Introduction
Gestational Diabetes Mellitus (GDM) is a prevalent pregnancy complication with significant health implications for both the mother and offspring. Galectin-3, a protein expressed in various cells, contributes to cellular and systemic insulin resistance and is secreted into extracellular fluid. However, the link between Galectin-3 and insulin resistance in the development of GDM has not been firmly established.
Aim
To estimate the circulating Galectin-3 levels in diagnosed GDM patients and compare them with those of healthy pregnant women.
Materials and Methods
This cross-sectional study was conducted in the Obstetrics and Gynaecology Outpatient Department (OPD) at SRM Medical College Hospital and Research Centre, SRM Institute of Science and Technology, Kattankulathur, Chengalpattu, Tamil Nadu, India, from July 2023 to December 2023, including 40 pregnant women aged ≥18 years in each group. The parameters measured between both groups included the diabetic profile, lipid profile and Galectin-3 levels. The case group consisted of individuals diagnosed with GDM whose Oral Glucose Challenge Test (OGCT) value was ≥140 mg/dL, whereas the control group comprised pregnant women with OGCT values below 140 mg/dL {selected using Diabetes in Pregnancy Study Group of India (DIPSI) criteria}. Independent t-tests, Mann-Whitney U tests and Pearson Correlation were performed using Statistical Package for the Social Sciences (SPSS) (27.0).
Results
The mean age of the patients was 27.78±3.84 years in the GDM group and 26.88±3.89 years in the normal pregnancy group. The mean Galectin-3 levels were higher in GDM patients compared to normal pregnant women (4.84±0.75 ng/mL vs. 3.34±0.78 ng/mL; p<0.001). Additionally, GDM patients exhibited significant increases in Fasting Plasma Glucose (FPG), fasting insulin, Homeostatic Model Assessment for Insulin Resistance (HOMA-IR), Triglycerides (TyG) index and Glycated Haemoglobin (HbA1c) compared to normal pregnant women.
Conclusion
The present study confirmed the presence of insulin resistance and elevated Galectin-3 levels in pregnancies affected by GDM but did not find a correlation between them.
Introduction
The GDM is a prevalent metabolic condition that develops during pregnancy. It is a temporary type of diabetes that arises due to insulin resistance and the malfunction of pancreatic β-cells during pregnancy. GDM causes an increased propensity for adverse pregnancy effects for both the mother and the offspring [1-4]. The effects can be both short-term as well as long-term [5]. Women diagnosed with GDM are prone to experiencing health issues throughout the postnatal period. In addition, they are more likely to develop diabetes and cardiovascular disease in the future. Many factors contribute to the risk of GDM [6,7]. These factors may include maternal characteristics such as advanced maternal age, pre-pregnancy overweight or obesity, excessive gestational weight gain, dietary patterns, passive smoking, parity, family history of diabetes and socioeconomic status [8]. The prevalence of GDM varies depending on population characteristics and diagnostic criteria. A cohort study conducted in the UK and Ireland in 2010 indicated that 1-3% of pregnancies are affected by GDM. In the early 1980s, the prevalence of GDM was 2% in India [9]. However, a 2008 study revealed higher rates, with urban areas experiencing a prevalence of 17.8%, rural areas 9.9% and semi-urban regions 13.8% [10]. There is considerable geographical variation in GDM prevalence in India, ranging from 3.2% in Kashmir [11] to 16.2% in Tamil Nadu [10,12]. Galectin-3 is a protein found in various types of cells and can be released into the extracellular fluid in its soluble form [13]. It serves various functions, including regulating cell adhesion, differentiation, proliferation and promoting inflammation [14-16]. In women with a history of GDM, insulin resistance is present before pregnancy and progresses during gestation [17,18]. Hyperglycaemia occurs when an increase in insulin secretion is unable to compensate for insulin resistance [19]. Because Galectin-3 has been associated with insulin resistance, there is a possibility that circulating Galectin-3 mediates insulin resistance, which might be a factor in the pathogenesis of GDM [20]. Literature focusing on Galectin-3 levels in Indian women with GDM is scarce. An Israeli study comparing Galectin-3 levels between normal healthy pregnant women and GDM participants identified significantly elevated levels in women with GDM [21]. A recent study found that Galectin-3 was significantly related to adverse pregnancy outcomes in Chinese mothers with GDM [22]. In the present study, an attempt was made to estimate circulating Galectin-3 levels in pregnant women with GDM and in normal healthy pregnant women and to investigate whether circulating Galectin-3 is associated with insulin resistance in GDM within the Indian context.
