Dermatofibrosarcoma Protuberans (DFSP) is a low-grade cutaneous soft-tissue sarcoma that originates in the dermis and infiltrates deeper structures. It comprises less than one percent of all soft-tissue sarcomas and is histologically defined by their slow growth, localised invasiveness and a tendency to recur when not adequately excised. However, unlike other cancers, distant metastasis is relatively uncommon; the invasive nature of DFSP infiltration causes diagnostic and therapeutic challenges. DFSP can involve any area of the body; however, it predominantly favours the trunk and extremities. The mainstay of management is wide local excision, which should achieve negative margins, as inadequate margins have a propensity to recur. Recurrent cases require specific surgical management to balance oncological security with the management of their consequences. The presented case involves a 72-year-old man with recurrent DFSP, manifesting as a long-standing swelling of the left great toe that progressively increased over 10 years. Initially, conservative treatment was attempted, but the condition became symptomatic, leading to excision and a diagnosis of Chronic Granulomatous Changes (CGC) and liquefactive necrosis. Although the swelling was initially excised, it recurred after eight months and was treated by amputation due to its aggressive nature and the impossibility of definitive resection. Radical surgical re-intervention for wound dehiscence, which later reopened, was supplemented by Split-thickness Skin Grafting (SSG). In the management of recurrent soft-tissue tumours, early diagnosis and individualised treatment planning should be emphasised to maximise patient outcomes and minimise recurrence.
Case Report
A 72-year-old male presented to the Outpatient Department (OPD) with a complaint of longstanding swelling in the left great toe. Initially, the swelling was quite indistinct and grew slowly over 10 years, eventually reaching a prominent size and being associated with sharp, needle-like pain. The patient has a significant past medical history of leprosy, which was managed and resolved 25 years ago, with no recurrence or other co-morbidities observed after the completion of treatment and subsequent remission. During the physical examination, a solitary, skin-coloured swelling was noted in the left great tarsal region, measuring 4×3 cm, as shown in [Table/Fig-1].
A solitary, skin-coloured swelling was noted within the left great tarsal region.

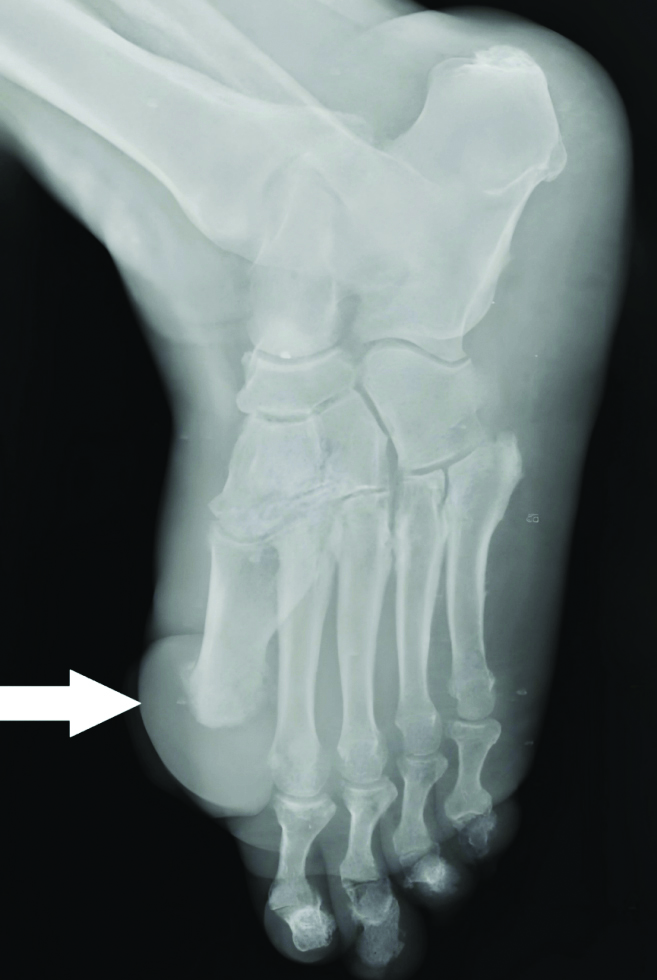
The swelling was globular in shape, glossy and non tender on palpation. It was firm in consistency, immobile and appeared fixed to the underlying cartilage. The overlying skin did not exhibit erythema or oedema and the degree of swelling was not accompanied by any changes related to an adjacent joint. In the standard weight-bearing X-ray of the left foot, there was no direct involvement of the left foot bones; however, the soft-tissue density at the site of the swelling was marginally elevated, as shown in [Table/Fig-2]. There was no evidence of bone erosion, fracture, subluxation, dislocation, or calcification within the lesion, thus limiting the differential diagnosis to soft-tissue pathology.
