Cavernolithiasis is defined as a calcified focus found inside a lung cavity. The patient can remain asymptomatic or exhibit non specific symptoms such as haemoptysis and recurrent chest infections. Its diagnosis poses a challenge to clinicians worldwide, making it a topic of interest. A collection of more than 190 various mycobacteria that cause infections in different body organs, especially the lungs, is collectively referred to as Non Tuberculous Mycobacteria (NTM). Hereby, authors report a rare case of cavernolithiasis in a 35-year-old-female patient with an NTM infection who was previously diagnosed and treated for Pulmonary Tuberculosis (PTB). This patient’s sputum was positive for Acid-fast Bacilli (AFB), and sputum culture showed growth of NTM species. High-resolution Computed Tomography (CT) of the thorax revealed bilateral cavitary lesions with the presence of calcified material inside the cavities. She did not require any surgical intervention and was managed conservatively. NTM infection poses a diagnostic challenge, making treatment milestones very difficult due to the complex treatment regimen involving multiple drugs administered for a prolonged period. Therefore, appropriate measures such as cessation of substance abuse, pulmonary hygiene, a nutritional diet, adherence to treatment, and regular follow-up must be taken to improve the quality of life.
Case Report
A 35-year-old female presented with complaints of cough with expectoration, fever, weight loss, and loss of appetite for 11 months. She also had episodes of expectorating stones while coughing for two to three times over the past three to four months. The patient had no known co-morbidities. She had a history of Pulmonary Tuberculosis (PTB) two years ago, for which she underwent extended antitubercular treatment consisting of three tablets of a fixed-dose combination of Isoniazid (75 mg), Rifampicin (150 mg), Pyrazinamide (400 mg), and Ethambutol (275 mg) daily for one year due to persistent symptoms and ongoing sputum positivity for acid-fast bacilli. After completing the treatment, she began experiencing recurrent episodes of massive haemoptysis, for which she underwent bronchial artery embolisation twice. Subsequently, the patient started expectorating stones (lithoptysis) as shown in [Table/Fig-1].
Stones of various sizes that were expelled by the patient on coughing.

On examination, the patient was conscious and oriented, with a pulse rate of 128 beats per minute, a respiratory rate of 22 breaths per minute, an oxygen saturation of 96% on room air, and a blood pressure of 110/70 mmHg measured in the sitting position in the right upper arm. Blood investigations revealed microcytic hypochromic anaemia, raised Erythrocyte Sedimentation Rate (ESR), and a reversal of the albumin-globulin ratio, as shown in [Table/Fig-2].
Blood investigations of the patient.
| Parameters | Value | Reference range |
|---|
| Haemoglobin | 9.9 g/dL | 11.6-15 g/dL |
| Albumin | 3.7 g/dL | 3.5-5.5 g/dL |
| Globulin | 4.7 g/dL | 2.0-3.5 g/dL |
| Erythrocyte Sedimentation Rate (ESR) | 118 mm/hr | 0-20 mm/hr |
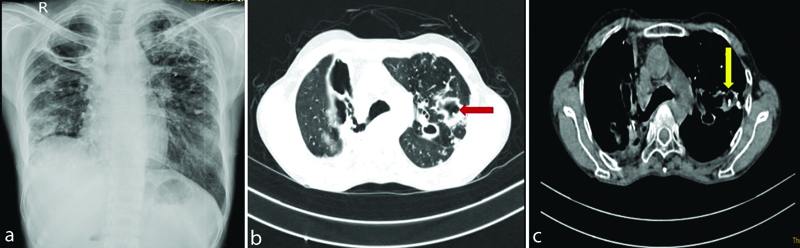
Sputum for Acid-fast Bacilli (AFB) was positive (2+), but TrueNat was negative, thereby excluding Mycobacterium tuberculosis infection. Two sputum cultures were positive for non tuberculous mycobacterium, and the sputum was sent for NTM species identification. A chest X-ray showed bilateral fibrocavitary lesions [Table/Fig-3a], and a Computed Tomography (CT) scan of the thorax revealed cavitary lesions with surrounding consolidation and a calcific focus within the cavity [Table/Fig-3b,c].
a) Chest X-ray showing bilateral fibrocavitary lesion. b) CT scan lung window with a red arrow showing multiple thick walled cavitary lesion with surrounding consolidation scattered throughout bilateral lung fields. c) CT scan mediastinal window with a yellow arrow showing calcified material inside the cavity in the left lung.