Materials and Methods
A cross-sectional study was carried out at OPD SRM Medical College Hospital and Research Centre, SRM Institute of Science and Technology, located in Kattankulathur, Chennai, Tamil Nadu, India, from July 2023 to December 2023. Following the study protocol, the authors obtained written informed consent from each participant after receiving approval from the Institutional Ethics Committee (SRMIEC-ST0323-437). The present study comprised 80 gestational age-matched pregnant women, of whom 40 had GDM and 40 were normal, healthy pregnant women.
Inclusion criteria:
For GDM patients: Pregnant women aged 18 years and older with singleton gestation diagnosed with GDM using the Diabetes in Pregnancy Study Group India (DIPSI) criteria [23], with a gestational age between 24 and 36 weeks, were included in the case group.
For normal pregnancy: Pregnant women aged 18 years and older with singleton gestation and a gestational age between 24 and 36 weeks were included in the control group.
Exclusion criteria: Pregnant women with a history of Diabetes Mellitus (DM), polyhydramnios, Polycystic Ovary Syndrome (PCOS), chronic hypertension, chronic renal disease, coronary heart disease, heart failure, infectious diseases and liver disease were excluded from both the case and control groups.
Sample size calculation: The sample size was calculated using the formula:
N={(zα/2+z1-β)2(σ12+σ22)}/(μ1-μ2)2 where [21],
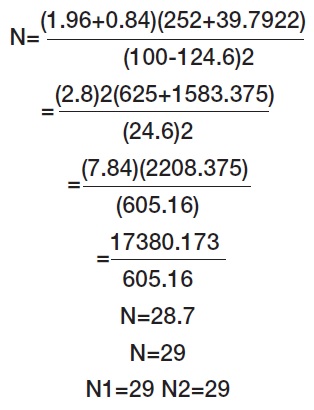
N: Sample size required for the case and control groups in the gestational age of 24 to 36 weeks. z(α/2): z-score corresponding to the desired significance level (α) for a two-tailed test. z(1-β): z-score corresponding to the desired power (1-β) for the test. σ12 and σ22: variances of the two populations. μ1 and μ2: means of the two populations.
μ1=100, standard deviation σ1=25% of 100; σ1=0.25×100=25
μ2=124.6, standard deviation σ2=32% of 124.6; σ2=0.32×124.6=39.792.
Using this formula, the minimum sample size required was N1=29 and N2=29. However, in the current study, the sample size was 80, with N1=40 and N2=40, where N1 and N2 are the sample sizes required for GDM patients and normal pregnancy groups, respectively.
Study Procedure
The GDM was diagnosed using the DIPSI criteria [23] for gestational ages between 24 and 36 weeks. Pregnant women attending the antenatal Outpatient Department (OPD) were given 75 g of anhydrous glucose dissolved in 250-300 mL of water, regardless of their fasting state and plasma glucose levels were estimated after two hours. A two-hour plasma glucose level of ≥140 mg/dL was considered a criterion for diagnosing GDM. Biochemical parameters like FPG, fasting insulin, HbA1c, HOMA-IR, HOMA-β, TyG index and Galectin-3 were measured. HOMA-IR was calculated using the formula: HOMA-IR=(fasting insulin (μIU/mL)×fasting blood glucose (mg/dL))/405 [24]. The TyG index was calculated using the formula: TyG index=Ln (TyG (mg/dL)×FPG (mg/dL))/2 [25]. The Homeostatic Model Assessment for β cell function (HOMA-β) was calculated using the formula: HOMA-β={20×fasting insulin (μU/L)}/{(FPG (mg/dL)×0.0555)-3.5} [24]. Following aseptic protocol, a 4 mL fasting venous blood sample was collected in plain vacutainer, sodium fluoride and Ethylenediamine Tetraacetic Acid (EDTA) tubes. (The plain vacutainer tubes were centrifuged at 3000 rpm for 10 minutes and the serum sample was separated). Samples were analysed for various parameters, like glucose and HbA1c. The remaining samples were aliquoted and stored daily at -80°C until the analysis of Galectin-3 and fasting insulin. The samples can be stored at -80°C for one year and the validity of the kits is also one year. Galectin-3 and fasting insulin were estimated using a Bio-Rad Enzyme-linked Immunosorbent Assay (ELISA) reader and washer, while HbA1c was analysed using a Bio-Rad D10.
