With the introduction of general anaesthesia, it is possible to induce patient in a regulated unconscious state, rendering them insensitive to pain and unaware of the surgical proceedings taking place [1]. General anaesthesia is most commonly achieved via combination of induction agents, intravenous sedatives and analgesics followed by maintenance with volatile anaesthetics [2,3].
Laryngoscopy and endotracheal intubation can trigger a broad array of stress responses or pressure response, including tachycardia, hypertension, bronchospasm, elevated intraocular pressure, increased intracranial pressure and arrythmias, myocardial ischaemia [4]. The haemodynamic response begins within 5 seconds of direct laryngoscopy and further increases with the passage of the endotracheal tube. It reaches its highest point within 1-2 minutes, and returns to normal levels by 5 minutes [4]. These changes are brief and well tolerated in healthy individuals, but patients with cardiovascular compromise or cerebrovascular disease may experience adverse complications such as arrythmias, cardiac arrest or cerebrovascular accidents [5].
Various agents like lignocaine, opioids, nitroglycerine, calcium channel blockers such as diltiazem and β-blockers such as esmolol have been used to obtund these stress responses [1]. Dexmedetomidine, a highly selective, short-acting, alpha-2-adrenoreceptor agonist, has anxiolytic analgesic and sedative property without inducing respiratory depression. It is a preferred choice for alleviating anxiety or nervousness prior to anaesthesia. [6] Dexmetomidine is now widely being used as it minimises the perioperative requirement of sedatives and analgesics, while stabilising intraoperative haemodynamics [7].
Dexmedetomidine suppresses noradrenaline release and induces hypnosis and sedation by acting on presynaptic central α2 receptors in the locus coeruleus. Activation of α2 receptors in the post synaptic region results in reduced sympathetic activity, which manifests as bradycardia and hypotension [8].
Intravenous dexmedetomidine in larger doses can cause detrimental haemodynamic complications like bradycardia hypotension, and even cardiac arrest, which mandates proper dosage in intravenous dexmedetomidine. Moreover, rapid intravenous dexmedetomidine infusion may also cause unfavourable biphasic changes in mean arterial pressure. Other administration routes like intranasal, intramuscular or oral are also effective and may mitigate the adverse effects seen with intravenous route [3].
The intramuscular route is more convenient and efficient than others as it has shown to have uniform and slow absorption of drug, reaches the systemic circulation quickly bypassing the first-pass metabolism of liver [9]. Also the peak concentration is significantly slower in intramuscular route than intravenous. This not only prolongs the drug onset time but also leads to a less prominent maximum effect of dexmedetomidine, therefore bradycardia and hypotension are not much marked via intramuscular as seen in intravenous route. The bioavailability dexmedetomidine via intramuscular route is 104% and time to peak concentration is approximately 1.6-1.7 hours [10].
This research work bridges a critical gap of lack in the current literature. None of the studies on author’s extensive literature search revealed direct comparison of same dose of dexmedetomidine via intramuscular and intravenous for blunting pressure response to laryngoscopy and intubation. This research work bridges this critical gap in the current literature. Hence, in present study, primary objective was to compare efficacy of intramuscular dexmedetomidine with intravenous dexmedetomidine as premedication for on heart rate, systolic blood pressure, diastolic blood pressure, and Mean Arterial Pressure (MAP) following laryngoscopy and tracheal intubation. The secondary objective was to compare the adverse effects like sedation, desaturation encountered with the above two routes of administration. It was hypothesised that intramuscular route of dexmedetomidine would provide superior hemodynamic stability compared to intravenous administration in dampening the hemodynamic response to laryngoscopy and intubation.
Materials and Methods
The present prospective randomised clinical study was conducted in Department of Anaesthesia, Shrimati Bhikhiben Kanjibhai Shah Medical Institute and Research Centre (SBKS MIRC) in Piparia, Vadodara, Gujarat, India over a period of six months from January 2024 to June 2024. It was approved by the Institutional Ethical Committee (SVIEC/MEDI/SRP/JUNE/23/79). The present study was conducted in accordance with Institutional Ethics Committee standards and the Helsinki declaration. Written informed consent was obtained from all eligible patients. No names or initials were used.
