Glaucoma encompasses a group of diseases characterised by irreversible and progressive damage to the neuroretinal fibres, with characteristic structural damage to the optic nerve and corresponding visual dysfunction caused by various pathological processes [1]. It is the second most common cause of blindness after cataracts and is globally the leading cause of irreversible blindness [2]. The prevalence of glaucoma among individuals aged 40-80 years is 3.54% [3]. India has an estimated 12 million cases of glaucoma and accounts for approximately one-fifth of the global glaucoma burden. POAG is a more common variant compared to Primary Angle-closure Glaucoma (PACG), accounting for approximately three-fourths of all glaucoma cases [2]. India contributes to 12.9% of global POAG blindness and 12.7% of PACG blindness [3].
A common characteristic of glaucoma is optic neuropathy, which results from various risk factors such as older age, hypertension, diabetes, high myopia, trauma, steroid overuse, lower ocular perfusion pressure and increased IOP [2]. IOP and the aqueous humour dynamics that regulate the pressure are factors that can be controlled to prevent the progression of optic neuropathy [4]. Trabeculectomy, introduced in 1968 by Watson and Cairns, is the standard surgical intervention for managing glaucoma, with a success rate between 67% and 94% in primary glaucoma cases [5]. A fistula is created to connect the Anterior Chamber (AC) with the subtenon space, permitting a bypass from the trabecular meshwork by the aqueous humour [6]. Several postoperative complications, such as early postoperative aqueous leak (21%), postoperative hyphema (18%-38%), initiation or progression of cataract formation (10%-20%) and failing bleb due to conjunctival or episcleral fibrosis, are observed with this procedure [7].
To overcome these complications, a novel technique of creating a fistula into the subconjunctival space with minimal disruption of conjunctiva and ocular tissues, which does not induce significant astigmatism, has been described. This technique is known as small flap trabeculectomy or microtrabeculectomy [8].
Many previous studies have attempted to compare the safety and efficacy of microtrabeculectomy with CT in POAG patients, but no study has reached a clear conclusion. Additionally, not many studies have been conducted in the Indian context [9,10]. Thus, the current study aimed to compare the efficacy of microtrabeculectomy with CT in treating POAG.
Materials and Methods
A prospective interventional study was performed in the Department of Ophthalmology at Shri BM Patil Medical College Hospital and Research Centre (tertiary care centre), BLDE (DU), Vijayapura, North Karnataka, India, from June 2023 to August 2024. The research was conducted in accordance with the Declaration of Helsinki and institutional ethical clearance was obtained (Ethical clearance approval number: BLDE (DU)/IEC/684/2022-23). After explaining the nature of the procedure and the associated risks and benefits to the patients, informed consent was obtained. The study focused on patients diagnosed with POAG who required filtration surgery.
Inclusion criteria: Patients diagnosed with POAG, who had raised IOP values and were willing to undergo filtration surgery, were enrolled in the present study.
Exclusion criteria: Patients with PACG, secondary and congenital glaucoma, a history of previous intraocular surgery in the same eye, rubeotic eye, uveitis and those unwilling to participate in the study were excluded.
Sample size: A total of 16 patients were included based on convenience sampling.
Study Procedure
The patients were divided into two groups of eight each: Group-I underwent microtrabeculectomy and Group-II underwent CT. Demographic characteristics, preoperative IOP readings, Cup-to-Disc (C:D) ratio, angle grading and visual fields of the participants were obtained and tabulated.
Surgical procedure: The surgery was performed by a single surgeon under local peribulbar anaesthesia. After painting and draping, a wire speculum was placed and a superior rectus bridle suture was secured.
Group-I: Small flap trabeculectomy (microtrabeculectomy)
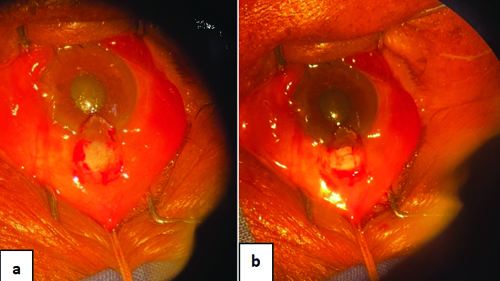
After the conjunctival flap was fashioned, a square-shaped lamellar scleral flap measuring 2×2 mm (1/2 to 1/3 of the thickness of the sclera) was created with the limbus as the base and dissected up to the level where the bluish-grey zone is at least 1 mm exposed. AC entry was made at the anterior end using Vannas scissors. A Kelly Descemet membrane punch was used to remove 1×1 mm of the trabecular meshwork. The scleral flap was approximated using a single 10-0 monofilament suture after performing the peripheral iridectomy. The conjunctival flap was then approximated using continuous 10-0 monofilament sutures [Table/Fig-1a,b].
a) Conjunctival flap is fashioned; b) 2×2 mm square shaped lamellar scleral flap.
