial block [11]. Tetzlaff JE et al., provided the definition of T-HTN as ‘rise of the BP (any parameter or all) by 30% above baseline after the inflation of the tourniquet’ [12].
Surprisingly, the modality of anaesthesia, such as GA, IVRA, or neuraxial block (subarachnoid/epidural or combination), does not have any effect on this phenomenon. These reports also describe administration of multiple drugs preemptively to control these untoward effects, like, preoperative or intraoperative infusions of low-dose ketamine [13-17], magnesium [17,18], lidocaine [19], amantadine [20], clonidine [21,22] and, latest the spate of reports on dexmedetomidine [23-27].
In spite of these and many other articles on this issue, there is no known aetiology. Some theories/hypotheses are as follows:
Due to exsanguination of one limb, the blood from that limb expands the central venous volume and also somehow increases the systemic vascular resistance, to which may contribute to the tourniquet-related pain and the ischaemia of the limb [15].
Tourniquet-induced hypertension (TIH/T-HTN) is mediated through N-Methyl D-Aspartate (NMDA) receptor activation because of noxious stimuli from the extremity, which might be the reason why NMDA antagonists like ketamine, amantadine, or magnesium sulphate might minimise this response in some patients [13,17,18,20].
Possible ischaemic pain mediated through ‘C’ fibres due to obtundation of ‘Aδ’ fibers after 40-45 minutes of tourniquet time, leading to an exaggerated sympathetic response [6,10]. The suppression of this seems to be the mechanism of action of α2 agonists, dexmedetomidine or clonidine.
At present, preoperative infusion of dexmedetomidine is considered to be most effective panacea for tourniquet-induced reperfusion injury, tourniquet pain and everything related to tourniquets [23-27].
Against this background, the present case appears to be unique. The patient was a young male with no significant history or preoperative problems, except for a history of chronic alcohol intake. During administration of subarachnoid block, the authors added dexmedetomidine as an adjuvant to bupivacaine and as expected, all the features of dexmedetomidine-enhanced subarachnoid block began to establish until the onset of Tourniquet-Induced Hypertension (TIH). Therefore, even its presence could not prevent the process. One can deduce that dexmedetomidine acts purely centrally in subarachnoid block, with no systemic effects. This is corroborated by all the reported studies/reports where specifically, dexmedetomidine has to be infused preoperatively to have any effect.
It also confirms that once the process has been initiated, any drug-whether benzodiazepines, opioids, lidocaine, ketamine, β-blockers, even centrally acting α2 agonists, cannot reverse or control it. One might consider allowing the process to go on relentlessly without intervention, as that was the only alternative left to the authors and it is expected to reverse itself momentarily upon deflation of the cuff [26]. This approach may be feasible in young, healthy patients as in present case case, who came out unscathed and recovered well. However, it might have disastrous consequences the compromised patients, as has been reported [11].
Another striking feature in the present case was that, contrary to the common occurrence of TIH in patients under GA, the present case involved a subarachnoid block. The correlation between TT and TIH was confirmed, as the TT in the present case was nearly 90 minutes.
Conclusion(s)
The TIH is a dreadful phenomenon and all the patients requiring use of a tourniquet, especially for lower limb surgeries, are potential victims. If it is going to happen, it will happen, 30-45 minutes after inflation of the tourniquet. Factors like age (including paediatric patients), gender and preoperative conditions (with a greater predisposition in hypertensive patients) do not seem to matter. The modality of anaesthesia has no control over it; TIH can occur under general, regional, neuraxial, or IVRA. It may not necessarily be due to tourniquet pain. However, TT is a very important factor. Once established, there is currently no treatment for TIH. The reported efficacy of various drugs is not curative or therapeutic in established TIH but may be preventive if infused before the establishment of TIH, especially dexmedetomidine. So, anaesthesiologists must be prepared for prevention rather than treating established TIH, which would be futile/fruitless. Lastly, Surgeon needs to be sensitised and made aware about TIH and specificity of TT.
