Case Report
Hereby the authors report a case of a 38-year-old male who was involved in a high-velocity Road Traffic Accident (RTA) four hours ago causing a floating knee injury to the right lower limb. Upon arrival at the nearest trauma centre, the patient was stabilised following the Advanced Trauma Life Support (ATLS) guidelines. Initial assessment revealed that the patient had an e-fast positive due to blunt trauma to the abdomen. X-rays were conducted for further assessment, showing a proximal humerus 3-part fracture, a comminuted distal femur intercondylar fracture and a comminuted proximal tibia-fibula comminuted fracture. The patient had no history of co-morbidities.
Primary stabilisation was done according to the Damage Control Orthopaedics (DCO) protocol, using an external fixator. Due to personal reasons, the patient was discharged and advised to keep regular follow-ups while the plan ahead was considered. The patient was lost for follow-up and arrived at the hospital after three months with the external fixator in-situ in the right lower limb, developing a knee joint flexion deformity of the knee joint along with external rotation of the floating knee segment to 90 degrees [Table/Fig-1].
Plain radiograph of the right tibia- anteroposterior and lateral view.
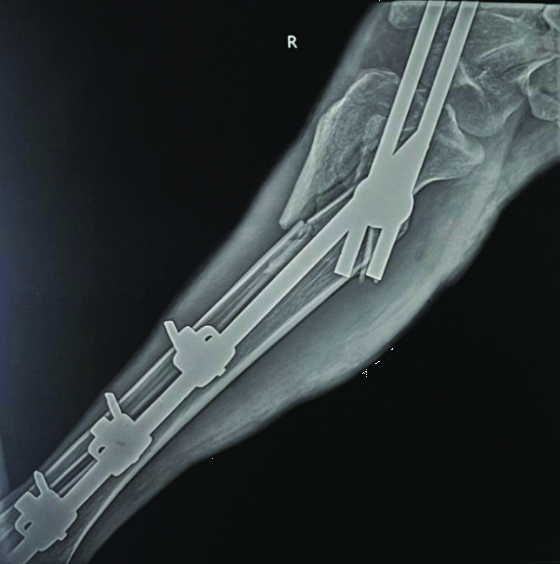
Patient at this phase clinically and radiologically was showing features of malunion, an externally rotated knee, poor nutrition, quadriceps atrophy and a poor skin condition, with right lower limb shortening of 2 cm as compared to normal limb. Initial step was removal of the previously applied external fixator [Table/Fig-2].
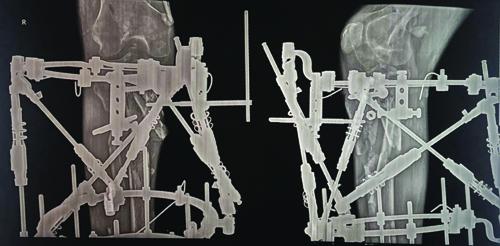
Post removal radiograph with anteroposterior and lateral views keeping the complexities of the present case in mind the authors decided to go for the OSF system to achieve alignment of the knee to the original axis and correction of the limb shortening.

Considering the complexities of the present case, the authors decided to go for the Orthopaedic Spanning Fixation (OSF) system to achieve alignment of the knee to the original axis and correct
Curettage of the fracture sites was done and intraoperatively, it was discovered that the patient had a full-thickness quadriceps muscle loss. Correction of the deformity was achieved using the OSF [Table/Fig-3] and distal tibia corticotomy was done to induce lengthening. This was followed-up with a strict and computerised distraction-compression charting program. This distraction-compression cycle was done for three months to achieve new bone formation by distraction osteogenesis.
Radiograph of the proximal tibia with the hexapod frame in-situ.
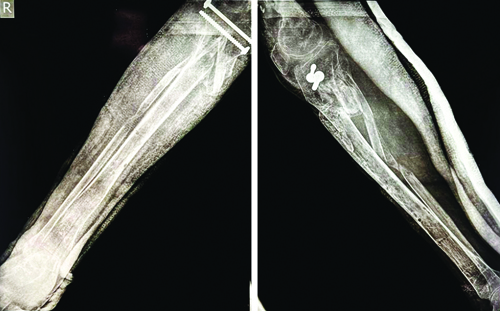
By the end of three months, the deformity correction and required limb lengthening had been achieved; by the end of three months but the proximal tibia fragment remained displaced. The authors decided on the removal of hexapod and fixing the displaced proximal tibia fragment using Cannulated Cancellous Screws (CCS) [Table/Fig-4] followed by a six-week non weight-bearing after which the patient demonstrated normal Range of Motion (ROM) and full weight-bearing walking, initially with the help of a gradually discontinued walker.