Group-II: Conventional Trabeculectomy (CT) [9]
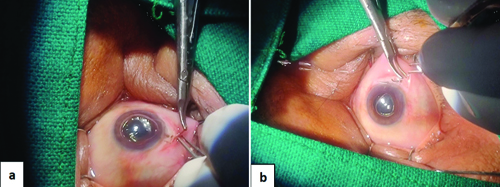
A conjunctival flap was created, after which a partial thickness, limbal-based, lamellar, square-shaped scleral flap measuring 5×5 mm (1/2 to 1/3 of the thickness of the sclera) was performed. The flap was extended well past the limbus into the clear cornea until the bluish-grey zone was exposed up to 1 mm. Adjacent to the scleral spur anteriorly a block of tissue measuring 1×4 mm was excised manually. The scleral flap was approximated to the scleral bed using 10-0 monofilament sutures after a broad-based peripheral iridectomy was performed. The conjunctival flap was then approximated with a continuous 10-0 monofilament suture [Table/Fig-2a,b].
Scleral and conjunctival flap suturing in Conventional Trabeculectomy (CT).
Postoperative course: Antibiotic-steroid eye drops were administered six times daily to all patients and gradually tapered over six weeks. Patients were evaluated on the first postoperative day and followed-up at one week, six weeks and three-month intervals. On the first postoperative day, patients were examined for conjunctival inflammation, bleb characteristics, corneal oedema, formation of the AC and hyphema. In subsequent follow-ups, IOP recording was performed using Goldmann’s applanation tonometer.
Success criteria: Success was achieved when the postoperative IOP was in the range of 6 to 21 mmHg according to the World Glaucoma Association (WGA) [11].
Complete success: IOP less than or equal to 21 mmHg without any topical antiglaucoma agents [11].
Qualified success: IOP less than or equal to 21 mmHg with the requirement of antiglaucoma medications to achieve the target [11].
Failure: IOP greater than 21 mmHg or less than 5 mmHg with medications based on two consecutive follow-up visits, at least one week apart [11].
Statistical Analysis
Data was documented in Microsoft Excel and analysed using statistical software R 3.6.3. Continuous variables and categorical variables were represented by mean±Standard Deviation (SD) and frequency tables, respectively. The Chi-square test or independent samples t-test was employed to check for associations. A p-value ≤0.05 was considered statistically significant.
Results
The study was conducted on 16 patients aged 40 to 80 years with POAG. The patients were divided into two groups: Group-I, which underwent microtrabeculectomy and Group-II, which underwent CT, with eight patients in each group. The demographic details and baseline characteristics of the patients in both groups is illustrated in [Table/Fig-3].
Demographic details and baseline characteristics of the patients and in the groups.
| Characteristics | Mean±SD | Median (Range) |
|---|
| Age (in years) | 61.18±9.33 | 65 (53.75, 68.25) |
| C:D ratio | 0.8±0.08 | 0.8 (0.7, 0.9) |
| Preop IOP (mmHg) | 30.37±6.46 | 28 (25.75, 33.5) |
The ages of the patients included in this study ranged from 53.75 to 68.25 years, with a mean of 61.18±9.33 years. Two patients in Group-I were on previous antiglaucoma medication, while one patient in Group-II was also on previous antiglaucoma medication. In total, 13 patients (6 in Group-I and 7 in Group-II) were newly diagnosed. The Best Corrected Visual Acuity (BCVA) of one patient in Group-I and two patients in Group-II was ≤6/60 on the Snellen chart. All the remaining patients in both groups had a BCVA of >6/60 (7 in Group-I and 6 in Group-II). In Group-I, 4 cases (50%) had a C:D of 0.7; in Group-II, 1 case (12.5%) had a C:D ratio of 0.7. A C:D ratio of 0.8 was observed in 1 (12.5%) case in Group-I and in 5 (62.5%) cases in Group-II. A C:D ratio of 0.9 was seen in 3 (37.5%) cases in Group-I and in 2 (25%) cases in Group-II. The vertical C:D ratio was higher compared to the horizontal C:D ratio [Table/Fig-4].
