Blunt trauma to the abdomen is widely encountered in the Emergency Department (ED) among both children and adults. Trauma is a major contributor to morbidity and mortality, even in the paediatric population. However, post-traumatic rupture of the urinary bladder in children is a rare occurrence. Hereby, the authors present a case report of a seven-year-old male, who was a victim of a bike versus truck collision, was brought to the Emergency Department in a state of haemodynamic shock. Two out of the three passengers on the motorcycle succumbed to their injuries on the spot. The survivor was rushed to the ED by ambulance. Upon initial examination, the patient was in a state of haemodynamic shock, with abdominal tenderness, lower abdominal guarding, and left inguinal subcutaneous emphysema. Fluid resuscitation was initiated at 10 mL/kg of crystalloids through intravenous access. Insertion of a Foley catheter revealed frank haematuria without urine output, and a Contrast-enhanced Computed Tomography (CECT) scan of the abdomen and pelvis showed gross haemoperitoneum. The patient was taken for emergency exploratory laparotomy, as the suspicion of bladder rupture was high. The procedure revealed a 3×4 cm rent in the dome of the urinary bladder. The bladder was repaired with Polydioxanone Suture 2-0 sutures in two layers. An abdominal drain was placed in the pelvic cavity, and the abdomen was closed in layers. The patient was discharged after seven days with an indwelling Foley catheter. The Foley catheter was kept in place for 14 days, after which it was removed following a successful trial voiding. On subsequent follow-up, the patient had no urinary complaints and recovered well. The present case report is significant as it addresses the bladder rupture of a young child who was a victim of a road accident. It is evident that double-layer repair of the bladder rupture with absorbable sutures yields significant outcomes even in children.
Case Report
A seven-year-old male was brought to the Emergency Department by relatives with an alleged history of a bike versus truck road traffic accident, which was claimed to have happened an hour ago. Two out of the three passengers on the motorcycle succumbed to their injuries on the spot. The survivor was brought to the ED by an ambulance. The patient had sustained trauma to the head, chest, and abdomen as a consequence of the incident.
Upon arrival at the hospital, the patient was irritable, with inconsolable crying, and was in a state of haemodynamic shock. Post-trauma, there was no history of loss of consciousness, vomiting, dizziness, Ear Nose and Throat (ENT) bleeding, or seizures in the patient. The Glasgow Coma Scale (GCS) was E4V5M6 upon arrival. A general physical examination revealed tachycardia at 112 bpm, blood pressure of 92/58 mmHg, and adequate oxygen saturation of 96% on room air; the patient weighed 25.3 kilograms. Examination of the cardiovascular, respiratory, and nervous systems revealed normal findings. Intravenous access was obtained, and fluid resuscitation with crystalloids at 10 mL/kg was initiated.
Abdominal examination showed diffuse tenderness over all nine quadrants of the abdomen, with guarding and distension, along with a 4×3 cm contusion over the suprapubic region and left inguinal region. After assessing the vitals and commencing fluid resuscitation, Ryle’s tube and Foley catheter were inserted. Upon insertion of the Foley catheter, frank haematuria was noted in the urobag, which raised a suspicion of bladder injury.