Sample size calculation: Following a pilot study involving 10 patients (5 in each group), the sample size was calculated using Process Automation Software System (PASS) 15 (NVSS-National Vital Statistics System). From data from pilot study, considering the mean heart rate during laryngoscopy 88.5±9.42 beats/minute of group DIM and 94.06±11.9 beats/minute of group DIV, power 80% and level of significance 0.05 and type I error (α) of 0.05, sample size was calculated as 64; n DIM=32, n DIV=32.
Inclusion criteria: Adults patients aged 18-60 years belonging to grade I and II of American Society of Anaesthesiologists (ASA) classification who underwent elective surgeries under general anaesthesia with endotracheal intubation were included in the study.
Exclusion criteria: Patients below 18 years or above 65 years, those refusing to participate, those with ASA III or higher, hepatic, renal, cardiac, respiratory or cerebral co-morbidities, Body Mass Index (BMI) ≥30 kg/m2 (as these patients are anticipated for difficult airway) or a history of snoring and obstructive sleep apnoea were excluded from the study. Patients in whom laryngoscopy and intubation duration was prolonged (>3 minutes), multiple attempts were required were also excluded.
Study Procedure
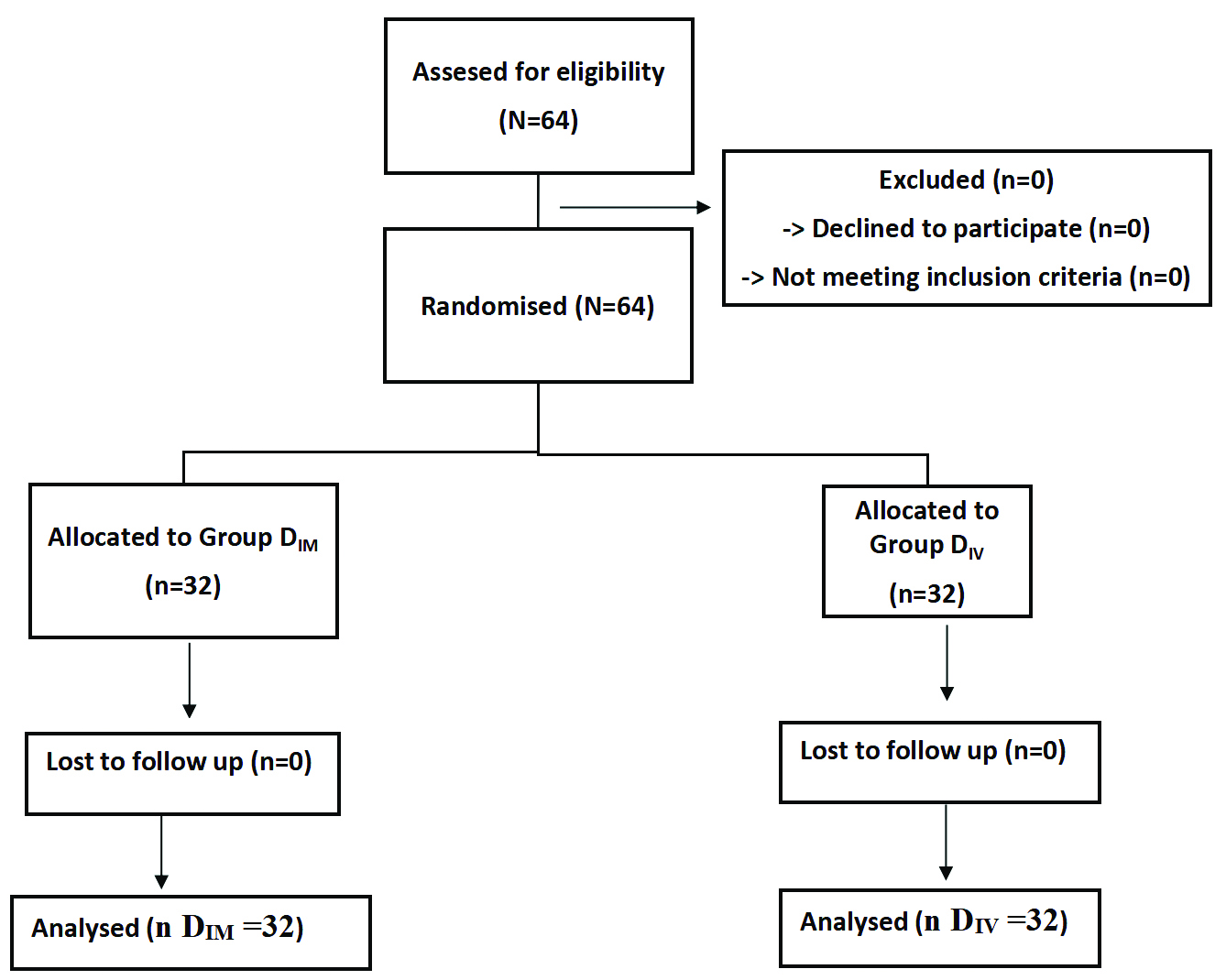
It was a parallel group design study, in which 64 patients were randomised into 2 groups of 32 patients each with the help of computer-generated randomisation in MS Excel and concealment was done using sealed opaque envelope method.