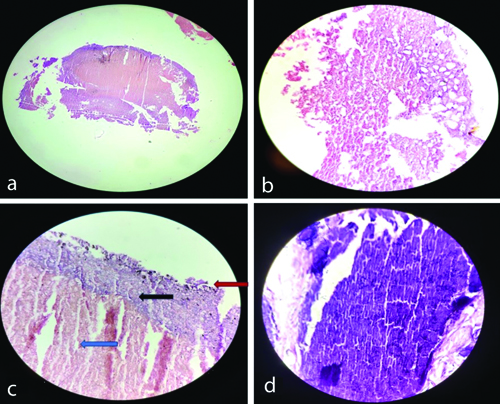
The stones expelled while coughing were sent for histopathological examination {Haematoxylin and Eosin (H&E)}, which confirmed the diagnosis of cavernolith [Table/Fig-4]. Malignancy and reactivation of tuberculosis were the initial differential diagnoses that were ruled out based on the CT scan, which showed no evidence of any mass lesion. The sputum was AFB positive, but TrueNat of the sputum was negative for the patient. The patient had a history of lithoptysis, which can occur in broncholithiasis, cavernolithiasis, and calcified endobronchial tumours. The CT scan revealed calcified material inside the cavity, leading to a diagnosis of NTM infection with cavernolith.
Histopathological image of the cavernolith in (a) Scanner (b) 10x magnification (H&E). Both (a) and (b) showing histopathological features of haemorrhage and necrosis (c) Showing fragments of granulation tissue (red arrow) with few calcified material (black arrow), haemorrhage (blue arrow) and occasionally scattered inflammatory infiltrate (H&E, 40X) (d) Showing areas of calcification (H&E, 40X).
The patient was treated for an NTM infection with Azithromycin 500 mg tablets, weight-based Ethambutol tablets, and Rifampicin tablets, all taken once daily. Since, the patient coughed out the stones, possibly due to the connection of the cavity with the bronchus, no further intervention for Cavernolithiasis was required. The patient was also treated with the proton pump inhibitor Esomeprazole 40 mg twice daily, intravenous fluids, iron supplements in the form of injectable Iron Sucrose once daily for three days, a protein-rich diet, and chest physiotherapy. Liver function tests were monitored to check for possible rifampicin-induced hepatitis. No abnormalities were found in the biochemical parameters after 72 hours of medication consumption. The patient was advised to continue the prescribed regimen for a period of 20 months and to have monthly reviews for sputum AFB examinations. The Matrix Assisted Laser Desorption Ionisation Time of Flight Mass Spectrometry (MALDI-TOF MS) report to identify the Mycobacterium species is awaited. The patient is currently in follow-up, has no symptoms at present, and has started gaining weight.
Discussion
The NTM infection is caused by mycobacteria other than M. tuberculosis and M. leprae. The global prevalence of NTM infection in adults is estimated to be around 10% [1]. The clinical presentation of NTM infection is varied, which poses a challenge in the diagnosis and treatment of the condition. Broncholiths and cavernoliths are calcified materials found within the tracheobronchial tree and lung cavity, respectively [2]. The incidence is about 0.1-0.2%, with a male preponderance [3]. The most common symptoms include chronic cough and haemoptysis. Asymptomatic patients require no intervention, whereas others may need bronchoscopic or surgical removal. Cavernolithiasis in a patient with NTM infection is extremely rare, and no such case has been reported previously to the best of authors knowledge.
Common pulmonary NTM symptoms include chronic cough, fever, fatigue, weight loss, chest pain, and shortness of breath. Underlying lung conditions like bronchiectasis and chronic obstructive pulmonary disease may predispose patients to NTM infection. Fibrocavitary lesions, cylindrical bronchiectasis, and hypersensitivity pneumonitis are the common radiological features observed. Diagnosis involves correlating symptoms with radiological findings and obtaining a positive sputum culture on two different occasions. A single positive culture from bronchoalveolar lavage may also be considered positive. Echeverria G et al., emphasised the importance of sputum culture in their study, where sputum samples from 260 patients were cultured, leading to a conclusion of a 10% prevalence of NTM infection cases that were initially misdiagnosed as tuberculosis [4]. MALDI-TOF MS is very helpful and effective in identifying the organism [5].