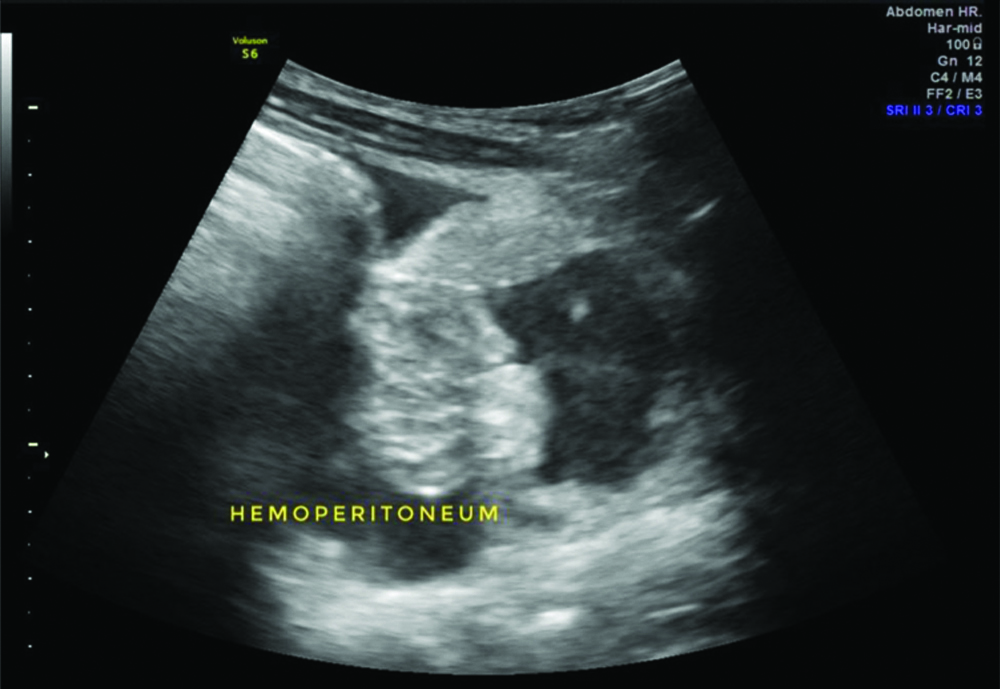
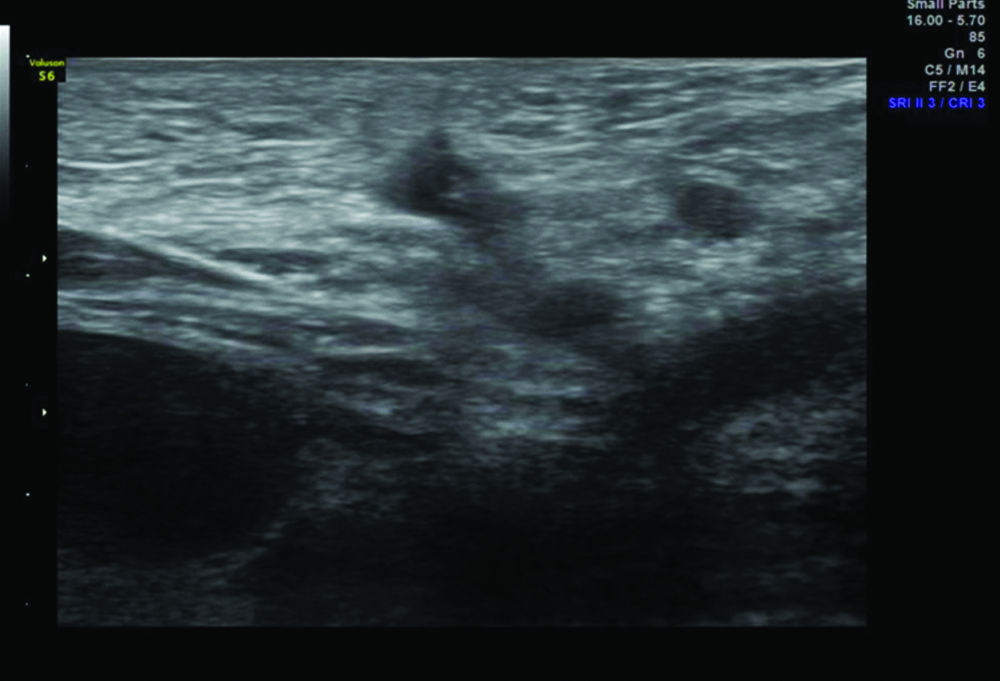
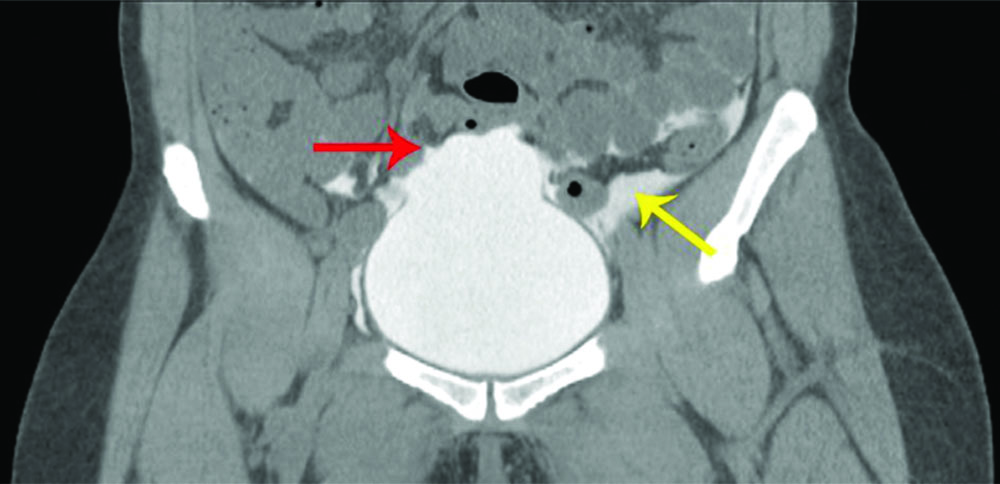
A routine haemogram showed a haemoglobin level of 8.4 gm% and a White Blood Cells (WBC) count of 23,300 cells per cubic millimeter. A Focused Assessment with Sonography in Trauma (FAST) scan was performed, which was suspicious for haemoperitoneum [Table/Fig-1]. Ultrasonography of the inguinal region revealed left inguinal subcutaneous emphysema [Table/Fig-2]. A CECT of the abdomen showed gross free fluid with internal echoes within the abdomen, suggestive of gross haemoperitoneum, along with subcutaneous emphysema in the left inguinal region [Table/Fig-3].
FAST scan suggestive of haemoperitoneum.
Ultrasonography of the left inguinal region suggestive of left inguinal subcutaneous emphysema.
Contrast-enhanced Computed Tomography (CECT) suggestive of Intraperitoneal (IP) bladder rupture (red arrow: rupture in the dome of the bladder with extravasation of contrast and yellow arrow: extravasated contrast material).
