The knee is the most commonly injured joint in the body. The ACL is a ligament located in the middle of the knee and injuries to this ligament are common and referred to as ACL injuries [1]. The primary function of the ACL is to provide anteroposterior and rotational stability, while its secondary function includes acting as a proprioceptor for the joint, offering mediolateral stability and resisting valgus and varus stress [2]. Athletes and sports persons are more prone to ACL injuries [3]. Such serious injuries can significantly impede the careers of athletes and sports professionals. An ACL injury may result from a hyperextended knee and if there is a muscle tear, it can lead to a more severe injury [4-6]. Studies indicate that 50% of ACL injuries involve a combination of damage to the meniscus, articular cartilage and other ligaments [7-9]. Furthermore, research shows that female athletes have a greater likelihood of knee injuries compared to their male counterparts, attributed to differences in physical conditioning, muscular strength and other factors [10,11].
Arthroscopic ACL reconstruction has become the gold standard for treating torn ACLs. This procedure allows patients to return to their preinjury activity levels while delaying meniscal degenerative injuries and the onset of osteoarthritis. Despite these established benefits, ongoing research is focused on optimising ACL reconstruction techniques, particularly about using various grafts and the anatomical reconstruction of both the anteromedial and posterolateral bundles to improve rotational stability. Accurate placement of the femoral tunnel has also been shown to play a crucial role in determining the success of the procedure [11]. While ACL reconstruction using a four-strand hamstring tendon autograft has demonstrated benefits such as the elimination of anterior tibial subluxation, improved functional knee scores and enhanced isokinetic knee extension strength, there remains a need for further investigation.
The novelty of present study lies in evaluating the functional outcomes of this specific technique in a cohort of patients and its impact on postoperative recovery. By focusing on the functional outcomes of arthroscopic management using a four-strand hamstring tendon graft, present study aimed to provide additional evidence to refine surgical techniques and improve patient outcomes.
Materials and Methods
This prospective cohort study was conducted at the Department of Orthopaedics, SRM Medical College and Hospital and Research Centre, Chennai, Tamil Nadu, India, from January 2016 to June 2017, including the follow-up period. A total of 33 participants who met the study’s inclusion criteria and were treated during the study period were selected. Ethical approval was obtained from the SRM Institutional Ethics Committee (Ethics clearance number: 903/IEC/2015), and the study’s progress was periodically reviewed.
Inclusion criteria: Patients with unilateral Grade II and Grade III ACL tears, aged between 20 and 55 years, with or without associated meniscal injuries, who had experienced traumatic knee injuries, were included in the study.
Exclusion criteria: Individuals having multiligament injuries, skeletal immaturity, lower limb bony injuries, prior knee surgeries, or any medical conditions contraindicating an anaesthesia were excluded from the study.
The surgical procedure involved ACL reconstruction using a four-strand hamstring tendon graft, where the femoral tunnel was created through the transtibial technique, and the tibial tunnel was made using the “Tibial Zig” technique. Patients were monitored for a minimum period of six months, with regular follow-ups.
Clinical evaluations were conducted at baseline (preoperatively) and at various postoperative intervals. Two key clinical parameters were assessed during the follow-up: the Tegner Lysholm score [12] and the VAS. The Tegner Lysholm score was utilised to measure knee function, addressing common complaints such as limping, pain, swelling, locking and instability, both before surgery and at three and six months postoperatively. The VAS was employed to assess pain levels, with patients rating their pain on a scale of 0 (no pain) to 10 (unbearable pain) at different time points: preoperatively, on the second postoperative day, at the second week, the third month and the sixth month.
Statistical Analysis
Statistical analysis was performed using SPSS version 16.0. The collected data were analysed using various statistical tools, including mean±Standard Deviation (SD), frequency and percentage distributions, and ANOVA tests to assess changes in clinical outcomes over time.