Comparison of demographic details and baseline characteristics of the patients between the groups.
| Variables | Groups | Total | p-value |
|---|
| Group-I | Group-II |
|---|
| Age (in years) | 62.62±7.3 | 59.75±11.34 | | 0.55 |
| Gender | Male | 6 (75%) | 5 (62.4%) | 11 | 0.99MC |
| Female | 2 (25%) | 3 (37.5%) | 5 |
| Eye involved | Right | 4 (50%) | 6 (75%) | 10 | 0.99MC |
| Left | 4 (50%) | 2 (25%) | 6 |
| Angle grading | 3 | 6 (75%) | 7 (87.5%) | 13 | 0.99MC |
| 4 | 2 (25%) | 1 (12.5%) | 3 |
| Visual fields | 2 | 3 (37.5%) | 3 (37.5%) | 6 | 0.99MC |
| 3 | 5 (62.5%) | 4 (50%) | 9 |
| NR | 0 (0) | 1 (12.5%) | 1 |
| C:D ratio | 0.7 | 4 (50%) | 1 (12.5%) | 5 | 0.99MC |
| 0.8 | 1 (12.5%) | 5 (62.5%) | 6 |
| 0.9 | 3 (37.5%) | 2 (25%) | 5 |
| BCVA | <6/60 | 1 (12.5%) | 2 (25%) | 3 | 0.99MC |
| >6/60 | 7 (87.5%) | 6 (75%) | 13 |
| Previous treatment history | Previous antiglaucoma medications | 2 (25%) | 1 (12.5%) | 3 | 0.99MC |
| Newlydiagnosed | 6 (75%) | 7 (87.5%) | 13 |
*IOP: Intraocular pressure; CT: Conventional trabeculectomy; MT: Microtrabeculectomy; POAG: Primary open angle glaucoma; NR: Non recordable; MC: McNemar’s test
The comparison of IOP within the groups is illustrated in [Table/Fig-5]. The IOP within the CT group was significantly different between preoperative and postoperative follow-ups (p<0.00001). Similarly, the IOP within the Microtrabeculectomy (MT) group significantly decreased from preoperative IOP to postoperative follow-ups (p<0.00001). However, no significant difference in IOP was observed between the groups at both preoperative and postoperative follow-ups (p>0.05) [Table/Fig-6].
Preoperative and postoperative IOP within-group analysis over time.
| Variables | Time points | Groups |
|---|
| Conventional Trabeculectomy (CT) | Microtrabeculectomy |
|---|
| Median (Range) | Mean (SD) | Median (Range) | Mean (SD) |
|---|
| IOP (in mmHg) | Preoperative | 27.5 (25.5, 31.25) | 30 (7.27) | 30.5 (25.75, 33.5) | 30.75 (6.04) |
| Postoperative week 1 | 12 (9.75, 14.5) | 12.25 (3.05) | 13 (10, 15) | 12.62 (2.72) |
| Postoperative week 6 | 13.5 (10.75, 16) | 13.5 (3.02) | 14 (10.75, 15.25) | 13.5 (2.97) |
| Postoperative month 3 | 14 (12, 16.25) | 14.12 (2.79) | 14 (11.75, 16) | 13.97 (2.79) |
| p-value | <0.00001* | - | <0.00001* | - |
*IOP: Intraocular pressure; CT: Conventional trabeculectomy; MT: Microtrabeculectomy; *p-value statistically significant
Comparison of IOP at different timepoints between the groups.
| Different time points | Groups | p-value |
|---|
| Conventional Trabeculectomy (CT) | Microtrabeculectomy |
|---|
| Median (range) | Mean (SD) | Median (Range) | Mean (SD) |
|---|
| Preoperative IOP (in mmHg) | 27.5 (25.5, 31.25) | 30 (7.27) | 30.5 (25.75, 33.5) | 30.75 (6.04) | 0.63MU |
| Postoperative week 1 (in mmHg) | 12 (9.75, 14.5) | 12.25 (3.05) | 13 (13, 15) | 12.62 (2.72) | 0.78MU |
| Postoperative week 6 (in mmHg) | 13.5 (10.75, 16) | 13.5 (3.02) | 14 (10.75, 15.25) | 13.5 (2.97) | 0.99MU |
| Postoperative month 3 (in mmHg) | 14 (12, 16.25) | 14.25 (2.79) | 14 (11.75, 16) | 13.87 (2.79) | 0.87MU |
*MU: Mann-Whitney U test; IOP: Intraocular pressure; CT: Conventional trabeculectomy; MT: Microtrabeculectomy
None of the patients met the criteria for failure. All the patients fulfilled the criteria for complete success (16 patients, 100%).