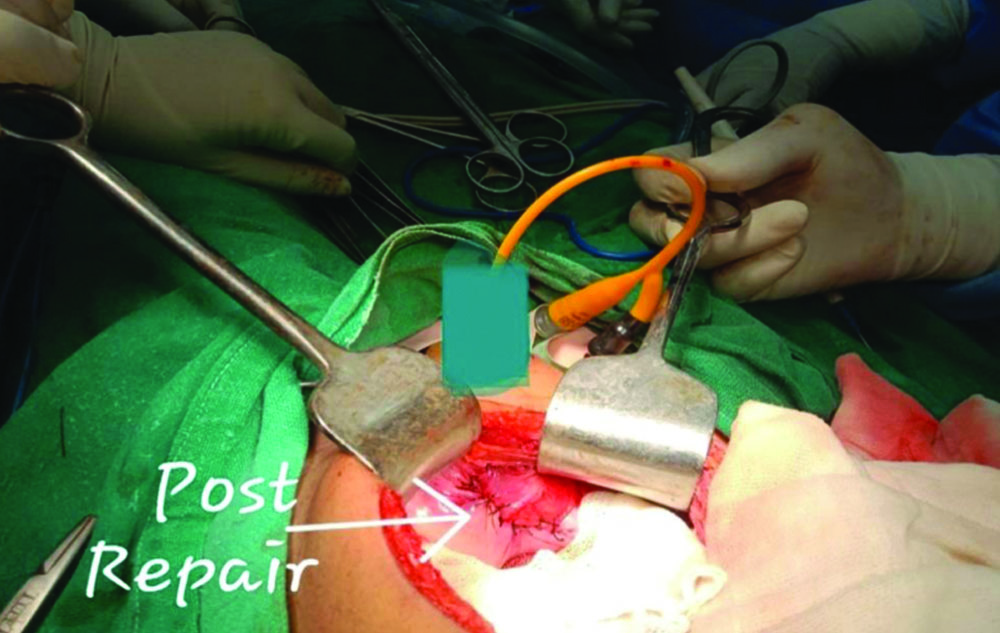
With the suspicion of a traumatic bladder injury, the decision was made to perform an exploratory laparotomy. A lower midline laparotomy incision was made, the abdomen was opened, and approximately 200 mL of frank blood with clots was noted in the peritoneal cavity. A 3×4 cm rent, vertically oval in shape, was observed on the dome of the bladder, suggestive of bladder rupture secondary to blunt trauma to the abdomen [Table/Fig-4]. The bladder was repaired in two layers using PDS 2-0 sutures [Table/Fig-5], and haemostasis was achieved [1]. An abdominal drain was placed in the pelvic cavity and secured with 1-0 silk sutures. The peritoneum was closed with Vicryl 2-0 sutures, the rectus muscle and anterior rectus were closed with Ethilon loop 1-0 sutures, followed by skin sutures with Ethilon 2-0.
