Deep Vein Thrombosis (DVT), a subtype of Venous Thromboembolism (VT) is more likely to occur in areas such as the lower leg, thigh or pelvis when vessel wall damage, blood flow stasis and hypercoagulability are present. Untreated DVT in the lower extremities can enlarge and result in further complications such as Post Thrombotic Syndrome (PTS) and an elevated risk of pulmonary thromboembolism. Prothrombotic anomalies may arise as a result of a variety of circumstances including the degree and type of infection, inflammation, bed rest, the use of mechanical ventilators and venous catheterisation. The rise in DVT cases in recent years along with thrombus complications in various patient populations calls for customised DVT care and intervention. This research was carried out on a young man without any notable medical history and no history of addictions who arrived complaining of severe swelling that had developed over the course of a day, affecting his left lower limb. A bilateral lower limb doppler ultrasound suggested thrombosis in the popliteal vein, great saphenous vein, deep femoral vein and common femoral vein in the left lower limb. Low molecular weight heparin injection was used to treat the patient. However, as the patient had not shown any significant signs of clinical improvement, an Inferior Vena Cava (IVC) filter was inserted to prevent pulmonary thromboembolism, and catheter-based thrombolysis was performed to break down clots and restore blood flow, thereby reducing the risk of long-term complications like PTS. Following recovery, the patient was discharged on oral anticoagulants and is currently on regular follow-up.
Case Report
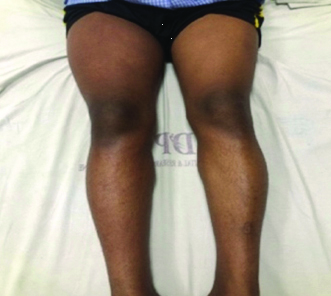
A 21-year-old man presented with the complaint of the abrupt onset of significant swelling in his left lower limb [Table/Fig-1], which had developed over the course of a day and was associated with pain. The pain was acute in onset, progressive in nature, excruciating in intensity, radiating from the feet to the hip, aggravating with movement and not relieved by rest. There was no history of fever, palpitations, dysopnea, chest pain, or addictions in the past. The patient followed a vegetarian diet.
Massive swelling of left lower limb.

On general examination, his pulse was 140 beats per minute, regular, with no radiofemoral delay and palpable in all peripheral areas. Blood pressure was 110/70 mmHg in the right arm while in a supine position. The respiratory rate was 20 breaths per minute, and oxygen saturation on room air was 98%. On the left lower leg, there was pitting oedema, with the peripheries being cold and significant tenderness at the site of swelling. No abnormalities were detected on examination of the other systems.
Laboratory tests revealed a total leukocyte count of 9,000/mm3 (Normal range 4000-10000/mm3), platelets of 248,000/mm3 (Normal range 150000-450000 mm3), and haemoglobin of 13.4 g/dL (Normal range 12-16 g/dL). Serum electrolytes, serum proteins, urine routine and microscopy, renal function tests, liver function tests, thyroid function tests, fasting lipid profile and serum fibrinogen were all within normal ranges. The patient was negative for serological status. Further laboratory investigations showed a D-dimer level of 2,046 ng/mL (Normal range 0-500 ng/mL), activated Partial Thromboplastin Time (aPTT) of 20.0 seconds (Normal range 28.05-36.00 seconds), Prothrombin Time-International Normalised Ratio (PT-INR) of 12.4 seconds/1.07 seconds (10.35-12.90 seconds/0.85-1.15 ISI), serum homocysteine >50 (Normal range 0-15 mcmol/L), serum vitamin B12 of 142 pg/mL (Normal range 183-887 pg/mL), ANA blot for SS-B/La antigen, and ANA immunofluorescence showing a 1:160 speckled pattern. Antiphospholipid antigen profiles (Beta 2 Glycoprotein 1 [IgM/IgG], Cardiolipin antibody [IgM/IgG], Lupus anticoagulant), thrombophilia profiles (Activated Protein C Resistance [APCR], Protein S Activity, Antithrombin III activity), cytoplasmic antineutrophil cytoplasmic antibodies and perinuclear antineutrophil cytoplasmic antibodies were all negative.
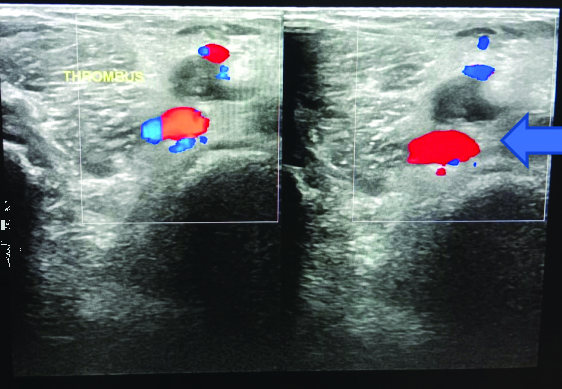
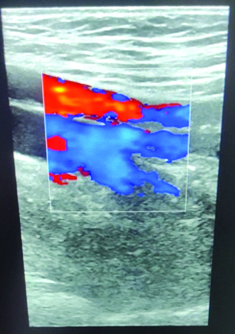
Sinus tachycardia was observed on electrocardiography. A two-dimensional echocardiogram, chest X-ray and ultrasonography of the pelvis and abdomen were within normal limits. Bilateral lower limb doppler ultrasound suggested patchy to no flow on colour doppler, indicating partial to near-total thrombosis in the left common femoral vein, superficial femoral vein, deep femoral vein, great saphenous vein and popliteal vein [Table/Fig-2]. The proximal external iliac vein appeared non compressible with echogenic content within.