Chemotherapy options include amikacin, azithromycin, ethambutol, ethionamide, bedaquiline, doxycycline, isoniazid, levofloxacin, linezolid, and rifampicin. Treatment duration usually varies from 18 to 24 months. A high degree of suspicion should always be maintained for NTM infection in those with chronic and recurring respiratory symptoms.
Gupta et al., presented a report of 18 cases of NTM from a tertiary care centre in India. The cases of NTM infection were speciated, with five identified as M. fortuitum, four as MAC, three as M. abscessus, two as M. kansasii, and one as M. chelonae. Patients were started on various treatment regimens consisting of a mean of 3.8±0.9 drugs. The drugs used most commonly were clarithromycin, amikacin, ethambutol, rifampicin, linezolid, and levofloxacin [6]. Similarly, in present case report, the patient was started on a triple drug regimen consisting of azithromycin, rifampicin, and ethambutol once daily.
Tuberculosis is a major global health issue, but it is a preventable and curable disease. In 2022, an estimated 10.6 million people were affected by tuberculosis worldwide, which was 1.6 times more in men compared to women [7]. Tuberculosis is caused by the bacillus Mycobacterium tuberculosis, which is spread through droplet infection. Pulmonary tuberculosis leads to a number of acute and chronic complications [8], which can be divided by site: a) Lung parenchyma - tuberculoma, residual cavitation, aspergilloma, scarring; b) Airways - obstructive airway disease, broncholithiasis; c) Vascular - Rasmussen pseudoaneurysm, pulmonary thrombosis; d) Pleural - chronic empyema, pneumothorax, bronchopleural fistula.
Broncholith is defined as the presence of a calcified substance in the bronchial tree. Similarly, in cavernolith, a calcific focus is present inside a lung cavity. The most common causes of broncholith and cavernolith are erosion by a calcified lymph node, which is seen in tuberculosis and histoplasma infection [2]. A calcified foreign body, erosion by calcified or ossified cartilage, and migration of a foreign substance into the bronchus from a different site due to fistula formation may lead to cavernolith formation [9]. Cavernoliths usually form inside thoracic tissues previously infected with Mycobacterium tuberculosis. The most common presentation is cough with expectoration, occasionally accompanied by haemoptysis. In a study conducted by He R et al., among 63 patients with broncholithiasis, the most common symptom was cough in 57.1% of patients, followed by haemoptysis, which was observed in 23.8% of patients [10]. There may be a history of expectoration of stones, known as lithoptysis. The patient in present case report presented with cough, expectoration, fever, and lithoptysis. The cavernoliths are usually gray-white, varying in size and shape [11]. They are composed of calcium phosphate or calcium carbonate. Other symptoms include localised wheezing and chest pain. Complications include massive haemoptysis, formation of fistulas, and recurrent pneumonia. Broncholithiasis may result in lobar collapse, bronchiectasis, mucus impaction, and air trapping [12]. Usually, organisms may not be detected in extracted broncholiths.
The diagnosis of cavernolith can be made by observing the change in its position in the cavity with a change in the patient’s position, examined with a series of X-rays. Usually, it occupies a dependent position but sometimes may adhere to the walls [13]. Dakkak M et al., stated that in suspected cases of broncholithiasis, a CT scan is the diagnostic modality of choice [2]. With the help of a CT scan, the exact location of the broncholith can be identified, followed by an attempt at bronchoscopic removal. In the current case, the diagnosis was made through a CT scan, where calcification was seen inside the cavity. Treatment includes the removal of calcified material by bronchoscopy. He R et al., in a study of 63 patients with broncholithiasis, concluded that the first-line therapy was endoscopic removal of the broncholith, followed by surgical removal if necessary [10]. If, the broncholith is inaccessible, lobectomy or segmentectomy may be required. Caution should be taken while removing the broncholith, as close proximity to the pulmonary artery may lead to haemorrhage. Observation is warranted in asymptomatic cases [14].
Conclusion(s)
Cavernolithiasis is a very rare disease that was observed in a patient with a non tuberculous Mycobacterium infection who had previously been diagnosed and treated for pulmonary tuberculosis. Uncomplicated cases may be managed medically with bronchoscopic removal of stones, while patients with complications such as obstructive bronchiectasis, haemoptysis, and bronchopyocele may require surgical resection or lobectomy. A multidisciplinary approach involving a thoracic surgeon, pulmonologist, and radiologist may be beneficial. Despite the potential for complications, the overall prognosis is good when a timely diagnosis is made and appropriate treatment is administered. This is a unique case report of an NTM infection with cavernolithiasis in a patient with a history of pulmonary tuberculosis.