X-ray of the left foot of patient showing elevated soft-tissue density at site of swelling.
The patient was informed about his treatment options after an extensive discussion regarding the swelling and surgical excision was preferred as the swelling had become uncomfortable and was gradually growing. Following complete excision of the swelling, the specimen was placed in 10% neutral buffered formalin as soon as possible for block processing and histopathological analysis. The condition of the swelling one day post-excision is shown in [Table/Fig-3].
The condition of swelling after one day of excision.

Histopathologically, the tumour was first reported as liquefactive necrosis with underlying granulation tissue, along with dead bony spicules, foci of cartilage and extensive areas of active granulation tissue, i.e., Chronic Granulomatous Changes (CGC). After 9 to 10 months postsurgery, the patient returned with a similar swelling in the same affected area. The recurrent swelling displayed characteristics similar to those during the initial presentation; it was firm, non tender and exhibited deep attachment to the surrounding soft tissues. The recurrent swelling of the patient is shown in [Table/Fig-4].
The recurrent swelling of the patient.

This recurrence indicated the possibility of an aggressive or infiltrative nature of the lesion. A more radical surgical intervention, namely amputation of the left great toe with disarticulation of the first metatarsal-phalangeal joint, was planned to ensure negative histology on the margins and thereby control the disease.
The patient was then placed under anaesthesia to allow for optimal positioning of the affected region. A circumferential incision was made around the base of the great toe, extending through the skin and subcutaneous tissues, with wide margins to include the tumour and surrounding soft tissue. Dissection proceeded carefully around the swelling, ensuring the preservation of nearby neurovascular structures while maintaining adequate oncological margins. Additional structures excised in this case included the deeper attachments involving partial plantar ligamentous and capsular structures to avoid the spread of the condition.
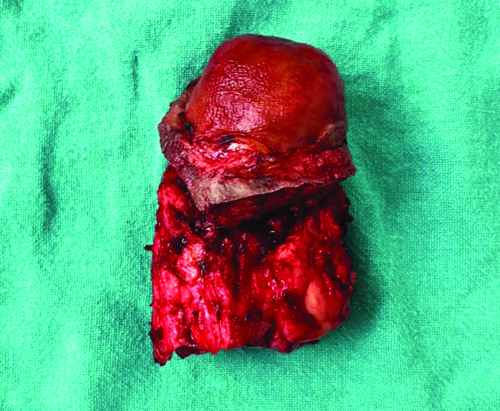
The swelling was then dissected out and the associated toe tissue, including the proximal phalanx, was resected, leaving behind healthy tissue margins for oncological clearance. Haemostasis was achieved and the wound was closed in layers to promote healing and minimise the risk of infection. The wound was cleaned, sterile dressings were applied and the patient was discharged with appropriate instructions regarding foot care and limitations on physical activity. The tissue sample that was removed was immersed in 10% neutral buffered formalin for histopathological analysis, which subsequently confirmed complete tumour removal with no evidence of residual disease. The amputated part of the patient is presented in [Table/Fig-5].
The amputated part of patient.