Preoperative image showing the rent in the dome of the bladder.

Postoperative image after bladder repair.
Postoperatively, the patient received a blood transfusion, with the quantity adjusted according to body weight. The patient was mobilised on Postoperative Day (POD) 1. Due to the implementation of incentive spirometry, chest physiotherapy, and adequate wound management, the patient recovered without any complications during the postoperative period. The wound was inspected on POD 3 and POD 7, showing no signs of surgical site infection. The patient was discharged on POD 7 with an indwelling 10 Fr urethral catheter. The patient was followed-up in the Outpatient Department (OPD) on POD 10 and POD 14. As the wound showed no signs of surgical site infection, the skin sutures were removed on POD 10. The catheter was removed on POD 14, after which the patient was able to void the bladder normally.
Discussion
A careful analysis of the existing literature shows that less than 2% of all cases of blunt abdominal trauma present with bladder injury, and among them, almost 80% of cases are associated with pelvic fractures [2]. In most cases, a distended bladder is more commonly affected than a collapsed bladder. Gross haematuria is the hallmark sign of bladder injury, followed by abdominal distension due to urinary ascites, perineal haematoma, urine retention, and abdominal pain [2]. In a retrospective study conducted by Monstrey SJM et al., it was inferred that the anatomical and physiological differences in children make them more susceptible to urological trauma than adults [3].
Bladder injuries can be classified as bladder contusions, Intraperitoneal (IP) bladder rupture, and Extraperitoneal (EP) bladder rupture. Damage to the bladder mucosa or muscular layer without losing bladder wall continuity is seen in bladder contusions. Further, Cystography shows no extravasation and is generally treated conservatively. The IP bladder rupture occurs due to an abrupt rise in intravesical pressure, often secondary to blunt pelvic trauma. The dome of the bladder, being the weakest part, is frequently ruptured. Cystography shows extravasation of contrast with the outlining of visceral organs with dye. IP bladder rupture is seen in about 40% of cases of all bladder injuries. The EP bladder rupture is exclusive to pelvic ring fractures, where a bony spicule may lacerate the bladder near the bladder base and is almost always accompanied by disruption of the pelvic ring. Cystography shows extravasation of contrast confined to the perivesical soft tissues with urinary extravasation up to the thigh or scrotum. EP bladder ruptures account for about 60% of cases of bladder injuries. Combined intra- and extraperitoneal injuries are rare and are often diagnosed intraoperatively [4].
Unlike in adults, a child’s bladder is more intraperitoneal, making it more susceptible to rupture, especially when it is full [5]. In about 95% of all cases of bladder injury, gross haematuria is the most classical feature, whereas microscopic haematuria is seen in about 5% of cases [6]. According to the American Association for the Surgery of Trauma bladder injury scoring scale, urinary bladder trauma can be graded as follows: Grade I- contusions, haematoma, or partial thickness laceration of the bladder; Grade II- extraperitoneal bladder wall laceration less than 2 cm; Grade III- extraperitoneal lacerations more than 2 cm or intraperitoneal lacerations less than 2 cm; Grade IV- intraperitoneal lacerations of more than 2 cm; Grade V- intraperitoneal or extraperitoneal lacerations extending to the bladder neck or trigone [7].