[1]. Zhou Y, Mu W, Zhang J, Wen SW, Pakhale S, Global prevalence of non-tuberculous mycobacteria in adults with non-cystic fibrosis bronchiectasis 2006-2021: A systematic review and meta-analysisBMJ Open 2022 12(8):e05567210.1136/bmjopen-2021-05567235914904PMC9345037 [Google Scholar] [CrossRef] [PubMed]
[2]. Dakkak M, Siddiqi F, Cury JD, Broncholithiasis presenting as bronchiectasis and recurrent pneumoniasBMJ Case Rep 2015 2015:bcr201420903510.1136/bcr-2014-20903526106172PMC4480076 [Google Scholar] [CrossRef] [PubMed]
[3]. Ozyurek BA, Bozbas SS, Broncholithiasis presenting with lithoptysisLung India 2018 35(4):339-340.10.4103/lungindia.lungindia_304_1729970776PMC6034379 [Google Scholar] [CrossRef] [PubMed]
[4]. Echeverria G, Rueda V, Espinoza W, Rosero C, Zumárraga MJ, de Waard JH, First case reports of Nontuberculous Mycobacterial (NTM) lung disease in Ecuador: Important lessons to learnPathogens 2023 12(4):50710.3390/pathogens1204050737111393PMC10142742 [Google Scholar] [CrossRef] [PubMed]
[5]. Bethencourt Mirabal A, Nguyen AD, Ferrer G, Lung Nontuberculous Mycobacterial Infections. [Updated 2024 Feb 17]In: StatPearls [Internet] 2024 Jan Treasure Island (FL)StatPearls PublishingAvailable from: https://www.ncbi.nlm.nih.gov/books/NBK551583/ [Google Scholar]
[6]. Gupta N, Mittal A, Niyas VKM, Banerjee S, Ray Y, Kodan P, Nontuberculous mycobacteria: A report of eighteen cases from a tertiary care center in IndiaLung India 2020 37(6):495-500.10.4103/lungindia.lungindia_365_1933154211PMC7879861 [Google Scholar] [CrossRef] [PubMed]
[7]. Global tuberculosis report 2023 2023 GenevaWorld Health OrganizationAvailable from: https://iris.who.int/bitstream/handle/10665/373828/9789240083851-eng.pdf?sequence=19789240083851-eng.pdf (who.int) [Google Scholar]
[8]. Shah M, Reed C, Complications of tuberculosisCurr Opin Infect Dis 2014 27(5):403-10.10.1097/QCO.000000000000009025028786 [Google Scholar] [CrossRef] [PubMed]
[9]. Weerakkody Y, Silverstone L, Farhadi M, Broncholith. Reference articleRadiopaedia.org (Accessed on 23 Aug 2024). Available from: https://doi.org/10.53347/rID-2403210.53347/rID-24032 [Google Scholar] [CrossRef]
[10]. He R, Zhou H, Jiang M, Lv X, Meng J, Broncholithiasis: Treatment evaluation in 63 patientsAm J Med Sci 2022 363(4):351-58.Epub 2021 Aug 3010.1016/j.amjms.2021.05.02834473998 [Google Scholar] [CrossRef] [PubMed]
[11]. De S, De S, BroncholithiasisLung India 2008 25(4):152-54.10.4103/0970-2113.4528021264082PMC3019338 [Google Scholar] [CrossRef] [PubMed]
[12]. Seo JB, Song KS, Lee JS, Goo JM, Kim HY, Song JW, Broncholithiasis: Review of the causes with radiologic-pathologic correlationRadiographics 2002 22 Spec No:S199-213.10.1148/radiographics.22.suppl_1.g02oc07s19912376611 [Google Scholar] [CrossRef] [PubMed]
[13]. Cooley DA, The clinical significance of cavernolithiasisJournal of Thoracic Surgery10.1016/S0096-5588(20)31019-913035861 [Google Scholar] [CrossRef] [PubMed]
[14]. Krishnan S, Kniese CM, Mankins M, Heitkamp DE, Sheski FD, Kesler KA, Management of broncholithiasisJ Thorac Dis 2018 10(Suppl 28):S3419-S3427.10.21037/jtd.2018.07.1530505529PMC6218369 [Google Scholar] [CrossRef] [PubMed]