The histopathological diagnosis was more in line with Dermatofibrosarcoma Protuberans (DFSP), a low-grade malignant fibrous histiocytoma (spindle cell tumour) that has a propensity to recur. The revised diagnosis emphasised the importance of detailed histopathological examination and underscored the diagnostic challenges associated with soft-tissue tumours. A complication of postoperative wound dehiscence occurred after the amputation of the left great toe with disarticulation of the first metatarsal-phalangeal joint; as a result, a SSG procedure was performed to ensure proper closure and facilitate healing. The SSG of the patient is presented in [Table/Fig-6].
The Split-thickness Skin Graft (SSG) of patient.

Following the surgery, the graft was monitored for complications such as infection and the development of a haematoma or seroma. After confirming adequate graft integration and early signs of wound healing, the patient was discharged with detailed instructions regarding self-care for both the graft and donor areas. The patient is currently under follow-up and is doing well.
Discussion
Swelling of the great toe may result from various causes, including injury or trauma, such as a sprain, fracture, or blunt impact [1,2]. It can also be due to bacterial and fungal infections, leading to conditions like cellulitis or paronychia [2,3]. Poor circulation, venous insufficiency and blood clots can also cause swelling in the toes due to circulatory conditions [4]. Typical symptoms include redness, warmth, pain and, in some cases, immobility [1,4].
Leprosy is a chronic infectious disease caused by Mycobacterium leprae [5]. In comparison to the toe or other extremities, nerve damage resulting from leprosy may impair sensation in this region [5]. This means that these areas become insensitive to injury or infection and patients may easily get hurt or infected in sensitive regions without noticing it [5,6]. In due course, this can lead to ulcers, deformities and tissue damage; if untreated, digits or limbs may eventually be lost [6]. Granulomatous changes are noted during most chronic infectious diseases, like leprosy and tuberculosis, while some non infectious diseases include Crohn’s disease [7].
The DFSP is a rare, slowly growing soft-tissue sarcoma originating in the skin’s dermal layer, extending into deeper tissues with infiltration of subcutaneous tissue and sometimes reaching the muscular layer [8]. Distant metastasis is a rare occurrence for DFSP; however, it does have a locally aggressive nature [9].
The case of a 32-year-old Indian man reported by Shah SR et al., with a recurrent swelling on his left loin and the case of a 72-year-old man with a recurring swelling on his left great toe illustrate notable similarities and differences in the presentation and management of soft-tissue tumours [10]. In both cases, there was a history of recurrent, slow-growing swellings accompanied by sharp pricking pain. Both lesions were firm in consistency and deeply attached to the surrounding soft tissues. Histopathological examination highlighted the diagnostic challenges of soft-tissue tumours in both cases as the diagnosis needed to be differentiated from other malignant mesenchymal tumours [10].
Matias M et al., reported a case of a 48-year-old woman from Brazil who presented with a small, asymptomatic swelling on the dorsum of her foot, which was diagnosed as DFSP, a rare, low-grade malignant soft-tissue tumour [11]. The patient underwent an incisional biopsy coupled with a limb and cervico-thoraco-abdominal Computed Tomography (CT) scan, wherein no distant metastasis was confirmed [11]. A wide local excision with 4 cm margins led to the ray amputation of the second and third toes, with caution taken regarding the neurovascular structures [11]. Postoperative care included immobilisation, supported walking with two crutches and gabapentin for neuropathic pain [11]. Definitive histopathology revealed complete resection of the tumour and no evidence of residual disease [11].
The case of a 39-year-old male from the United States, as reported by Madden C et al., and the presented 72-year-old male patient present distinct yet comparable clinical scenarios of soft-tissue swellings affecting the hallux [12]. The 39-year-old male patient reported by Madden C et al., exhibited a 3.5-year history of a gradually enlarging, pain-associated subcutaneous swelling on the right dorsal hallux, which, upon excision, was diagnosed as DFSP [12]. Histopathological examination revealed monomorphic spindle cells arranged in a storiform pattern with infiltration into adjacent adipose tissue, highlighting its infiltrative nature [12]. In contrast, the presented 72-year-old male had a long-standing swelling on the left great toe that had been growing for 10 years, initially presenting as non tender but later becoming associated with sharp pain.