Lower limb doppler image of thrombosis in left popliteal vein.
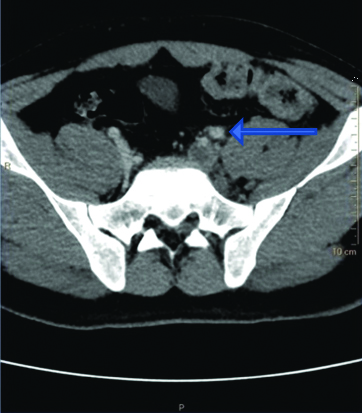
On postcontrast images from the aortogram and venogram obtained via Computed Tomography (CT), there was a hypodense filling defect visible in the left common iliac vein, left external iliac vein, left internal iliac vein, left superficial femoral vein left deep femoral vein, and left great saphenous vein, suggestive of thrombosis [Table/Fig-3]. The Wells score was 3 points, with 1 point each attributed for calf swelling greater than 3 cm compared to the asymptomatic calf, unilateral pitting oedema and swelling of the entire leg with localised tenderness along the deep venous system. A rheumatology opinion was sought for the ANA reports and they advised repeating the ANA profile after six weeks, which later came back negative.
CT axial section suggestive of hypodense filling defect in left common iliac vein causing left iliac vein thrombosis.
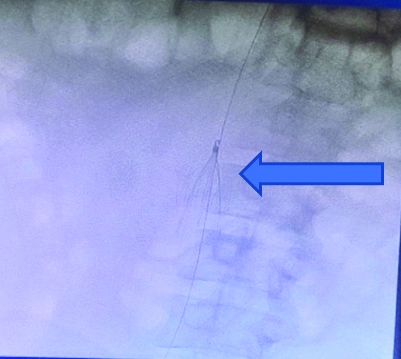
The patient was initially treated with 0.6 cc of enoxaparin subcutaneously twice a day, which is a common anticoagulant regimen to prevent clot extension and reduce the risk of pulmonary embolism. Vitamin B12 supplementation was provided to address the patient’s vitamin B12 deficiency. Magnesium Sulphate dressings, crepe bandaging and limb elevation were employed to help reduce swelling and alleviate pain associated with DVT. Despite the anticoagulation therapy, the patient’s symptoms, particularly pain and swelling, did not improve, indicating a significant clot burden or resistance to standard therapy. Therefore, he was planned for catheter-based thrombolysis and the insertion of an Inferior Vena Cava (IVC) filter. Right common femoral vein puncture was performed under ultrasound guidance, with the insertion of an 11 Fr sheath. The Bard Denali Filter [Table/Fig-4] was activated at the infrared wavelength. A left popliteal vein puncture was performed under ultrasound guidance, a 5 Fr sheath was inserted, and a 5 Fr pigtail multihole catheter was placed into the left common femoral vein and common iliac vein, after which thrombolysis infusion was started.
Showing in Bard Denali filter, being activated.
Postoperatively, the patient was given an injection of heparin infusion at 500 IU/hour through the sheath (5 mL=25,000 IU Heparin+45 mL NS@ 500 IU/hour=1 mL/hour) and an injection of alteplase infusion at 1 mg/hour through the catheter (20 mg in 20 mL NS=2 mL/hour). After catheter-guided thrombolysis and IVC filter insertion, the patient’s clinical condition improved.
At discharge, the patient was prescribed tablet rivaroxaban 15 mg twice a day and an oral tablet of vitamin B12 once a day. On subsequent follow-ups, the patient showed clinical improvement, with a significant reduction in leg swelling [Table/Fig-5] and resolution of thrombosis [Table/Fig-6], with no fresh complaints.
Significant reduction in swelling of left lower limb.
Showing significant resolution of thrombosis of portal vein.
Discussion
DVT is a major global health concern and one of the key preventable causes of morbidity and mortality. DVT is a form of VT that occurs when a blood clot forms in a deep vein, typically in the legs. If left untreated, DVT can lead to serious complications, the most severe being pulmonary embolism. Virchow’s Triad is a well-known model that explains the three broad categories of factors that contribute to thrombosis: stasis of blood flow, endothelial injury and hypercoagulability [1]. Unprovoked DVT, especially in patients under 30 years of age, is relatively rare. The cardinal signs and symptoms of DVT include asymmetrical swelling, warmth, or pain in an extremity [2]. The Wells criteria are the most prevalent criteria used to evaluate the pretest probability of DVT. Like the Wells scoring criteria, the D-dimer assay has high sensitivity (75-100%) but poor specificity (26-83%) [3]. In present report, the Wells score was found to be 3. For the diagnosis of DVT, a range of imaging modalities is available, with the choice depending on clinical suspicion, available resources and the patient’s condition. Colour-flow doppler ultrasound and ultrasonography are widely regarded as first-line tools for diagnosing proximal DVT, given their non invasive nature, high sensitivity and ease of use. However, the highest standard used is contrast venography, including venography using CT and venography using Magnetic Resonance (MR). As referenced in the study by Chan NC and Weitz JI, which utilised advanced imaging techniques like CT venography, these modalities offer enhanced detail and accuracy, especially in complicated cases or where the thrombus extends beyond what is visible with standard ultrasound techniques [4].
