Prenatal Ultrasonic Diagnosis of Persistent Right Umbilical Vein with Single Umbilical Artery in Twin Pregnancy: A Case Report
Shubhi Gaur1, Pratap Singh Parihar2, Vaishali Dhawan3, Devyansh Nimodia4, Prasad Sanjay Desale5
1 Junior Resident, Department of Radiodiagnosis, Datta Meghe Institute of Higher Education and Research, Sawangi, Wardha, Maharashtra, India.
2 Head, Department of Radiodiagnosis, Datta Meghe Institute of Higher Education and Research, Sawangi, Wardha, Maharashtra, India.
3 Professor, Department of Radiodiagnosis, Datta Meghe Institute of Higher Education and Research, Sawangi, Wardha, Maharashtra, India.
4 Junior Resident, Department of Radiodiagnosis, Datta Meghe Institute of Higher Education and Research, Sawangi, Wardha, Maharashtra, India.
5 Junior Resident, Department of Radiodiagnosis, Datta Meghe Institute of Higher Education and Research, Sawangi, Wardha, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Shubhi Gaur, Junior Resident, Department of Radiodiagnosis, Datta Meghe Institute of Higher Education and Research, JNMC Campus, Sawangi, Wardha-442001, Maharashtra, India.
E-mail: imboss.shubhi@gmail.com
Persistent Right Umbilical Vein (PRUV) is a developmental abnormality of the vascular system that occurs during embryonic development when the right umbilical vein remains open while the left umbilical vein becomes atretic. PRUV presents in two forms: the extrahepatic variety, which is less prevalent but more often associated with complications, and the intrahepatic type, which is the most common (90-95%). A Single Umbilical Artery (SUA) occurs when there is only one umbilical artery in the cord, and it is associated with an increased risk of various abnormalities, including cardiovascular defects. Hereby, the authors present a case report of a 32-year-old primigravida, approximately 20.3 weeks into her pregnancy, underwent an anomaly scan that revealed a two-vessel umbilical cord, showing an SUA and a PRUV in one of the foetuses, while both foetuses demonstrated normal intrauterine growth. PRUV in foetuses is linked to preterm births, oligohydramnios, and intrauterine growth restriction. It can also lead to gastrointestinal malformations, various cardiac anomalies, skeletal malformations, urinary tract anomalies, and SUA defects. Therefore, prenatal diagnosis of PRUV is essential.
Cardiovascular anomalies, Foetal echocardiogram, Gallbladder duplication, Intrauterine growth restriction
Case Reprort
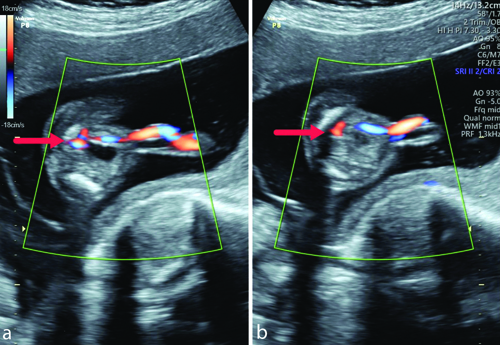
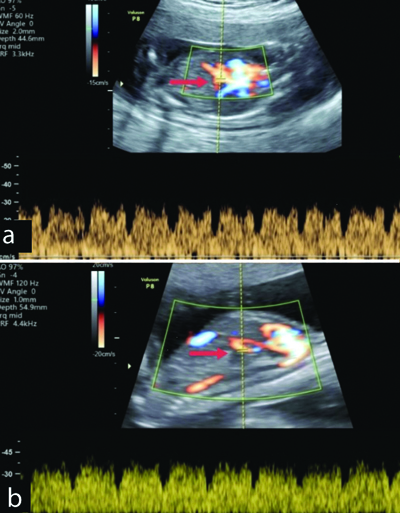
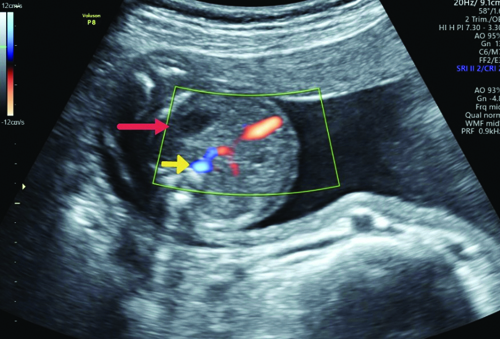
A 32-year-old primigravida in her second trimester, with Rhesus factor (Rh)-negative status, visited the department for her first prenatal appointment. The dating scan, performed at a secondary care centre, showed the presence of two intrauterine gestational sacs with yolk sacs and foetal poles corresponding to five weeks and five days, with normal cardiac activities and an inter-twin membrane in between. During the first trimester, routine investigations were conducted as usual. In the late first trimester, the patient was advised to undergo a double marker test and a Nuchal Translucency (NT) scan, in which the maternal free beta-Human Chorionic Gonadotropin (HCG) and Pregnancy Associated Plasma Protein A (PAPP-A) levels are combined with the NT scan; both parameters were normal. This is a rural hospital set-up where most of the pregnant females belong to lower socio-economic status, and many of the patients are lost to follow-up. The patient did not have the means to undergo chromosomal microarray testing and was unwilling to be admitted at that time to undergo a foetal echocardiogram. Thus, both additional investigations were not performed. About 20.3 weeks into the pregnancy, an anomaly scan was performed at study centre, and the results showed a two-vessel umbilical cord on cross-section, indicating a SUA and a PRUV in one of the foetuses, while both foetuses showed normal intrauterine growth [Table/Fig-1a,b]. The ductus venosus flow pattern of both twins was found to be in its normal anatomical position and within normal limits [Table/Fig-2a,b].