The sealed envelope was opened by a preoperative room staff nurse who was not otherwise participating in the trial. Patients were counselled and after signing consent, monitors were applied in well-equipped pre-operative room (crash cart trolley readily available). Intravenous access was taken. The test drug was administered according to assigned route. Dosage of intravenous and intramuscular dexmedetomidine were derived from study done by Singla, A. et al., [11] and Sun Y et al., [12] where they used 1 μg/kg intravenous and 1 μg/kg intramuscular dexmedetomidine respectively and found them effective dose and route for pressure response blunting during laryngoscopy and intubation.
Group DIM (Intramuscular Dexmedetomidine) received intramuscular Inj. Dexmedetomidine 1 μg/kg 45 minutes prior to induction Group DIV (intravenous Dexmedetomidine) received intravenous Inj. Dexmedetomidine 1 μg/kg as an infusion in 100 mL NS over 10 minutes 45 minutes prior to induction. The consultant anaesthesiologist who was conducting the cases, monitoring and observing the values was not aware of the administration route. In the operating room, all ASA standard monitors were connected to the patients and their vitals were noted. Preoxygenation with 100% oxygen via a face mask was given for three minutes. Standard general anaesthesia was administered by the consultant Anaesthesiologist using propofol 1.5-2 mg/kg intravenously, supplemented with intravenous succinylcholine 2 mg/kg to aid in endotracheal intubation.
Following tracheal intubation, the patient was put on mechanical ventilation on volume control mode using with ventilatory settings of a tidal volume of 6-8 mL/kg and a respiratory rate of 12-14/min to maintain an End-tidal Carbon Dioxide (etCO2) level between 30-35 mmHg with a 1:1 mixture of nitrous oxide and oxygen at total flow of 2 litres per min, along with isoflurane maintaining minimum alveolar concentration of 1. Muscle relaxation was achieved through an initial loading dose of inj. Atracurium (0.5 mg/kg) followed by a maintenance dose of (0.1 mg/kg). Notably, opioids were not administered during the entire procedure.
Heart rate, systolic blood pressure, diastolic blood pressure and oxygen saturation were recorded at specific time points: before induction, immediately after induction, during laryngoscopy and tracheal intubation and at 1, 3, 5, and 7 minutes following intubation.
Inj. Ondansetron 0.1 mg/kg was given 15 mins before completion of surgery. As the surgery ended, after ensuring that the patient’s breathing was normal with sufficient tidal volume and respiratory rate the effects of anaesthesia were reversed by giving glycopyrrolate (0.008 mg/kg) and neostigmine (0.05 mg/kg) intravenously. Following this, the endotracheal tube was removed and patients were observed for any complications such as nausea, vomiting, low blood pressure. Episodes of hypotension (MAP <20% of baseline) [6], bradycardia (HR <50/min) [6] and hypoxia (SPO2 <90%) [6] within the study period were noted and treated accordingly. Sedation status in both groups, were assessed using the Ramsay Sedation Scale (RSS) [13] at extubation. The Consolidated Standards of Reporting Trials (CONSORT) flow diagram is given in [Table/Fig-1].
Statistical Analysis
The sample size of 64 patients in which 32 patients were present in each group was determined using MedCalc 12.5 software. Data was collected and then tabulated for assessment. Numerical variables (continuous parametric data) were presented as mean and Standard Deviation (SD). Categorical data were presented as the number of patients. On assessment, data was normally distributed, Shapiro-Wilk test was used to assess normality. MedCalc statistical software version 12.5 was used for comparisons between groups. Unpaired student’s t-test was used for numerical variables. For categorical variables, the Chi-square test was employed. In this study Bonferroni correction was applied to account for multiple comparisons, adjusting the significance level to reduce the likelihood of type I errors. A p-value of less than 0.05 was considered statistically significant, while a p-value less than 0.001 was regarded as highly significant.