[1]. Deloughry JL, Griffiths R, Arterial tourniquetsContinuing Education in Anaesthesia Critical Care & Pain 2009 9(2):56-60.Available from: https://doi.org/10.1093/bjaceaccp/mkp00210.1093/bjaceaccp/mkp002 [Google Scholar] [CrossRef]
[2]. Kam PCA, Kavanaugh R, Yoong FFY, The arterial tourniquet: The pathophysiological consequences and anaesthetic implicationsAnaesthesia 2001 56:534-45.10.1046/j.1365-2044.2001.01982.x11412159 [Google Scholar] [CrossRef] [PubMed]
[3]. Description of Esmarch bandages from en.wikipedia.org [Internet][cited 18th Aug 2022]. Available from: https://en.wikipedia.org/wiki/Esmarch_bandage [Google Scholar]
[4]. Holmes CM, The history and development of intravenous regional anaesthesiaActa Anaesthesiologica Scandinavica. Supplementum 1969 13(s36):11-18.10.1111/j.1399-6576.1969.tb00473.x4953013 [Google Scholar] [CrossRef] [PubMed]
[5]. Girardis M, Milesi S, Donato S, Raffaelli M, Spasiano A, Antonutto G, The hemodynamic and metabolic effects of tourniquet application during knee surgeryAnaesth Analg 2000 91:727-31.10.1213/00000539-200009000-00043 [Google Scholar] [CrossRef]
[6]. Estebe JP, Davies JM, Richebe P, The pneumatic tourniquet: Mechanical, ischaemia reperfusion and systemic effectsEur J Anaesthesiol 2011 28(6):404-11.10.1097/EJA.0b013e328346d5a921502865 [Google Scholar] [CrossRef] [PubMed]
[7]. Dickson M, White H, Kinney W, Kambam JR, Extremity tourniquet deflation increases end-tidal pCO2Anaesth Analg 1990 70:457-58.10.1213/00000539-199004000-000202107775 [Google Scholar] [CrossRef] [PubMed]
[8]. Besir A, Tugcugil E, Does tourniquet time or pressure contribute to intracranial pressure increase following tourniquet application?Med Princ Pract 2019 28:16-22.10.1159/00049511030396181PMC6558323 [Google Scholar] [CrossRef] [PubMed]
[9]. Bradford EMW, Haemodynamic changes associated with the application of lower limb tourniquetsAnaesthesia 1969 24(2):190-97.10.1111/j.1365-2044.1969.tb02837.x5774710 [Google Scholar] [CrossRef] [PubMed]
[10]. Kaufman RD, Walts LF, Tourniquet-induced HypertensionBr J A 1982 54(3):333-36.10.1093/bja/54.3.3336461346 [Google Scholar] [CrossRef] [PubMed]
[11]. Valli H, Rosenberg PH, Kyttä J, Nurminen M, Arterial hypertension associated with the use of a tourniquet with either general or regional anaesthesiaActa Anaesthesiol Scand 1987 31(4):279-83.10.1111/j.1399-6576.1987.tb02566.x3591250 [Google Scholar] [CrossRef] [PubMed]
[12]. Tetzlaff JE, O’Hara J Jr, Yoon HJ, Schubert A, Tourniquet-induced hypertension correlates with autonomic nervous system changes detected by power spectral heart rate analysisJ Clin Anaesth 1997 9(2):138-42.10.1016/S0952-8180(97)00238-99075039 [Google Scholar] [CrossRef] [PubMed]
[13]. Satsumae T, Yamaguchi H, Sakaguchi M, Yasunaga T, Yamashita S, Yamamoto S, Preoperative small-dose ketamine prevented tourniquet-induced arterial pressure increase in orthopedic patients under general anaesthesiaAnaesth Analg 2001 92:1286-89.10.1097/00000539-200105000-0003911323363 [Google Scholar] [CrossRef] [PubMed]
[14]. Ongaya J, Mung’ayi V, Sharif T, Kabugi J, A randomized controlled trial to assess the effect of a Ketamine infusion on tourniquet hypertension during general anaesthesia in patients undergoing upper and lower limb surgeryAfri Health Sci 2017 17(1):122-32.Available from: https://dx.doi.org/10.4314/ahs.v17i1.1610.4314/ahs.v17i1.1629026385PMC5636252 [Google Scholar] [CrossRef] [PubMed]
[15]. Meghare S, Shah K, Shah B, Effect of low dose ketamine hydrochloride on tourniquet induced hypertension in lower limb surgeriesIndo American Journal of Pharmaceutical Research 2018 8(12):1395-99. [Google Scholar]