Grey scale B mode images of axial sections of the abdomen at the level of the urinary bladder shows Single Umbilical Artery (SUA) and vein (red arrow).
a,b) Mid sagittal sections of the twin fetuses showing normal colour flow of ductus venosus as marked by red arrow in twin a and twin b.
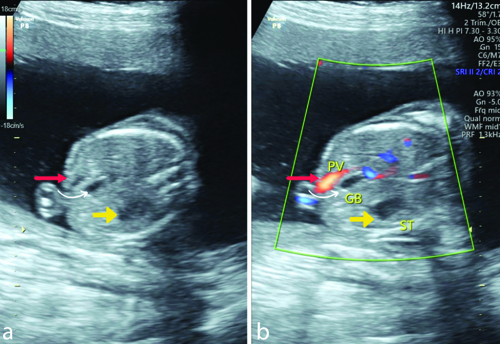
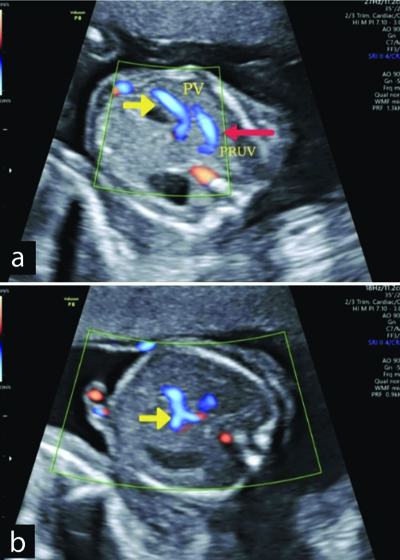
The foetal gallbladder was positioned medially, suggesting PRUV. The portal vein was observed bending towards the stomach in the axial section at the level of the foetal abdominal girth during the targeted anomaly scan [Table/Fig-3a,b]. Tracing the PRUV revealed that it also connected to the portal system, indicating intrahepatic drainage. In further cranial sections of the abdomen, just oblique to the midline sagittal plane, the PRUV was visualised lateral to the portal vein, which was seen branching [Table/Fig-4a,b]. No other structural or cardiac abnormalities were observed. When examining the abdominal sections of the other twin, the normal relationship of the portal vein and the gallbladder was noted [Table/Fig-5]. A good prognosis was given to the parents, and the pregnancy was carried to term, resulting in the delivery of two healthy twins. The female twin was later discharged on postoperative day 4 without any complications for either her or the twins.
In the above axial section of the abdomen at the level of the stomach bubble, the anechoic gallbladder marked by a curved white arrow, lies in between the portal vein as marked by red arrow and the stomach bubble marked by a yellow arrow.
a,b) Oblique and axial sections of the abdomen showing PRUV marked by red arrow lying lateral to the portal vein which can be seen branching in marked by yellow arrow.
Abdominal section of the second twin showing portal vein marked by yellow arrow lying medially to the gallbladder as marked by red arrow.
Discussion
In a typical embryo, the right umbilical vein gradually begins to atrophy at week four and fully disappears by week seven. The left umbilical vein returns blood from the placenta to the inferior vena cava through the ductus venosus formed in the liver, remaining intact while the proximal segment of the left umbilical vein, that is, the section between the liver and the sinus venosus, also degenerates later [1]. Consequently, PRUV occurs when the right umbilical vein remains intact while the left umbilical vein atrophies and degenerates [2]. The reported incidence of PRUV, an unusual disorder, ranges from one in 250 to one in 1,250 [3]. Gastrointestinal malformations, various cardiac anomalies, skeletal malformations, urinary tract anomalies, and SUA are among the many defects linked to PRUV [4]. The most common associated congenital defects are cardiovascular malformations, followed by neurological malformations. To date, no correlation between chromosomal abnormalities and any particular case has been discovered [1].
Differential diagnosis of PRUV include umbilical vein varix, gallbladder duplication, intrahepatic cysts, and abnormal courses of the portal vein and its branches [5]. Careful assessment of location using colour and pulsed Doppler ultrasound will aid in the diagnosis. Foetal PRUV should be detected during prenatal ultrasound examinations, and a foetal echocardiogram along with a thorough assessment of other foetal structures should be conducted to rule out abnormalities in other systems. Recent investigations have revealed that PRUV is not an extremely rare disorder, with an incidence of 0.08% to 0.5%, due to advances in ultrasound technology and increased understanding of foetal venous system assessment [6].