Statistical Analysis
The statistical analysis was performed utilising SPSS version 27.0 software. Data are expressed as mean±SD for parametric variables and as median (interquartile ranges) for non parametric variables. An independent samples t-test was used to determine the significant difference between the means of two independent groups: pregnant women with GDM and normal healthy pregnant women. The Mann-Whitney U test was used to compare the medians between the groups. The Pearson correlation coefficient was used to analyse the correlation between serum Galectin-3 levels and insulin resistance in GDM patients.
Results
The Body Mass Index (BMI) was higher in GDM patients compared to normal, healthy pregnant women. The diabetic profiles, such as FPG, OGCT and HbA1c, showed a significant increase in GDM patients compared to healthy, non diabetic pregnant women. Galectin-3 levels and HOMA-IR values were significantly higher in GDM patients compared to those with normal pregnancies [Table/Fig-1]. There is no correlation between Galectin-3 and the indices of insulin resistance, including HOMA-IR and the TyG index [Table/Fig-2].
Demographic and biochemical characteristics of both GDM and normal healthy pregnant women.
| Parameters | GDM patients (n=40) | Normal pregnant women (n=40) | p-value |
|---|
| Gestational age (weeks) | 30.73±6.07 | 30.73±6.07 | 1.00 |
| Patient age (years) | 27.78±3.84 | 26.88±3.89 | 0.307 |
| BMI (current) kg/m2 | 29.5±5.4 | 27.0±4.7 | 0.035* |
| FPG (mg/dL) | 84.5 (74.5-97.25) | 77 (73.25-83.75) | 0.005* |
| OGCT (mg/dL) | 158 (158-183) | 104 (94-111.75) | 0.001* |
| HbA1c (%) | 5.4 (5.1-5.8) | 5.0 (4.82-5.2) | 0.002* |
| Fasting insulin (micro IU/mL) | 17.42 (9.89-27.38) | 12.65 (7.48-20.0) | 0.061 |
| Total cholesterol (mg/dL) | 217.5 (197-234) | 229 (202.25-254.25) | 0.137 |
| TGL (mg/dL) | 226 (184-281.75) | 189.5 (150.75-226.75) | 0.005* |
| LDL (mg/dL) | 135.56±31.16 | 150.63±36.29 | 0.053 |
| VLDL | 43.5 (35-56.2) | 37.9 (30.15-45.35) | 0.037* |
| HDL (mg/dL) | 63.75±8.87 | 64.1±13.08 | 0.890 |
| Galectin-3 (ng/mL) | 4.84±0.75 | 3.34±0.78 | 0.001* |
| HOMA IR | 3.78 (2.00-5.76) | 2.46 (1.30-3.83) | 0.019* |
| HOMA-β | 311.29 (179.63-427.14) | 330.98 (162.17-583.80) | 0.672 |
| TyG index | 4.95±0.20 | 4.78±0.15 | <0.001* |
BMI: Body mass index; FPG: Fasting plasma glucose; OGCT: Oral glucose challenge test; HbA1c: Glycated haemoglobin; HOMA-IR: Homeostatic model assessment for insulin resistance; HOMA-β: Homeostatic model assessment for β cell function; TGL: Triglycerides; LDL: Low density lipoprotein; VLDL: Very low density lipoprotein; HDL: High density lipoprotein
Data are expressed as mean±SD for parametric variables and median (interquartile ranges) for non parametric variables. Independent student’s t test: *p-value <0.05 is considered significant. Mann-Whitney U Test: *p-value 0.05 is considered significant
Correlation between Galectin-3 and insulin resistance in GDM patients.