Postoperative radiograph after fixation of the proximal tibia using CC screws- anteroposterior and lateral views.
Discussion
The term “floating knee” was first introduced by Blake R and McBryde A in 1975 [1]. This condition involves simultaneous fractures in the femur and tibia on the same side of the body. These breaks can occur in the diaphysis, metaphysis, or even the articular complex, effectively “disconnecting” the knee from the rest of the limb. The majority of patients are men in their thirties [2]. The majority of floating knee cases are caused by Road Traffic Accidents (RTA), followed by falls from height, often occurring as part of polytrauma. Ipsilateral fractures of the femur and tibia in adults, FKI, are serious and have a high complication rate.
The FKIs can lead to several complications, including infection, excessive blood loss resulting in limb shortening, fat embolism, malunion, delayed or non union, knee stiffness, prolonged hospitalisation and inability to bear weight [3]. The management of femur and tibia fractures in polytrauma patients has been a subject of debate. Due to the high mortality rate associated with delayed immobilisation in these patients, treatment strategies have evolved. The earlier approach of Early Total Care (ETC) led to significant complications in unstable patients. This has shifted to the current concept of DCO, which involves immobilising the fracture using external fixation [4,5].
The DCO prioritises immediate life-saving procedures, with definitive treatment considered only after the patient is stabilised in the intensive care unit. Using external fixation for the initial stabilisation of major fractures helps control bleeding and reduces the risk of the “second hit” phenomenon [6]. This phenomenon stems from the fact that sequential insults that are individually trivial could end up in overwhelming physiological reactions. This strategy also avoids time-consuming procedures that can exacerbate the “triad of death,” a term describing the decompensation caused by acute blood loss, leading to hypothermia, coagulopathy and acidosis [7]. The timing for definitive fracture fixation after initial stabilisation with an external fixator is a debated topic and generally depends on the patient’s overall condition and soft tissue recovery.
In the 1950s, Professor Gavriil Abramovich Ilisarov (1921-1992) of Russia introduced a ground-breaking circular or ring external fixator. These fixators are utilised to tackle challenging scenarios like infected non unions, limb shortening via bone lengthening and correcting joint and bone deformities, either individually or combined [8]. Correcting complex deformities, particularly rotational ones, often involved intricate techniques and large, cumbersome frame designs, leading to extended treatment times, higher costs and decreased patient compliance [9]. Keeping these issues in mind, the authors decided to go for a hybrid hexapod system that could achieve deformity correction as well as limb lengthening simultaneously. The OSF frame system represents an advanced evolution in external fixation technology, particularly suited for complex deformity correction. Unlike traditional Ilisarov frames, the OSF system utilises a hexapod structure that offers multi-axial correction capabilities.
Its computer-assisted design integrates radiographic data and allows for precise adjustments in real-time, making it ideal for cases requiring both rotational and angular corrections, as well as limb lengthening. Modality of the nodes of this platform don’t require orthogonal fixation of the rings, nor strict locations for strut fixation. The struts are fixed to each ring in only three places and external supports of any geometry can be used (rings, half-rings, 5/8 rings, triangles, polygonal). Struts can be fixed to the basic rings as well as to the stabilisers and there is no necessity to change the struts during deformity correction [10,11].
The software accompanying the OSF system facilitates detailed preoperative planning, error detection and visualisation of deformity correction outcomes. This enables surgeons to achieve accurate and predictable results, improving patient compliance and reducing treatment time. In the present case, the OSF system allowed simultaneous correction of the rotational deformity and limb shortening, providing a more streamlined and efficient approach compared to bulkier, more cumbersome traditional frames. The frame’s versatility in fixation points and its ability to accommodate various ring geometries further enhanced its effectiveness in this complex case.
The OSF system’s utility in treating severe deformities and its adaptability for limb lengthening offer a significant advantage over older systems. Its six-axis control allows for meticulous deformity correction with minimal patient discomfort, making it a powerful tool in modern orthopaedics. Furthermore, it provides visual simulations of deformity correction outcomes, enabling the users to adjust parameters interactively to achieve desired results. Moreover, the software features built-in error detection mechanisms to promptly identify and rectify measurement inaccuracies made by users [11].
In the present case, the combination of deformity correction and distraction osteogenesis using the OSF system led to a successful outcome, with the patient regaining normal range of motion and full weight-bearing function.