In Group-I, one patient experienced intraoperative subconjunctival bleeding and early postoperative hyphema. In Group-II, two patients had intraoperative subconjunctival bleeding and early postoperative hyphema.
Discussion
Trabeculectomy is accepted worldwide as the safest and most effective drainage procedure for glaucoma. Although medical treatment is effective, the cost, adherence to medical therapy and associated side-effects are problematic in developing countries. Therefore, an effective surgical procedure is needed that can slow down the mechanism of damage in the nerve fibre layer and the corresponding visual field dysfunction, while minimising complications. The present study aimed to compare the efficacy and safety profiles of microtrabeculectomy and CT in cases diagnosed with POAG.
Most patients in the present study were between 61-70 years of age (mean age 61.18±9.33 years), indicating that age can be a factor contributing to the development of POAG. This aligns with a study conducted by Mudhol R and Bansal R in a similar demographic, which reported a mean age of 67.63±8.86 years [12]. The same finding was consistent with the studies by Kumar A and Gupta D (mean age 60.72±9.62 years) [13].
Out of the 16 patients in the current study, 5 (31.25%) were females and 11 (68.75%) were males, exhibiting a robust male predilection. Evidence suggests that female sex hormones might be protective of the optic nerve, explaining the male preference [14]. However, although females exhibit a marked propensity for PACG, the sex predilection in POAG remains controversial, with the Rotterdam study showing a male predilection and the Blue Mountains Eye study showing a female predilection [15,16].
The present study showed that most patients had an increase in the vertical C:D ratio (mean ratio 0.8±0.08) compared to the horizontal ratio. A higher value in the former is a risk factor for the progression of glaucomatous visual dysfunction [17]. This was mirrored by a study conducted by Kurysheva NI and Lepeshkina LV which stated that an increase in the C:D ratio by more than or equal to 0.2 is a risk factor for glaucoma [18].
Out of 16 patients, three experienced subconjunctival bleeding during the intraoperative period. Two of these three patients were on long-term antiglaucoma medications. Episcleral bleeding is commonly observed in patients who have been on antiglaucoma medications for an extended period [19]. Hyphema was also noted in these patients, which resolved spontaneously. No late complications were reported in either group during follow-up.
Controlling IOP is the only intervention that can delay the onset and slow the progression of glaucoma, making it a crucial parameter to measure. The present study demonstrated a substantial difference in preoperative and postoperative IOP for both groups, with Group-I exhibiting a mean percentage reduction of 53% at the end of the third postoperative month and Group-II showing a decrease of 52.2%. This difference was statistically significant for both groups (p<0.001). Rong SS et al., proposed a cut-off value of 13.5 mm Hg on the seventh day for predicting an 80.0% success rate in achieving an IOP of less than 15 mm Hg without medications at 18 months [20]. This finding was comparable to the study by Mudhol RR and Ray A, in which they performed a subtenon injection of low-dose mitomycin C and achieved an initial success rate of 53.55% [21]. This cut-off value was achieved by all cases in the present study.
The difference in postoperative IOP values at follow-ups and the difference in IOPs from the preoperative value between the groups were not statistically significant (p>0.05), indicating similar efficacy of both procedures. This suggests that microtrabeculectomy is equally effective as CT for treating POAG. Microtrabeculectomy has certain advantages over CT. Since it occupies a smaller surface area of the eye, there is enough space for a minimum of three micro trabeculectomies near the superior limbus in case of failure [13]. This is a beneficial characteristic when operating on patients who have previously undergone cataract surgery. Additionally, the smaller size of the surgical field decreases the risk of corneal astigmatism compared to the conventional method, leading to faster visual rehabilitation. Furthermore, microtrabeculectomy results in a shorter hospital stay and recovery [13].
Limitation(s)
The present study had limitations, including a smaller sample size, being a single-centre study and a shorter follow-up period. A large-scale study with an extended follow-up period will further strengthen the findings of the present research.
Conclusion(s)
Thus, microtrabeculectomy is a safe procedure that has similar efficacy to CT for reducing IOP while producing good filtering blebs with fewer complications.
*IOP: Intraocular pressure; CT: Conventional trabeculectomy; MT: Microtrabeculectomy; POAG: Primary open angle glaucoma; NR: Non recordable; MC: McNemar’s test
*IOP: Intraocular pressure; CT: Conventional trabeculectomy; MT: Microtrabeculectomy; *p-value statistically significant
*MU: Mann-Whitney U test; IOP: Intraocular pressure; CT: Conventional trabeculectomy; MT: Microtrabeculectomy