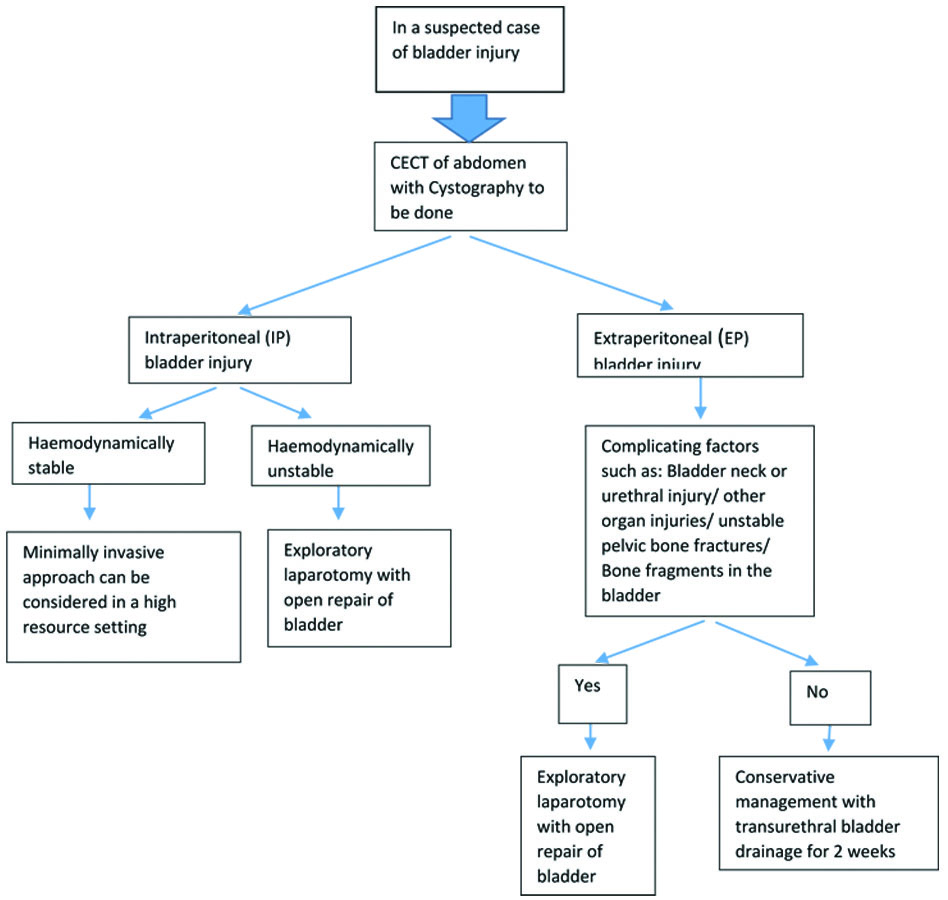
Contusions and interstitial bladder injuries are managed conservatively with prolonged bladder rest and a urethral catheter for about 7-14 days. Intraperitoneal bladder rupture significantly increases the risk of urinary ascites and sepsis, necessitating urgent surgical repair [7]. After the repair, a dye is injected into the bladder through a Foley catheter to confirm that there is no urinary leakage, and the abdomen is closed after placing an abdominal drain into the pelvic cavity. A urethral catheter is kept in place for about 7-14 days to provide adequate rest to the bladder and different treatment approaches for bladder trauma are depicted in [Table/Fig-6] [3]. A similar technique was followed in present case, where the bladder rent was repaired in two layers, followed by pelvic drain insertion. A 10 Fr Foley catheter was left in-situ for 14 days, after which the catheter was removed.
Treatment approaches for suspected bladder trauma [3].
Extraperitoneal bladder rupture is usually treated conservatively with a urethral catheter, and most extraperitoneal bladder ruptures heal within three weeks. However, surgical repair is indicated in bladder injuries that do not heal even after four weeks of catheterisation, as verified by an X-ray cystogram showing extravasation of contrast [8]. In a multi-institutional cohort study conducted by Anderson RE et al., 43% of the study group with extraperitoneal bladder injury underwent operative management, whereas 57% underwent conservative management. It was inferred that there was no significant difference in the outcomes between operative and conservative management [9].