Results
All 64 patients selected initially for the study were able to complete the study without any dropouts. Patients in both the groups were similar in terms of age (in years), weight (in kilograms), gender, ASA status and duration of surgery (in minutes) (p>0.05) [Table/Fig-2].
| Parameters | Group DIM | Group DIV | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Age (years) | 37.84±12.85 | 40.41±9.82 | 0.3722 |
| Weight (kg) | 64.69±9.71 | 64.09±10.29 | 0.8112 |
| Duration of surgery (minutes) | 190.3±17.3 | 192.5±17.3 | 0.8 |
| n (%) | n (%) |
| Gender |
| Male | 19 (59.38%) | 18 (56.25%) | 1.0000 |
| Female | 13 (40.63%) | 14 (43.75%) |
| ASA |
| I | 17 (53.13%) | 20 (62.5%) | 0.6127 |
| II | 15 (46.88%) | 12 (37.5%) |
Unpaired student’s t-test and chi-square test were used as statistical test; p-value ≤0.05 statistically significant
Baseline haemodynamic variables like HR, SBP, DBP, MAP and SpO2 were comparable in both the groups at baseline (p>0.05) [Table/Fig-3,4,5 and 6].
Comparison of mean Heart Rate (HR) in beats/minute in both the groups at different time intervals.
| Time | Group DIM | Group DIV | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 83.88±6.94 | 86.44±14.14 | 0.3615 |
| After test drug | 81.38±6.89 | 83.19±13.27 | 0.4960 |
| After induction | 80.19±7.55 | 84.78±11.11 | 0.0578 |
| At laryngoscopy and intubation | 88.5±9.42 | 94.06±11.9 | 0.0424 |
| 1 min | 86.63±10.18 | 92.19±11.39 | 0.0437 |
| 3 min | 84.63±9.64 | 89.88±11.17 | 0.0485 |
| 5 min | 81.66±8.93 | 86.84±11.2 | 0.0450 |
| 7 min | 78.56±8.79 | 83.81±9.65 | 0.0264 |
Unpaired student t-test was used as statistical test; p-value ≤0.05 statistically significant
Comparison of Mean SBP in mmHg in both the groups at different time intervals.
| Time | Group DIM | Group DIV | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 123.34±5.84 | 126.63±9.82 | 0.1084 |
| After test drug | 117.06±5.43 | 120.38±9.21 | 0.0839 |
| After induction | 117.16±4.98 | 121.22±10.6 | 0.0544 |
| At laryngoscopy and intubation | 132.56±5.74 | 137.13±9.54 | 0.0235 |
| 1 min | 125.94±7.83 | 130.31±6.15 | 0.0158 |
| 3 min | 121.06±11.19 | 125.75±5.67 | 0.0385 |
| 5 min | 115.97±10.41 | 123.09±5.78 | 0.0012 |
| 7 min | 114.06±10.51 | 119.03±4.13 | 0.0656 |
Unpaired student t-test was used as statistical test; p-value ≤0.05 statistically significant
Comparison of mean diastolic blood pressure in mmHg in both the groups at different time intervals.
| Time | Group DIM | Group DIV | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 82.38±5.67 | 85.06±5.48 | 0.0585 |
| After test drug | 79.06±8.13 | 82.41±5.31 | 0.0555 |
| After induction | 79.91±8.59 | 80.44±5.75 | 0.7728 |
| At laryngoscopy and intubation | 91.03±9.21 | 98.31±5.9 | 0.0004 |
| 1 min | 85.03±6.56 | 96.28±5.84 | p<0.0001 |
| 3 min | 79.09±8.66 | 93.25±6.05 | p<0.0001 |
| 5 min | 76.41±8.45 | 90.75±6.06 | p<0.0001 |
| 7 min | 73.41±8.04 | 87.81±6.18 | p<0.0001 |
Unpaired student t-test was used as statistical test; p-value ≤0.05 statistically significant
Comparison of mean arterial pressure in mmHg in both the groups at different time intervals.