| Parameters | | HOMA IR | TyG index |
|---|
| Galectin-3 | r value | -0.075 | -0.057 |
| p-value | 0.645 | 0.729 |
HOMA-IR: Homeostatic model assessment for insulin resistance; r value: Correlation coefficient
Pearson’s correlation: *p-value <0.05 is considered significant
Discussion
The GDM poses adverse health effects not only to the mother in the form of future T2DM risk but also for the newborn. The present study comparing women with GDM and those with normal pregnancies showed that women with GDM had a higher current BMI. By analysing National Family Health Survey data, comprising nearly 30,000 pregnant women, Chakraborty A and Yadav S identified BMI as one of the strong risk factors for GDM in Indian women [26]. Another recent study from Rajasthan concurred that a strong association exists between higher BMI and the development of GDM [27]. Elevated FPG and OGCT values suggest impaired glucose regulation and tolerance in GDM, while higher HbA1c levels indicate suboptimal long-term glycaemic control. Rajput R et al., suggested that OGTT should be performed in pregnant women with HbA1c levels between 5.45% and 5.95% for the diagnosis of GDM [28]. The TyG index, which is considered a surrogate marker of insulin resistance, was significantly increased in women with GDM. This strengthens the evidence for the potential role of insulin resistance in the pathogenesis of GDM [29]. These distinct metabolic characteristics associated with GDM emphasise the importance of early detection and targeted management strategies to mitigate adverse pregnancy outcomes. The presence of GDM suggests an altered metabolic profile during pregnancy, reflecting a potential predisposition to diabetes [30]. HOMA-β, an indicator of insulin secretion, was comparable between the two groups. Similar findings were reported by Zhang Z et al., [31].
In contrast to the present findings, Baldane S et al., showed lower HOMA-β levels in GDM patients but did not find a correlation with Galectin-3 levels and concluded that this lectin may not be involved in the impairment of insulin secretion [32]. However, the authors found no correlation between Galectin-3 and HOMA-β, aligning with the findings of Zhang Z et al., [31]. This suggests the potential existence of alternative metabolic pathways through which Galectin-3 may directly influence GDM. Heusler I et al., observed higher Galectin-3 mRNA expression in the maternal circulation and placenta of GDM patients [33]. Elevated levels of Galectin-3 in individuals with GDM indicate a potential association with an increased risk of developing the condition. This observation underscores the possibility that increased Galectin-3 levels may contribute to the onset of insulin resistance and subsequent DM [34]. HOMA-IR levels were elevated in pregnant women with GDM. The malfunctioning of beta cells, coupled with persistent insulin resistance throughout pregnancy, leads to impaired beta cell function and tissue insulin resistance. These factors are pivotal aspects of GDM pathophysiology [35].
Galectin-3 gene knock-out mice did not develop insulin resistance following a high-fat diet, indicating a potential link between Galectin-3 and insulin resistance [33]. Although markers of insulin resistance, like HOMA-IR and the TyG index, were significantly increased in GDM patients in our study, we could not establish a significant correlation between Galectin-3 and insulin resistance markers. In-vitro studies on 3T3-L1 adipocytes treated with Galectin-3 showed a reduction in insulin-stimulated Glucose Transporter type 4 (GLUT4) translocation [36]. A positive correlation between Galectin-3 and insulin resistance was also reflected in women with PCOS [37]. In contrast, Freitag N et al., did not identify any differences in Galectin-3 levels between normal and GDM pregnancies in the first and second trimesters and found a decrease in Galectin-3 levels in the third trimester [38]. Talmor-Barkan Y et al., recommended the utility of Galectin-3 levels in the first trimester to screen for GDM. Early detection of GDM plays a crucial role in implementing lifestyle modifications and treatments to prevent morbidity [21]. Literature findings suggest that Galectin-3 acts as a positive regulator of trophoblast functions and may be disrupted in GDM [38]. Authors who evaluated trophoblastic functions through exogenous Galectin-3 stimulation in cell culture combined these findings with serum results, suggesting a potential link between GDM and elevated serum Galectin-3 levels in late gestation [38]. Therefore, further research is needed to explore this association.
Limitation(s)
Due to the cross-sectional nature of the study, a causal relationship could not be derived between Galectin-3 and development of GDM. The lack of a significant correlation between insulin resistance and Galectin-3 could be due to the limited sample size.
Conclusion(s)
The present study established the existence of insulin resistance and elevated Galectin-3 levels in pregnancies affected by GDM, but it could not demonstrate an association between them.