The case of the 44-year-old Indian woman reported by Yadav S et al., and the case presented here of the 72-year-old man show two different clinical profiles of DFSP, illustrating both similarities and differences [13]. While the case of DFSP in a 52-year-old female by Bakry O and Attia A exhibited a slow-growing, asymptomatic lesion that was successfully treated with surgical excision [14], the case presented here required more aggressive intervention, including amputation, due to its infiltrative nature. A comparative analysis of the present case and previously published cases is presented in [Table/Fig-7] [10-14].
Comparative analysis of the present case and cases published in the past [10-14].
| Aspect | Present case | Shah SR et al., [10] | Matias M et al., [11] | Madden C et al., [12] | Yadav S et al., [13] | Bakry O and Attia A [14] |
|---|
| Demographics | 72-year-old, male- India | 32-year-old, male-India | 48-year-old, female- Brazil | 39-year-old, male- United States | 44-year-old, female- India | 52-year-old, female- Egypt |
| Clinical presentation | Long-standing, firm, skin-coloured swelling on left great toe, associated with pain | Recurrent swelling on left loin, slow-growing, firm, painful | Small, asymptomatic swelling on dorsum of foot | Gradually enlarging, painful subcutaneous swelling on dorsal hallux | Recurrent DFSP on right upper arm | Long-standing, asymptomatic violaceous plaque on left buttock |
| Imaging studies | No bone involvement, soft-tissue density elevation | Magnetic Resonance Imaging (MRI) performed to assess lesion | CT scan confirmed no distant metastasis | Imaging not detailed | Imaging revealed well-defined soft-tissue swelling | Imaging not detailed |
| Histopathology | DFSP, liquefactive necrosis, Chronic Granulomatous Changes (CGC) | DFSP, aggressive features noted | DFSP, complete excision confirmed | DFSP, monomorphic spindle cells in storiform pattern | DFSP, clear margins post-excision | DFSP with storiform pattern of spindle-shaped cells in fibrous stroma |
| Initial surgical intervention | Surgical excision with amputation due to recurrence | Surgical excision with 3 cm margin | Wide local excision with neurovascular preservation | Successful excision without complications | Surgical excision with clear margins | Surgical excision with a 3 cm safety margin |
| Postoperative outcomes | Amputation due to recurrence, wound dehiscence requiring Split-thickness Skin Graft (SSG) | No immediate complications reported | Successful recovery, no complications | No complications during follow-up | Remained symptom-free at six-month follow-up | Successful excision, no recurrence reported |
| Clinical insights | Aggressive nature of DFSP in older patients, need for vigilant follow-up | Importance of timely intervention in recurrent cases | Early diagnosis led to better outcomes | Recognition of DFSP characteristics for timely diagnosis | Importance of monitoring in recurrent cases | Importance of early diagnosis and intervention |
The DFSP and other soft-tissue sarcomas were considered in the differential diagnosis due to the lesion’s slow-growing, firm and non mobile characteristics. Chronic granulomatous infections, like tuberculosis and fungal diseases with dementia as features, were also considered because the patient had a history of leprosy; however, histopathological analysis revealed no fungal forms and granulomas were not typical of atypical mycobacterial infections. Giant cell tumour of soft tissue was ruled out as no multinucleated giant cells were observed under histopathological examination. Due to the lesion’s hardness and lack of mobility, lipomatous tumours like lipoma or more malignant liposarcoma were also ruled out, as this was evident from the histologic examination. Peripheral nerve sheath tumours and synovitis-like reactive lesions were other diagnosis considered and excluded owing to the lack of synovitis, cystic changes and lack of Verocay bodies/Antoni patterns on histology.
Conclusion(s)
The present case demonstrates the critical importance of histopathological assessment, timely intervention and close follow-up in older patients to improve outcomes and prevent recurrence of DFSP. Future management should focus more on thorough assessments and more individualised surgical planning.