| Time | Group DIM | Group DIV | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 88.13±12.72 | 98.41±5.7 | 0.0641 |
| After test drug | 88.69±13.79 | 94.16±5.66 | 0.0421 |
| After induction | 90.16±13.07 | 91.44±5.74 | 0.6138 |
| At laryngoscopy and intubation | 101.28±15 | 110.44±6.01 | 0.0021 |
| 1 min | 93.63±13.44 | 107.97±5.91 | p<0.0001 |
| 3 min | 87.97±12.99 | 104.44±5.9 | p<0.0001 |
| 5 min | 84.81±12.31 | 101.88±5.97 | p<0.0001 |
| 7min | 80.88±12.37 | 98.56±6.16 | p<0.0001 |
Unpaired student t-test was used as statistical test; p-value ≤0.05 statistically significant
A transient yet statistically significant elevation in HR, SBP, DBP and MAP occurred during laryngoscopy and intubation in both groups, with Group DIV exhibiting a more accentuated hypertensive response compared to Group DIM (p-value=0.04, 0.02, 0.004 and 0.0021, respectively). Following intubation, a gradual attenuation of the stress response was observed in both groups. Group DIM demonstrated a pronounced reduction in HR, SBP and DBP compared to Group DIV at 1, 3, and 5 minutes post-intubation, indicative of improved hemodynamic stability. Subsequently, after intubation there was significant difference in all the parameters between the two groups throughout (p<0.05) till 7 minutes [Table/Fig-3,4,5 and 6].
One patient had an episode of significant hypertension and tachycardia (BP=160/100 mm of Hg, HR=130/min) after starting of infusion of intravenous dexmedetomidine infusion which settled down after 5 mins and then haemodynamics were same as other patients of DIV group. The increase of all the haemodynamic parameters from laryngoscopy and intubation returned to baseline values around 3 minutes in DIM group while in the DIV group at around 7 minutes and thereafter remained comparable throughout. Post-intubation, the heart rate, SBP, DBP and MAP percentage reduction from baseline was more pronounced in DIM (6.34%, 7.52%, 10.88% and 8.22%, respectively) in comparison to DIV which exhibited a 3.04%, 6% decrease in heart rate, SBP and 3.23% increase in DBP while MAP reached the baseline values. [Table/Fig-7] SpO2 was comparable between the groups at all time points [Table/Fig-8].
Comparison of percentage fall from baseline of HR, SBP and DBP post intubation at 7 minutes.
| Parameters | Group DIM | Group DIV |
|---|
| Heart rate | 6.34% | 3.04% |
| SBP | 7.52% | 6.00% |
| DBP | 10.88% | 3.23% |
| MAP | 8.22% | 0% |
Comparison of oxygen saturation in % in both the groups at different time intervals.
| Time | Group DIM | Group DIV | t | p-value |
|---|
| Mean±SD | Mean±SD |
|---|
| Baseline | 100±0 | 100±0 | NA | NA |
| After test drug | 100±0 | 100±0 | NA | NA |
| At induction | 100±0 | 99.97±0.18 | NA | NA |
| At laryngoscopy and intubation | 99.94±0.25 | 99.94±0.25 | 0.0000 | 1.0000 |
| 1 min | 99.97±0.18 | 99.94±0.25 | -0.5510 | 0.5837 |
| 3 min | 100±0 | 100±0 | NA | NA |
| 5 min | 99.97±0.18 | 99.94±0.25 | -0.5510 | 0.5837 |
| 7 min | 99.97±0.18 | 99.97±0.18 | 0.0000 | 1.0000 |
Unpaired student’s t-test was used as statistical test; p-value ≤0.05 statistically significant
There was no significant postoperative sedation at extubation [Table/Fig-9]. Neither did any of the patient experience any adverse side effects including nausea and vomiting, hypotension [Table/Fig-7], Bradycardia [Table/Fig-3] and desaturation [Table/Fig-9] in both the groups.
Comparison of Sedation scores at extubation.
| Ramsay sedation score | Group DIM | Group DIV | p-value |
|---|
| n (%) | n (%) |
|---|
| 2 | 17 (53.13%) | 12 (37.5%) | 0.3152 |
| 3 | 15 (46.88%) | 20 (62.5%) |
Discussion
In present prospective randomised clinical study, haemodynamic responses following laryngoscopy and tracheal intubation were more favourable with intramuscular dexmedetomidine which resulted in a greater decrease in HR, SBP, DBP and MAP, both during and after laryngoscopy and intubation compared to intravenous dexmedetomidine. The sedation score was comparable in both groups along with no significant difference in incidence of adverse effects like nausea and vomiting, hypotension, bradycardia and desaturation in both the groups.