[16]. Park JW, Jung YH, Baek CW, Kang H, Cha SM, Effects of low dose ketamine on tourniquet-induced haemodynamic responses during general anaesthesiaJ Int Med Res 2007 35(5):600-08.10.1177/14732300070350050417900399 [Google Scholar] [CrossRef] [PubMed]
[17]. Lee DH, Lee DL, Kim Sy, Kim JM, Lee HM, Magnesium sulphate attenuates tourniquet induced hypertension and spinal C-fos mRNA expression; a comparison with ketamineJ Int Med Res 2006 34(6):573-84.10.1177/14732300060340060217294989 [Google Scholar] [CrossRef] [PubMed]
[18]. El Shal SE, Lotfy I, Evaluation of effect of intravenous Magnesium Sulfate infusion on tourniquet induced hypertension and pain in arthroscopic knee surgery patients under epidural anesthesiaEgypt J Anaesth 2017 33(1):73-82.10.1016/j.egja.2016.08.022 [Google Scholar] [CrossRef]
[19]. El-Sayed W, Hasanein R, Intraoperative lidocaine infusion attenuates tourniquet induced hypertension in patients undergoing anterior cruciate ligament reconstruction under general anaesthesiaEgyptian Journal of Anaesthesia 2016 32(3):345-50.Available from: https://doi.org/10.1016/j.egja.2015.12.00610.1016/j.egja.2015.12.006 [Google Scholar] [CrossRef]
[20]. Abd Elmawgood A, Rashwan S, Rashwan D, Tourniquet-induced cardiovascular responses in anterior cruciate ligament reconstruction surgery under general anaesthesia: Effect of preoperative oral amantadineEgyptian Journal of Anaesthesia 2015 31:29-33.10.1016/j.egja.2014.08.001 [Google Scholar] [CrossRef]
[21]. Zalunardo MP, Serafino D, Szelloe P, Weisser F, Zollinger A, Seifert B, Preoperative clonidine blunts hyperadrenergic and hyperdynamic responses to prolonged tourniquet pressure during general anaesthesiaAnaesth Analg 2002 94:615e810.1097/00000539-200203000-0002511867385 [Google Scholar] [CrossRef] [PubMed]
[22]. Singh KR, Baghel PS, Agrawal J, Chaudhary B, Preoperative clonidine prevents tourniquet induced hypertension in upper limb orthopaedic operation during general anaesthesiaInternational Journal of Contemporary Medical Research 2016 3(10):2856-59.10.21276/aimdr.2017.3.1.AN5 [Google Scholar] [CrossRef]
[23]. Ali S, Siraj F, Athar M, Badar A, Role of low dose preoperative dexmedetomidine in preventing tourniquet induced hypertension in paediatric orthopaedic upper limb surgeries during general anaesthesiaAnn Int Med Den Res 2017 3(1):AN20-AN24.10.21276/aimdr.2017.3.1.AN5 [Google Scholar] [CrossRef]
[24]. Lao HC, Tsai PS, Su JY, Kwok TG, Huang CJ, Dexmedetomidine attenuates tourniquet-induced hyperdynamic response in patients undergoing lower limb surgeries: A randomized controlled studyJ Surg Res 2013 179(1):e99-e106.10.1016/j.jss.2012.01.00822487388 [Google Scholar] [CrossRef] [PubMed]
[25]. Lu Y, Zhang Y, Dong CS, Yu JM, Wong GT, Preoperative dexmedetomidine prevents tourniquet-induced hypertension in orthopedic operation during general anaesthesiaKaohsiung J Med Sci 2013 29(5):271-74.10.1016/j.kjms.2012.09.00623639514 [Google Scholar] [CrossRef] [PubMed]
[26]. Lund D, Utilizing Dexmedetomidine for a patient with prolonged tourniquet time to decrease sympathetic effectsNursing Capstones 2016 :192Available from: https://commons.und.edu/nurs-capstones/192 [Google Scholar]
[27]. Lee C, Lee C, So C, Lee J, Choi I, Ma X, Impact of Dexmedetomidine on tourniquet-induced systemic effects in total knee arthroplasty under spinal anaesthesia: A prospective randomized, double-blinded studyBiomed Res Int 2020 2020:4208597Available from: https://doi.org/10.1155/2020/420859710.1155/2020/420859733083465PMC7559225 [Google Scholar] [CrossRef] [PubMed]