According to a study by Yamashita Y et al., medical management of DVT and its complications includes the injection of low molecular weight heparin and Direct Oral Anticoagulants (DOACs) like dabigatran, rivaroxaban and apixaban. In cases of extensive thrombus burden involving proximal deep veins, mechanical and catheter-directed thrombolysis may be indicated in the acute phase to rapidly induce clot lysis and reduce the risk of PTS, as was done in our case [5].
Indications for an IVC filter include anticoagulant contraindications, recurrent embolism, anticoagulant complications and prophylactic use after embolectomy. It has been reported that Candida can infect an IVC filter [6,7]. For severe and submassive pulmonary embolism with haemodynamic instability, catheter-directed thrombolysis provides an alternative revascularisation technique to systemic thrombolysis, transcatheter embolectomy, or surgical embolectomy. Common venous sites include the popliteal, jugular, femoral and tibial veins [8]. In a similar study, complications of catheter-directed thrombolysis included risks of bleeding, haematoma, pulmonary haemorrhage, cardiogenic shock, and contrast-induced nephropathy. Contraindications included active internal bleeding, recent (<3 months) stroke, neurosurgery or intracranial trauma, recent cardiopulmonary resuscitation, gastrointestinal bleed, major surgery or trauma and uncontrolled hypertension (SBP >180 mmHg) [9].
Conclusion(s)
Catheter-directed thrombolysis was selected in index patient because there was no discernible improvement with anticoagulation alone. It improved the prognosis of such a large DVT. Early intervention and prompt diagnosis are essential for these patients’ recovery. When used in conjunction with thrombolysis, the IVC filter helps to break up the clot lodged in the lower leg and prevents it from dislodging into the pulmonary veins. Thus, one can infer that intravenous thrombolysis yielded better results than the isolated use of anticoagulation in the management of large DVT.
[1]. Bajda J, Park AN, Raj A, Raj R, Gorantla VR, Inferior vena cava filters and complications: A systematic reviewCureus 2023 15(6):e4003810.7759/cureus.40038 [Google Scholar] [CrossRef]
[2]. Stone J, Hangge P, Albadawi H, Wallace A, Shamoun F, Knuttien MG, Deep vein thrombosis: Pathogenesis, diagnosis, and medical managementCardiovasc Diagn Ther 2017 7(Suppl 3):S27610.21037/cdt.2017.09.0129399531PMC5778510 [Google Scholar] [CrossRef] [PubMed]
[3]. Langford Nj, Stansby G, Avital L, The management of venous thromboembolic diseases and the role of thrombophilia testing: Summary of NICE Guideline CG144Acute Med 2012 11:138-42.10.52964/AMJA.0562 [Google Scholar] [CrossRef]
[4]. Chan NC, Weitz JI, Recent advances in understanding, diagnosing and treating venous thrombosisF1000Res 2020 9:F1000 Faculty Rev-120610.12688/f1000research.27115.133082930PMC7539078 [Google Scholar] [CrossRef] [PubMed]
[5]. Yamashita Y, Morimoto T, Kimura T, Venous thromboembolism: Recent advancement and future perspectiveJ Cardiol 2022 79(1):79-89.10.1016/j.jjcc.2021.08.02634518074 [Google Scholar] [CrossRef] [PubMed]
[6]. Konstantinides S, Torbicki A, Management of venous thrombo-embolism: An updateEur Heart J 2014 35:2855-63.10.1093/eurheartj/ehu24325179762 [Google Scholar] [CrossRef] [PubMed]
[7]. Fontyn S, Bai Y, Bolger S, Greco K, Wang TF, Hamm C, Inferior vena cava filter use at a large community hospital: A retrospective cohort studySci Rep 2024 14(1):1019210.1038/s41598-024-60868-z38702341PMC11068867 [Google Scholar] [CrossRef] [PubMed]
[8]. Goldhaber SZ, Magnuson EA, Chinnakondepalli KM, Cohen DJ, Vedantham S, Catheter-directed thrombolysis for deep vein thrombosis: 2021 updateVascular Medicine 2021 26(6):662-69.10.1177/1358863X21104293034606385PMC9009765 [Google Scholar] [CrossRef] [PubMed]
[9]. Hobohm L, Schmidt FP, Gori T, Schmidtmann I, Barco S, Münzel T, In-hospital outcomes of catheter-directed thrombolysis in patients with pulmonary embolismEur Heart J Acute Cardiovasc Care 2021 10(3):258-64.10.1093/ehjacc/zuaa02633620441 [Google Scholar] [CrossRef] [PubMed]