Baseline haemodynamic parameters and patient demographic profiles (age, weight and gender) between Group DIM and DIV were comparable, suggesting successful randomisation to create homogeneous groups. This allowed identification of the effect of route of administration of dexmedetomidine on haemodynamic responses and thus improved strength and internal validation of the study.
Patients in both groups were comparable in terms of ASA grading and duration of surgery. As baseline health conditions can significantly influence haemodynamic response to laryngoscopy and tracheal intubation, comparable patients in both groups ruled out differences in haemodynamic responses during airway manipulation attributable to other causes than the mode of dexmedetomidine administration.
In current study, during the stress response from laryngoscopy, HR transiently increased in both groups, increase was more in Group DIV (8.86%) as compared to Group DIM (5.60%) from baseline. Furthermore, after intubation, a gradual decline in HR was observed in both groups, with Group DIM exhibiting a more pronounced decline at 7 min (6.34%) compared to Group DIV (3.04%). In contrast, Singla A et al., compared intravenous dexmedetomidine vs nebulised dexmedetomidine and observed no significant difference in HR in two groups at 0, 5, 10 minutes after induction, but significant decrease at 15 minutes in intravenous dexmedetomidine group [11]. While Niyogi S et al., who did similar comparison found no significant difference in HR in intravenous and intranasal dexmedetomidine groups at any time interval [6].
On comparing blood pressures (SBP, DBP and MAP) changes during laryngoscopy and intubation, in present study, there was significant increase in DIV group as compared to DIM. Post-intubation SBP, DBP and MAP gradually decreased in both groups, but the decrease in group DIM was significant as compared to DIV at 1, 3 and 5 minutes post intubation. Intergroup comparison at seven minutes revealed that DIM led to a more pronounced decrease in SBP, DBP and MAP from baseline (7.52%, 10.88%, 8.22%, respectively) whereas DIV resulted in 6.00% decrease in SBP, 3.23% increase in DBP while MAP returned to baseline value. This guarded haemodynamic control in DIM group was favourable for intraoperative anaesthetic and surgical requirements. On contrary, Singla, A et al., in their study found delayed but significant difference in SBP at 20 minutes in post-induction period and concluded that intravenous dexmedetomidine exerts profound hypotensive effect than nebulised administration [11]. Also, Niyogi S et al., and Gandhi M et al., found that in the intravenous group, BP was slightly lower than the nebulisation group at all time intervals and concluded that nebulised dexmedetomidine was more effective than intravenous dexmedetomidine [6,14].
In current study, sedation score of patients at extubation and incidences of adverse effects like nausea, vomiting, bradycardia and hypotension were comparable in both groups. In contrast, Niyogi S et al., Singla A et al., observed higher sedation in intravenous group but they had observed sedation before induction while in this study sedation was observed at extubation [6,11]. Gandhi M et al., also found insignificant difference in intravenous and intranasal groups [14]. Sun Y et al., also found no significant side-effects with intramuscular dexmedetomidine [12].
Patel N et al., conducted a study where they compared intramuscular dexmedetomidine 2.5 μg/kg vs intramuscular dexmedetomidine 2.5 μg/kg along with intravenous fentanyl 1.5 μg/kg [15]. They concluded that intramuscular dexmedetomidine on its own demonstrates effectiveness as a premedication agent for blunting the stress response, showing around 8% decrease in HR which was in coherence to present study. While their study employed a higher dosage of 2.5 μg/kg, in current study, authors found that even a lower dose of 1 μg/kg of intramuscular dexmedetomidine achieved comparable attenuation of haemodynamic responses.
In another study, Sun Y et al., compared intramuscular Inj. dexmedetomidine (1 μg/kg) with intramuscular Inj. midazolam (0.02 mg/kg) in premedication for preoperative sedation and augmentation of the effects of anaesthesia [12]. They observed that HR response after tracheal intubation and extubation, as well as the MAP response after extubation were reduced in the dexmedetomidine group compared to the midazolam group.
Indira P et al., and Shin HW et al., in two separate double-blinded randomised controlled study found that Dexmedetomidine 1 μg/kg intravenously effectively blunts pressure response during carbon dioxide insuffulation in laparoscopic cholecystectomy and laryngoscopy-intubation respectively [16,17]. They observed intravenous dexmedetomidine decreased HR from baseline by 6%, SBP by 6%, and DBP by 10%. Authors of current study had similar observations in terms of HR and SBP but DBP showed 3.23% increase rather than decrease. They concluded that dexmedetomidine effectively dampened the sympathoadrenal response and ensured stability in perioperative haemodynamics. Likewise, Kaya F et al., studied different doses of intravenous dexmedetomidine: 0.5 μg/kg vs 1 μg/kg vs placebo [18]. They concluded that dexmedetomidine effectively reduced the stress response to endotracheal intubation in a dose-dependent manner.