[1]. Everett J, Lawrance S, Cooper K, Phillips N, The assessment and management of foot and toe oedema as part of holistic lower limb careBr J Community Nurs 2024 29(Sup4):S6-13.10.12968/bjcn.2024.29.Sup4.S638578926 [Google Scholar] [CrossRef] [PubMed]
[2]. Flores DV, Chronic swelling of the footSkeletal Radiol 2017 46(7):1017-18.10.1007/s00256-017-2641-6 [Google Scholar] [CrossRef]
[3]. Hirschmann JV, Raugi GJ, Lower limb cellulitis and its mimics: Part I. Lower limb cellulitisJ Am Acad Dermatol 2012 67(2):163.e1-12.quiz 175-7610.1016/j.jaad.2012.03.02422794815 [Google Scholar] [CrossRef] [PubMed]
[4]. Tengattini V, Magnano M, Patrizi A, Neri I, Sudden swelling and redness of the toeClin Case Rep 2017 5(11):1901-02.10.1002/ccr3.111529152297PMC5676277 [Google Scholar] [CrossRef] [PubMed]
[5]. Godron J, de Lambilly C, Cournac JM, Valois A, Tuan Nguyen A, Michoud G, Edema of limbs indicative of leprosyRev Prat 2023 73(9):988-90. [Google Scholar]
[6]. Scollard DM, The biology of nerve injury in leprosyLepr Rev 2008 79(3):242-53.10.47276/lr.79.3.24219009974 [Google Scholar] [CrossRef] [PubMed]
[7]. Bhatia S, Shenoi SD, Pai K, Ps S, Granuloma multiforme: An uncommon differential for leprosyTrop Doct 2019 49(1):55-58.10.1177/004947551880319130286700 [Google Scholar] [CrossRef] [PubMed]
[8]. Vitiello GA, Lee AY, Berman RS, Dermatofibrosarcoma protuberans: What is this?Surg Clin North Am 2022 102(4):657-65.10.1016/j.suc.2022.05.00435952694 [Google Scholar] [CrossRef] [PubMed]
[9]. Penel N, El Bedoui S, Robin YM, Decanter G, Dermatofibrosarcome: Prise en charge [Dermatofibrosarcoma: Management]Bull Cancer 2018 105(11):1094-101.10.1016/j.bulcan.2018.08.00830297237 [Google Scholar] [CrossRef] [PubMed]
[10]. Shah SR, Regmee S, Maharjan DK, Thapa PB, Recurrent dermatofibrosarcoma protuberance: A case reportJNMA J Nepal Med Assoc 2021 59(243):1192-95.10.31729/jnma.718735199742PMC9124319 [Google Scholar] [CrossRef] [PubMed]
[11]. Matias M, Verissimo M, Barbosa R, Casal D, Case report: Dermatofibrosarcoma protuberans of the foot: What steps can we take?Int J Surg Case Rep 2023 111:10866710.1016/j.ijscr.2023.10866737716054PMC10514428 [Google Scholar] [CrossRef] [PubMed]
[12]. Madden C, Spector A, Siddiqui S, Mirkin G, Yim J, Hao X, Dermatofibrosarcoma protuberans on adult toes: A case report and review of the literatureAnticancer Res 2019 39(4):2105-11.10.21873/anticanres.1332330952756 [Google Scholar] [CrossRef] [PubMed]
[13]. Yadav S, Verma N, Khurana N, Neogi S, Recurrent dermatofibrosarcoma protuberans with pigmentation and myoid differentiationSultan Qaboos Univ Med J 2018 18(2):e228-30.10.18295/squmj.2018.18.02.01930210857PMC6132508 [Google Scholar] [CrossRef] [PubMed]
[14]. Bakry O, Attia A, Atrophic dermatofibrosarcoma protuberansJ Dermatol Case Rep 2012 6(1):14-17.10.3315/jdcr.2012.108922514584PMC3322104 [Google Scholar] [CrossRef] [PubMed]