BMI: Body mass index; FPG: Fasting plasma glucose; OGCT: Oral glucose challenge test; HbA1c: Glycated haemoglobin; HOMA-IR: Homeostatic model assessment for insulin resistance; HOMA-β: Homeostatic model assessment for β cell function; TGL: Triglycerides; LDL: Low density lipoprotein; VLDL: Very low density lipoprotein; HDL: High density lipoprotein
Data are expressed as mean±SD for parametric variables and median (interquartile ranges) for non parametric variables. Independent student’s t test: *p-value <0.05 is considered significant. Mann-Whitney U Test: *p-value 0.05 is considered significant
HOMA-IR: Homeostatic model assessment for insulin resistance; r value: Correlation coefficient
Pearson’s correlation: *p-value <0.05 is considered significant
[1]. Metzger BE, Lowe LP, Dyer AR, Trimble ER, Chaovarindr U, Coustan DR, HAPO Study Cooperative Research GroupHyperglycemia and adverse pregnancy outcomesObstetric Anesthesia Digest 2009 29(1):39-40.10.1097/01.aoa.0000344706.95925.dc [Google Scholar] [CrossRef]
[2]. Falavigna M, Schmidt MI, Trujillo J, Alves LF, Wendland ER, Torloni MR, Effectiveness of gestational diabetes treatment: A systematic review with quality of evidence assessmentDiabetes Res Clin Pract 2012 98(3):396-405.10.1016/j.diabres.2012.09.00223031412 [Google Scholar] [CrossRef] [PubMed]
[3]. Lowe WL, Scholtens DM, Lowe LP, Kuang A, Nodzenski M, Talbot O, Association of Gestational Diabetes with maternal disorders of glucose metabolism and childhood adiposityJAMA 2018 320(10):1005-16.10.1001/jama.2018.1162830208453PMC6143108 [Google Scholar] [CrossRef] [PubMed]
[4]. Pettitt DJ, Knowler WC, Long-term effects of the intrauterine environment, birth weight, and breast-feeding in Pima IndiansDiabetes Care 1998 21(2):B138-41.10.1007/978-1-4757-6752-0_15 [Google Scholar] [CrossRef]
[5]. Szmuilowicz ED, Josefson JL, Metzger BE, Gestational diabetes mellitusEndocrinol Metab Clin North Am 2019 48(3):479-93.10.1016/j.ecl.2019.05.00131345518PMC7008467 [Google Scholar] [CrossRef] [PubMed]
[6]. Alejandro EU, Mamerto TP, Chung G, Villavieja A, Gaus NL, Morgan E, Gestational diabetes mellitus: A harbinger of the vicious cycle of diabetesInt J Mol Sci 2020 21(14):500310.3390/ijms2114500332679915PMC7404253 [Google Scholar] [CrossRef] [PubMed]
[7]. Stanley JL, Cheung CC, Rueda-Clausen CF, Sankaralingam S, Baker PN, Davidge ST, Effect of gestational diabetes on maternal artery functionReprod Sci 2011 18(4):342-52.10.1177/193371911039302921266665 [Google Scholar] [CrossRef] [PubMed]
[8]. Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, Freeman R, 2. Classification and Diagnosis of Diabetes: Standards of medical care in diabetes-2022Diabetes Care 2022 45(Suppl 1):S17-S38.10.2337/dc22-S00234964875 [Google Scholar] [CrossRef] [PubMed]
[9]. Agarwal S, Gupta AN, Gestational diabetesJ Assoc Physicians India 1982 30(4):203-05. [Google Scholar]
[10]. Seshiah V, Balaji V, Balaji MS, Paneerselvam A, Arthi T, Thamizharasi M, Prevalence of gestational diabetes mellitus in South India (Tamil Nadu)--A community-based studyJ Assoc Physicians India 2008 56:329-33. [Google Scholar]
[11]. Zargar AH, Sheikh MI, Bashir MI, Masoodi SR, Laway BA, Wani AI, Prevalence of gestational diabetes mellitus in Kashmiri women from the Indian subcontinentDiabetes Res Clin Pract 2004 66(2):139-45.10.1016/j.diabres.2004.02.02315533581 [Google Scholar] [CrossRef] [PubMed]