Many studies have proven efficacy of intravenous dexmedetomidine in blunting pressor response to laryngoscopy and intubation [16-21]. But it is associated with a biphasic response if, given as fast infusion [6]. This response was also observed by Singla A et al., and Kaya F et al., [11,18]. In adherence to their observations, in present study, authors also observed a biphasic blood pressure response with a bolus intravenous dose in a young 22-year-old patient, who had an episode of significant hypertension and tachycardia (BP=160/100 mm of Hg, HR=130/min) after starting of infusion of intravenous dexmedetomidine infusion which settled down after five minutes. Possible reason for such response may be accidental fast infusion of dexmedetomidine leading to biphasic response in form of hypertension for short duration along with transient tachycardia followed by hypotension and bradycardia. Such response is undesirable in anaesthesia. This response is caused by the activation of α2B receptors in vascular smooth muscles, which causes vasoconstriction and systemic and pulmonary hypertension. Later activation of central α2 adrenoceptors prevent the release of norepinephrine, thereby causing bradycardia leading to a decrease in serum norepinephrine levels by stimulating receptors in the medullary vasomotor centre (locus coeruleus) [22].
To minimise such adverse effects, alternative routes of dexmedetomidine administration have been explored. One such less explored route is intramuscular route. It offers a pharmacokinetic advantage over intravenous route, providing a more gradual absorption profile, reduced risk of dose-related toxicity, and diminished incidence of adverse effects. Furthermore, intramuscular delivery enhances bioavailability optimising therapeutic efficacy. Dexmedetomidine exhibits exceptional bioavailability of 104% when administered via the intramuscular route, with peak plasma concentrations reached in approximately 1.6 to 1.7 hours [10]. Also, this route is a preferred in specific cases like difficult venous access or emergency situations where intravenous access is difficult to achieve.
None of the previous studies have directly compared same dose of dexmedetomidine via intramuscular and intravenous routes for blunting pressure response to laryngoscopy and intubation. Thus, present study provides valuable insights on safety and efficacy of intramuscular dexmedetomidine in achieving optimal intraoperative haemodynamics. Findings of present study opens horizon for future research on larger-scale in diverse clinical settings and patients to confirm and generalise the results on safety and efficacy of intramuscular dexmedetomidine.
Limitation(s)
Major limitation of present study is that it could not be double blinded as patients knew their drug administration routes. Since, this is a hospital-based study, it has limited generalisability, it necessitates further investigation through larger and more extensive Randomised Controlled Trails (RCTs). The present study monitored hemodynamic changes up to only 7 minutes after intubation so effect of dexmedetomidine via different routes on intraoperatively hemodynamic parameters were not considered. Also, present study was conducted on ASA I and II so its effectiveness and usefulness needs be tested in ASA III and IV patients in further studies.
Conclusion(s)
The hemodynamic responses following laryngoscopy and tracheal intubation were more favourable with intramuscular dexmedetomidine compared to intravenously administered dexmedetomidine. Intramuscular administration of dexmedetomidine resulted in a better control of heart rate, SBP, DBP and MAP, both at and after laryngoscopy and intubation, when compared to the intravenous route with no significant adverse effects like sedation, hypotension, and bradycardia. The present study concludes that at an equal dose of 1 μg/kg, intramuscular dexmedetomidine is superior to intravenous dexmedetomidine in obtunding and maintaining hemodynamic stability following laryngoscopy and tracheal intubation, thus accepting the study hypothesis.
Unpaired student’s t-test and chi-square test were used as statistical test; p-value ≤0.05 statistically significant
Unpaired student t-test was used as statistical test; p-value ≤0.05 statistically significant
Unpaired student t-test was used as statistical test; p-value ≤0.05 statistically significant
Unpaired student t-test was used as statistical test; p-value ≤0.05 statistically significant
Unpaired student t-test was used as statistical test; p-value ≤0.05 statistically significant
Unpaired student’s t-test was used as statistical test; p-value ≤0.05 statistically significant