Results
The age distribution showed that the majority of patients i.e., 18 (54.55%), were between 21 and 30 years of age. Most of the participants were male, accounting for 29 (87.88%), with only 12.12% being female [Table/Fig-1]. The involvement of the right knee was slightly higher compared to the left knee [Table/Fig-2].
| Parameters | n (%) |
|---|
| Age (years) |
| ≤20 | 1 (3.03) |
| 21-30 | 18 (54.55) |
| 31-40 | 9 (27.27) |
| 41-50 | 5 (15.15) |
| Gender |
| Male | 29 (87.88) |
| Female | 4 (12.12) |
| Knee- side involved | n (%) |
|---|
| Right-side | 17 (51.52) |
| Left-side | 16 (48.48) |
Regarding diagnosis, 21 (63.64%) of the patients had isolated ACL tears. The distribution of diagnosis showed no significant variation (p-value=0.2251) [Table/Fig-3].
| Diagnosis | n (%) |
|---|
| ACL tear | 21 (63.64) |
| ACL tear with medial meniscal tear | 10 (30.30) |
| ACL tear with lateral meniscal tear | 1 (3.03) |
| ACL tear with medial and lateral meniscal tear | 1 (3.03) |
Preoperative and postoperative outcomes were assessed using the Tegner Lysholm Knee Score. The mean preoperative score was 35.97, which significantly improved to 71.97 at three months and 88.85 at six months postoperatively, with highly significant p-values (<0.0001) across all time comparisons, indicating a strong improvement in knee function postsurgery [Table/Fig-4].
Mean preoperative and postoperative Tegner-Lysholm Knee Scores.
| The Tegner Lysholm Knee Score | Preoperative | Postoperative (3 months) | Postoperative (6 months) |
|---|
| Mean±SD | 35.97±19.01 | 71.97±8.27 | 88.85±5.56 |
| p-value | Preoperative vs postoperative (3 months) | <0.0001 |
| Preoperative vs postoperative (6 months) | <0.0001 |
| Postoperative (3 months) Vs Postoperative (6 months) | <0.0001 |
| p-value ANOVA - | <0.0001 |
| Two factor without replication |
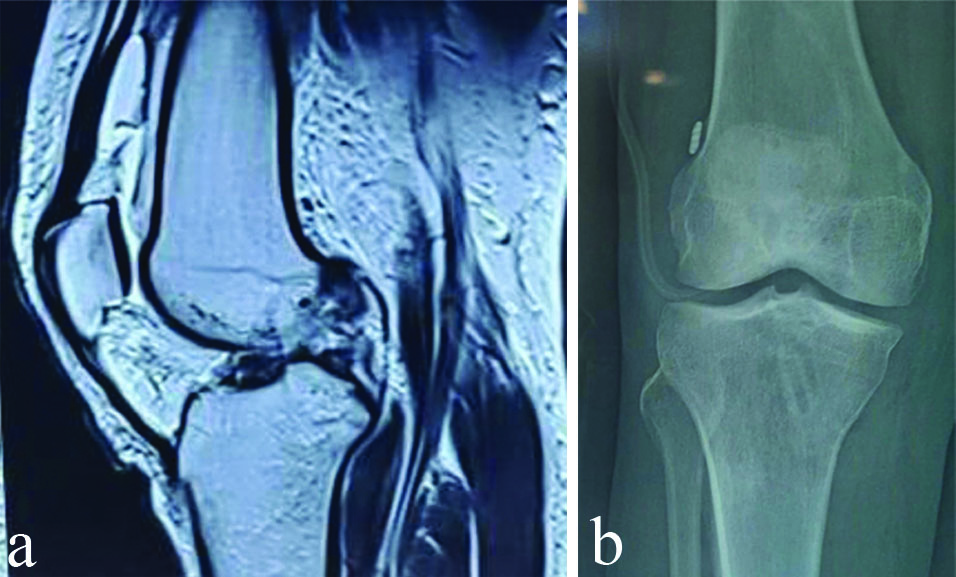
VAS scores were highest on the second postoperative day and steadily declined by the six-month follow-up, with significant improvements demonstrated by ANOVA (p-value<0.0001). Notably, patients undergoing arthroscopic ACL reconstruction with both medial and lateral meniscectomies had the highest preoperative VAS score (6.00), though pain levels reduced substantially over time [Table/Fig-5]. An MRI image showing pre- and postoperative reconstruction of the ACL tear is presented in [Table/Fig-6].