The findings of the present case report align with existing literature on the use of the OSF frame in managing complex deformities, highlighting its effectiveness in correcting severe malalignments and limb length discrepancies. Solomin LN et al., demonstrated that the OSF simplifies deformity correction, reducing treatment time significantly-by 2.3 times in complex deformities and by 1.6 times in moderate deformities [12]. In the present case, the OSF system was instrumental in achieving precise correction of a neglected rotational deformity and limb shortening within a period of three months, a timeframe comparable to or shorter than traditional methods. This supports Solomin’s findings that the OSF system not only improves efficiency but also reduces patient burden by shortening the overall treatment duration.
Additionally, Seide K et al., reported excellent outcomes in correcting translational deformities up to 40 mm and rotational deformities up to 33 degrees, with median residual deformities of 3.5 mm and 1 degree [13]. Similarly, the present case demonstrated successful rotational correction, achieving alignment of the knee to its original mechanical axis with minimal residual deformity. Post-correction radiographs revealed satisfactory anatomical restoration, corroborating Seide K et al., findings that the OSF provides high precision in both angular and rotational deformity correction. The ability to achieve these results with residual deformities of less than 5 mm and 1 degree further underscores the accuracy and versatility of the OSF system [14].
Other studies investigating the efficacy of the OSF frame in treating complex deformities of the tibia and femur have consistently reported positive outcomes. These studies emphasise the OSF’s capability to address challenging cases, particularly those involving rotational and translational malalignments, while maintaining the integrity of soft tissues. In the present case, the OSF was instrumental in managing a difficult situation involving full-thickness quadriceps muscle loss and poor skin condition. Despite these complications, the frame allowed for precise deformity correction and successful limb lengthening, reflecting the high adaptability of the OSF system in handling multifaceted clinical presentations [14-16].
Moreover, the computerised aspect of the OSF, as highlighted in Solomin LN et al., work, greatly enhances surgical planning and intraoperative decision-making [11]. In the present case, the OSF software provided real-time data integration, enabling accurate bone lengthening and deformity correction through distraction osteogenesis. This matches the experiences of other studies where the OSF’s computerised guidance significantly reduced errors and allowed for visual simulations of the correction process [11]. Such technology-driven precision ensures that even severe cases like the present case, where deformity and malunion had already set in, can be corrected without compromising the overall recovery trajectory.
The present study findings echo those of Solomin LN, Seide K et al., and other studies, further validating the Orthopaedic Surgical Frame (OSF) as a powerful tool for managing complex orthopaedic deformities [11-15]. The accuracy, efficiency and versatility of the system, as demonstrated in the present case and in the literature, suggest that it should be considered a first-line approach in treating similar complex deformities, particularly those involving malunion and limb shortening. The ability to correct deformities while minimising residual alignment errors and reducing treatment duration makes the OSF a superior option compared to traditional methods, especially in challenging clinical scenarios.
Conclusion(s)
The present case report highlights the successful use of the OSF frame in treating a complex floating knee injury with rotational deformity and limb shortening following delayed presentation. Key messages from the present case include the importance of timely follow-up in managing severe orthopaedic trauma and the challenges posed by neglected injuries, which often lead to malunion, deformity and functional impairment. The OSF system proved to be an effective solution for simultaneous deformity correction and limb lengthening, offering precision and flexibility that surpass traditional Ilisarov frames. The use of the OSF system, with its computer-assisted planning and real-time adjustments, allowed for meticulous correction of the external rotation deformity and restoration of limb length, demonstrating the system’s utility in managing complex lower limb injuries. Additionally, the device’s ability to integrate radiographic data ensured accurate alignment and reduced the risk of complications. The present case reinforces the value of advanced external fixation techniques in modern orthopaedic practice, particularly in cases where conventional methods may be inadequate or cumbersome. Overall, the present report underscores the importance of individualised treatment planning, careful follow-up and the potential benefits of advanced fixation systems in achieving optimal patient outcomes in complex fracture cases.