With groundbreaking developments in the field of minimal access surgery, laparoscopic bladder repair is also being performed. However, in a trauma setting, laparoscopy is contraindicated due to free fluid in the abdomen, extraperitoneal bleeding, and other visceral organ injuries that hinder vision and pose challenges during surgery [10].
Conclusion(s)
Isolated bladder trauma in the paediatric age group is a rare incidence associated with blunt abdominal trauma, occurring in less than 2% of all cases. IP bladder rupture is a surgical emergency that necessitates bladder repair. However, EP bladder rupture can often be managed conservatively. In present case, a Grade IV IP bladder rupture was encountered, and the bladder was repaired using a two-layer technique. An indwelling urethral catheter was placed for 14 days. The patient was discharged on POD 7. He was subsequently reviewed in the OPD on POD 10 for suture removal and on POD 14 for catheter removal. Upon follow-up, the patient recovered well without any urinary complaints, emphasising that, although paediatric bladder rupture is rare, the surgical principles of IP bladder rupture repair are essentially standard in both paediatric and adult bladder trauma.
[1]. Zelivianskaia AS, Bradley SE, Morozov VV, Best practices for repair of iatrogenic bladder injuryAJOG Glob Rep 2022 2(3):10006210.1016/j.xagr.2022.10006236276798PMC9563547 [Google Scholar] [CrossRef] [PubMed]
[2]. Jain U, Kumar D, Sreedhar Qazi IA, Rasool M, Laparoscopic repair of traumatic intraperitoneal bladder rupture: A rare case reportInt J Res Med Sci 2023 11:2307-9.10.18203/2320-6012.ijrms20231662 [Google Scholar] [CrossRef]
[3]. Monstrey SJM, Staak FHJ vander, Werken C vander, Debruyne FMH, Severijnen RSVM, Goris RJA, Urinary tract injuries in children: Are they different from adults?Z Für Kinderchir 2008 43:31-34.10.1055/s-2008-10434083376587 [Google Scholar] [CrossRef] [PubMed]
[4]. Gomez RG, Ceballos L, Coburn M, Corriere Jr JN, Dixon CM, Lobel B, Consensus statement on bladder injuriesBJU Int 2004 94(1):27-32.10.1111/j.1464-410X.2004.04896.x15217426 [Google Scholar] [CrossRef] [PubMed]
[5]. Reddy D, Laher A, Moeng M, Adam A, Bladder trauma: A guideline of the guidelinesBJU Int 2023 :13310.1111/bju.1623638009413 [Google Scholar] [CrossRef] [PubMed]
[6]. Mahat Y, Leong J, Chung P, A contemporary review of adult bladder traumaJ Inj Violence Res 2019 11:101-06.10.5249/jivr.v11i2.1069 [Google Scholar] [CrossRef]
[7]. The American Association for the Surgery of Trauma [Internet] 2009 [cited 2024 May 20]. Injury Scoring Scale. Available from: https://www.aast.org/resources-detail/injury-scoring-scale [Google Scholar]
[8]. Bakal U, Sarac M, Tartar T, Ersoz F, Kazez A, Bladder perforations in childrenNiger J Clin Pract 2015 18(4):483-88.10.4103/1119-3077.15175225966719 [Google Scholar] [CrossRef] [PubMed]
[9]. Anderson RE, Keihani S, Moses RA, Nocera AP, Selph JP, Becerra CMC, Current management of extraperitoneal bladder injuries: Results from the Multi-Institutional Genito-Urinary Trauma Study (MiGUTS)J Urol [Internet] 2020 [cited 2024 Sep 13]; Available from: https://www.auajournals.org/doi/10.1097/JU.0000000000001075 [Google Scholar]
[10]. Karadağ Ç, Tander B, Erginel B, Demirel D, Bicakci U, Gunaydin M, Laparoscopic repair in children with traumatic bladder perforationJ Minimal Access Surg 2016 12(3):292-94.10.4103/0972-9941.16997327279407PMC4916762 [Google Scholar] [CrossRef] [PubMed]