[12]. Unnikrishnan R, Anjana RM, Mohan V, Diabetes mellitus and its complications in IndiaNat Rev Endocrinol 2016 12(6):357-70.10.1038/nrendo.2016.5327080137 [Google Scholar] [CrossRef] [PubMed]
[13]. Menon RP, Hughes RC, Determinants in the N-terminal domains of galectin-3 for secretion by a novel pathway circumventing the endoplasmic reticulum-Golgi complexEur J Biochem 1999 264(2):569-76.10.1046/j.1432-1327.1999.00671.x10491105 [Google Scholar] [CrossRef] [PubMed]
[14]. Friedrichs J, Manninen A, Muller DJ, Helenius J, Galectin-3 regulates integrin alpha2beta1-mediated adhesion to collagen-I and -IVJ Biol Chem 2008 283(47):32264-72.10.1074/jbc.M80363420018806266 [Google Scholar] [CrossRef] [PubMed]
[15]. Nio J, Takahashi-Iwanaga H, Morimatsu M, Kon Y, Iwanaga T, Immunohistochemical and in situ hybridization analysis of galectin-3, a beta-galactoside binding lectin, in the urinary system of adult miceHistochem Cell Biol 2006 126(1):45-56.10.1007/s00418-005-0142-516404573 [Google Scholar] [CrossRef] [PubMed]
[16]. Schwaderer AL, Vijayakumar S, Al-Awqati Q, Schwartz GJ, Galectin-3 expression is induced in renal beta-intercalated cells during metabolic acidosisAm J Physiol Renal Physiol 2006 290(1):F148-58.10.1152/ajprenal.00244.200516131647 [Google Scholar] [CrossRef] [PubMed]
[17]. Agha-Jaffar R, Oliver N, Johnston D, Robinson S, Gestational diabetes mellitus: Does an effective prevention strategy existNat Rev Endocrinol 2016 12(9):533-46.10.1038/nrendo.2016.8827339886 [Google Scholar] [CrossRef] [PubMed]
[18]. Song C, Lyu Y, Li C, Liu P, Li J, Ma RC, Long-term risk of diabetes in women at varying durations after gestational diabetes: A systematic review and meta-analysis with more than 2 million womenObes Rev 2018 19(3):421-29.10.1111/obr.1264529266655 [Google Scholar] [CrossRef] [PubMed]
[19]. Homko C, Sivan E, Chen X, Reece EA, Boden G, Insulin secretion during and after pregnancy in patients with gestational diabetes mellitusJ Clin Endocrinol Metab 2001 86(2):568-73.10.1210/jc.86.2.56811158010 [Google Scholar] [CrossRef] [PubMed]
[20]. Yang H, Taylor HS, Lei C, Cheng C, Zhang W, Hormonal regulation of galectin 3 in trophoblasts and its effects on endometriumReprod Sci 2011 18(11):1118-27.10.1177/193371911140721221555510 [Google Scholar] [CrossRef] [PubMed]
[21]. Talmor-Barkan Y, Chezar-Azerrad C, Kruchin B, Leshem-Lev D, Levi A, Hadar E, Elevated galectin-3 in women with gestational diabetes mellitus, a new surrogate for cardiovascular disease in womenPLoS One 2020 15(6):e023473210.1371/journal.pone.023473232555606PMC7299386 [Google Scholar] [CrossRef] [PubMed]
[22]. Tang T, Chen L, Correlation between serum ApoC III and Galectin-3 levels and maternal and neonatal adverse outcomes in gestational diabetes Mellitus PatientsEmerg Med Int 2022 2022:5089529Available from: https://doi.org/10.1155/2022/508952910.1155/2022/508952936247704PMC9553661 [Google Scholar] [CrossRef] [PubMed]
[23]. Seshiah V, Das AK, Balaji V, Joshi SR, Parikh MN, Gupta S, Diabetes in pregnancy study groupGestational diabetes mellitus--guidelinesJ Assoc Physicians India 2006 54:622-28. [Google Scholar]
[24]. Wallace TM, Levy JC, Matthews DR, Use and abuse of HOMA modellingDiabetes Care 2004 27(6):1487-95.10.2337/diacare.27.6.148715161807 [Google Scholar] [CrossRef] [PubMed]
[25]. Khalaji A, Behnoush AH, Khanmohammadi S, Ghanbari Mardasi K, Sharifkashani S, Sahebkar A, Triglyceride-glucose index and heart failure: A systematic review and meta-analysisCardiovasc Diabetol 2023 22(1):24410.1186/s12933-023-01973-737679763PMC10486123 [Google Scholar] [CrossRef] [PubMed]