[1]. Blake R, McBryde A, The floating knee: Ipsilateral fractures of the tibia and femurSouth Med J 1975 68:13-16. [Google Scholar]
[2]. Elmrini A, Elibrahimi A, Agoumi O, Boutayeb F, Mahfoud M, Elbardouni A, Ipsilateral fractures of tibia and femur or floating kneeInt Orthop 2006 30:325-28.10.1007/s00264-006-0084-016525817PMC3172778 [Google Scholar] [CrossRef] [PubMed]
[3]. Veith RG, Winquist RA, Hansen ST Jr, Ipsilateral fractures of the femur and tibia. A report of fifty-seven consecutive casesJ Bone Joint Surg Am 1984 66:991-1002.10.2106/00004623-198466070-000046480657 [Google Scholar] [CrossRef] [PubMed]
[4]. D’Alleyrand JC, O’Toole RV, The evolution of damage control orthopedics: Current evidence and practical applications of early appropriate careOrthop Clin North Am 2013 44(4):499-507.10.1016/j.ocl.2013.06.00424095066 [Google Scholar] [CrossRef] [PubMed]
[5]. Lichte P, Kobbe P, Dombroski D, Pape HC, Damage control orthopedics: Current evidenceCurr Opin Crit Care 2012 18(6):647-50.10.1097/MCC.0b013e328359fd5723037876 [Google Scholar] [CrossRef] [PubMed]
[6]. Lasanianos NG, Kanakaris NK, Giannoudis PV, Intramedullary nailing as a ‘second hit’ phenomenon in experimental research: Lessons learned and future directionsClin Orthop Relat Res 2010 468(9):2514-29.10.1007/s11999-009-1191-120012236PMC2919890 [Google Scholar] [CrossRef] [PubMed]
[7]. Rozbruch SR, Fragomen AT, Ilizarov S, Correction of tibial deformity with use of the Ilizarov-Taylor spatial frameJ Bone Joint Surg Am 2006 88(suppl 4):156-74.10.2106/JBJS.F.0074517142445 [Google Scholar] [CrossRef] [PubMed]
[8]. Golyakhovsky V, Frankel VH, Textbook of Ilizarov Surgical Techniques: Bone Correction and Lengthening: Bone Correction and Lengthening 2010 Delhi, IndiaJaypee Brothers Medical Publishers10.5005/jp/books/11150 [Google Scholar] [CrossRef]
[9]. Dhawan M, Sharma A, Chauhan R, Vig V, Prasad M, Taylor spatial frame versus ortho SUV for correction of lower limb deformities: A comparative studyJ Mar Med Soc 2023 25(2):109-14.10.4103/jmms.jmms_130_22 [Google Scholar] [CrossRef]
[10]. Paley D, History and science behind the six-axis correction external fixation devices in orthopaedic surgeryOper Tech Orthop 2011 21:12502810.1053/j.oto.2011.01.011 [Google Scholar] [CrossRef]
[11]. Solomin LN, Deformity correction and fracture treatment using the software-based Ortho-SUV frameIn: The Basic Principles of External Skeletal Fixation using the Ilizarov and Other Devices 2012 2nd editionMilan, Heidelberg, New YorkSpringer-Verlag:159310.1007/978-88-470-2619-3_17 [Google Scholar] [CrossRef]
[12]. Solomin LN, Paley D, Shchepkina EA, Vilensky VA, Skomoroshko PV, A comparative study of the correction of femoral deformity between the Ilizarov apparatus and Ortho-SUV FrameInt Orthop 2014 38(4):865-72.Epub 2013 Dec 2810.1007/s00264-013-2247-024370977PMC3971274 [Google Scholar] [CrossRef] [PubMed]
[13]. Seide K, Wolter D, Kortmann HR, Fracture reduction and deformity correction with the hexapod Ilizarov fixatorClin Orthop Relat Res 1999 (363):186-95.10379322 [Google Scholar] [PubMed]
[14]. Takata M, Vilensky VA, Tsuchiya H, Solomin LN, Foot deformity correction with hexapod external fixator, the Ortho-SUV Frame™J Foot Ankle Surg 2013 52(3):324-30.10.1053/j.jfas.2013.01.01323522737 [Google Scholar] [CrossRef] [PubMed]
[15]. Zodey K, Mankar S, Agrawal PP, The management of complex knee deformity using Ortho-SUV: A case studyCureus 2024 16(8):e6806510.7759/cureus.6806539347215PMC11436753 [Google Scholar] [CrossRef] [PubMed]
[16]. Skomoroshko PV, Vilensky VA, Hammouda AI, Fletcher MD, Solomin LN, Mechanical rigidity of the Ortho-SUV frame compared to the Ilizarov frame in the correction of femoral deformityStrategies Trauma Limb Reconstr 2015 10(1):05-11.Epub 2015 Feb 2610.1007/s11751-015-0214-625716478PMC4395562 [Google Scholar] [CrossRef] [PubMed]