Visual Analogue Scale (VAS) scores.
| Visual analog scale score- procedures | Preoperative | Postoperative (2nd day) | Postoperative (2nd week) | Postoperative (3 months) | Postoperative (6 months) | p-value ANOVA-two factor without replication |
|---|
| Arthroscopic ACL reconstruction | 2.38 | 6.48 | 3.86 | 0.62 | 0.24 | <0.0001 |
| Arthroscopic ACL reconstruction with medial menisectomy | 3.5 | 6.8 | 3.9 | 1 | 0.4 | <0.0001 |
| Arthroscopic ACL reconstruction with lateral menisectomy | 0.00 | 5.00 | 2.00 | 0.00 | 0.00 | <0.0001 |
| Arthroscopic ACL reconstruction with medial and lateral menisectomy | 6.00 | 8.00 | 3.00 | 2.00 | 1.00 | <0.0001 |
a) MRI shows an ACL tear and b) Postoperative X-ray shows the EndoButton position and tibial tunnel for the screw.
Discussion
The current work examines the functional success of arthroscopic therapy for ACL restoration using a four-strand hamstring tendon graft. An investigation conducted by Jameson S, Emmerson K, revealed that single-bundle ACL restoration is the most effective approach [13]. However, Suomalainen P et al., also discovered that the double-bundle reconstruction methodology ultimately reduces the rate of degenerative changes [14]. A critical analysis of the rate of subsequent surgery and its predictors after undergoing ACL reconstruction found that 0.49% of the patients, approximately six individuals with an average follow-up treatment of two and a half months, experienced deep infections after the surgery [15]. In contrast, present study did not report any postoperative infections, suggesting a successful outcome of the medical procedure.
A comparative study was conducted to assess the functional outcome of preserving remaining tissue in arthroscopic ACL restoration using a quadrupled hamstring graft. A comprehensive empirical examination of 16 patients revealed a significant difference in functional outcomes and proprioception. Accordingly, it was discovered that the preservation of the remaining tibia positively correlates with proprioceptive function [16].
Present study revealed highly significant knee scores, which align with the findings of the study by Williams RJ et al., which also reported notably higher functional knee scores [17]. A recent study conducted by Yahia A, also showed notable improvements in functional knee ratings throughout follow-up, which aligns with the findings of present study investigation [16].
In a study conducted by Jagdeesh PC and Shaikh SR patients with ACL injuries who underwent arthroscopic anatomical ACL reconstruction using a quadrupled hamstring autograft were evaluated using the International Knee Documentation Committee score (IKDC), Lysholm scoring systems, the Tegner activity scale, and a subjective questionnaire. About 95% of the patients had favourable outcomes (IKDC, Lysholm score, subjective questionnaire) across all three scoring systems [18]. However, long-term follow-up is needed to determine the additional benefits of ACL reconstruction with four-strand hamstring tendon grafts, like delaying degeneration, improving sports activity and lesser chondral injuries. Comparative studies are needed to know the advantages of hamstring tendon grafts over other types of reconstruction.
Limitation(s)
The limitations of this study include a small sample size of 33 patients, which restricts the generalisability of the findings. Additionally, the short follow-up duration of six months is insufficient to assess long-term outcomes such as knee degeneration, osteoarthritis, or the rate of reinjury. As a single-centre study, the results may not reflect broader populations or variations in clinical practice across different healthcare settings. The absence of a comparison group between different ACL reconstruction techniques or graft options, such as patellar tendon grafts, further limits the ability to evaluate the specific advantages of the four-strand hamstring tendon graft. Furthermore, some assessments, like the VAS for pain, rely on subjective patient-reported data, which may introduce potential bias.
Conclusion(s)
Patients who underwent ACL reconstruction with an autologous four-strand hamstring tendon graft demonstrated good functional outcomes and clinical stability, with no significant complications. Future longitudinal and comparative studies are essential to ascertain the procedure’s impact on knee degeneration over time.