[26]. Chakraborty A, Yadav S, Prevalence and determinants of gestational diabetes mellitus among pregnant women in India: An analysis of National Family Health Survey DataBMC Womens Health 2024 24(1):14710.1186/s12905-024-02936-038424617PMC10902981 [Google Scholar] [CrossRef] [PubMed]
[27]. Patwa P, Sharma C, Shekhar S, Singh P, Gupta N, Ghuman NK, Association of body mass index with gestational diabetes mellitus—An Indian viewpointSN Comprehensive Clinical Medicine 2022 4(1):18010.1007/s42399-022-01263-5 [Google Scholar] [CrossRef]
[28]. Rajput R, Rajput M, Nanda S, Utility of HbA1c for diagnosis of gestational diabetes mellitusDiabetes Res Clin Pract 2012 98(1):104-07.10.1016/j.diabres.2012.02.01822456454 [Google Scholar] [CrossRef] [PubMed]
[29]. Kim JA, Kim J, Roh E, Hong SH, Lee YB, Baik SH, Triglyceride and glucose index and the risk of gestational diabetes mellitus: A nationwide population-based cohort studyDiabetes Res Clin Pract 2021 171:10853310.1016/j.diabres.2020.10853333157117 [Google Scholar] [CrossRef] [PubMed]
[30]. Lowe WL Jr, Karban J, Genetics, genomics and metabolomics: New insights into maternal metabolism during pregnancyDiabet Med 2014 31(3):254-62.10.1111/dme.1235224528228PMC3927230 [Google Scholar] [CrossRef] [PubMed]
[31]. Zhang Z, Kang X, Guo Y, Zhang J, Xie J, Shao S, Association of circulating galectin-3 with gestational diabetes mellitus, progesterone, and insulin resistanceJ Diabetes 2021 13(1):54-62.10.1111/1753-0407.1308832671973 [Google Scholar] [CrossRef] [PubMed]
[32]. Baldane S, Celik M, Korez MK, Baldane EG, Abusoglu S, Ali U, Assessment of Serum Galectin-3 levels in patients with gestational diabetes mellitusJ Diabetol 2023 14(1):28-33.10.4103/jod.jod_84_22 [Google Scholar] [CrossRef]
[33]. Heusler I, Biron-Shental T, Farladansky-Gershnabel S, Pasternak Y, Kidron D, Vulih-Shuitsman I, Enhanced expression of galectin-3 in gestational diabetesNutr Metab Cardiovasc Dis 2021 31(6):1791-97.10.1016/j.numecd.2021.03.00234023181 [Google Scholar] [CrossRef] [PubMed]
[34]. Li P, Liu S, Lu M, Bandyopadhyay G, Oh D, Imamura T, Hematopoietic-derived galectin-3 causes cellular and systemic insulin resistanceCell 2016 167(4):973-84.10.1016/j.cell.2016.10.02527814523PMC5179329 [Google Scholar] [CrossRef] [PubMed]
[35]. Hu J, Gillies CL, Lin S, Stewart ZA, Melford SE, Abrams KR, Association of maternal lipid profile and gestational diabetes mellitus: A systematic review and meta-analysis of 292 studies and 97,880 womenEclinical Medicine 2021 34:10083010.1016/j.eclinm.2021.10083033997732PMC8102708 [Google Scholar] [CrossRef] [PubMed]
[36]. Siwicki M, Engblom C, Pittet MJ, Gal3 links inflammation and insulin resistanceCell Metab 2016 24(5):655-56.10.1016/j.cmet.2016.10.01427829136 [Google Scholar] [CrossRef] [PubMed]
[37]. Yilmaz H, Cakmak M, Inan O, Darcin T, Akcay A, Increased levels of galectin-3 were associated with prediabetes and diabetes: New risk factor?J Endocrinol Invest 2015 38(5):527-33.Epub 2014 Dec 1210.1007/s40618-014-0222-225501605 [Google Scholar] [CrossRef] [PubMed]
[38]. Freitag N, Tirado-González I, Barrientos G, Cohen M, Daher S, Goldman-Wohl D, The chimera-type galectin-3 is a positive modulator of trophoblast functions with dysregulated expression in gestational diabetes mellitusAm J Reprod Immunol 2020 84(6):e1331110.1111/aji.1331132691950 [Google Scholar] [CrossRef] [PubMed]