The other common umbilical cord vascular abnormality is called SUA, which occurs when there is only one umbilical artery instead of two in the cord. About 0.5% to 6% of pregnancies are affected by this condition [7,8]. There is evidence linking SUA to congenital abnormalities, premature delivery, intrauterine growth restriction, and poor foetal obstetric outcomes. Risk factors for SUA include twin pregnancies, velamentous insertion, advanced maternal age, smoking, as well as conditions such as diabetes, hypertension, and seizure disorders in women [9].
In a case report published by Mohapatra I and Samantaray SR, a primigravida with a single intrauterine live foetus presented with PRUV and SUA, who underwent a caesarean section to deliver a healthy baby [10]. Regular follow-up was undertaken to monitor for Intrauterine Growth Restriction (IUGR) and oligohydramnios; however, none of these antenatal complications were encountered, which is similar to the outcome in our case.
In another research article published by Li J et al., it was found that the most common anomaly in complicated PRUV cases involved the Cardiovascular System (CVS), followed by the nervous system [11]. A few of these cases had SUA, which were associated with cardiovascular anomalies. However, in present case, the anomaly scan did not reveal any obvious CVS abnormalities.
In a brief communication published by Shah N, author presented a case report on an elderly second gravida with PRUV that was not associated with other structural anomalies of the foetus [12]. Author further concluded that determining the type of PRUV would help in better counselling of parents, leading to improved outcomes for the pregnancy.
Types of PRUV:
Type 1 or Intrahepatic PRUV (PRUV-I), is the most common with 95% of instances documented [13]. In PRUV-I, the Umbilical Vein (UV) bends towards the stomach after passing lateral to the right-side of the gallbladder and connects to the Portal Vein (PV). There is a small amount of haemodynamic interference, and the ductus venosus is typically present. The outlook for this type of PRUV is favourable. The present case belonged to type 1 PRUV.
Type 2 is the Extrahepatic PRUV (PRUV-E), in which the right atrium or the Inferior Vena Cava (IVC) is directly connected to the UV [13]. A worse prognosis and ductus venosus agenesis are associated with PRUV-E. If the ductus venosus is absent, blood returns directly to the heart, which could lead to an increased burden on the heart. Foetal hydrops can result from severe haemodynamic consequences and volume overload in the affected foetuses.
Conclusion(s)
Foetal PRUV should be detected during a prenatal ultrasound examination. While foetuses with isolated PRUV are not at high-risk of chromosomal abnormalities, foetuses with extensive PRUV should undergo foetal chromosomal screening. The prognosis for isolated PRUV is favourable, while that of complicated PRUV is influenced by the type and degree of concurrent abnormalities. Further research is necessary to determine whether PRUV is a developmental disorder or an anatomical variation.
Author Declaration:
Financial or Other Competing Interests: None
Was Ethics Committee Approval obtained for this study? Yes
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. NA
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 30, 2024
Manual Googling: Aug 31, 2024
iThenticate Software: Sep 02, 2024 (14%)
[1]. Martinez R, Gamez F, Bravo C, Sánchez P, Orizales C, Ortiz L, Perinatal outcome after ultrasound prenatal diagnosis of persistent right umbilical veinEur J Obstet Gynecol Reprod Biol 2013 168:36-39.10.1016/j.ejogrb.2012.12.01923317918 [Google Scholar] [CrossRef] [PubMed]
[2]. Yagel S, Kivilevitch Z, Cohen SM, Valsky DV, Messing B, Shen O, The fetal venous system, part I: Normal embryology, anatomy, hemodynamics, ultrasound evaluation and Doppler investigationUltrasound Obstet Gynecol 2010 35:741-50.10.1002/uog.761820205155 [Google Scholar] [CrossRef] [PubMed]
[3]. Pinna G, De-Carolis MP, Lanzone A, Sordo GD, Botta A, Carolis S, Persistence of right umbilical vein: A singular caseTurk J Pediatr 2020 62:338-42.10.24953/turkjped.2020.02.02432419430 [Google Scholar] [CrossRef] [PubMed]
[4]. Wolman I, Gull I, Fait G, Amster R, Kupferminc MJ, Lessing JB, Persistent right umbilical vein: Incidence and significanceUltrasound Obstet Gynecol 2002 19:562-64.10.1046/j.1469-0705.2002.00678.x12047534 [Google Scholar] [CrossRef] [PubMed]
[5]. Weichert J, Hartge D, Germer U, Axt-Fliedner R, Gembruch U, Persistent right umbilical vein: A prenatal condition worth mentioning?Ultrasound Obstet Gynecol 2011 37:543-48.10.1002/uog.776420922781 [Google Scholar] [CrossRef] [PubMed]
[6]. Blazer S, Zimmer EZ, Bronshtein M, Persistent intrahepatic right umbilical vein in the fetus: A benign anatomic variantObstet Gynecol 2000 95:433-36.10.1016/s0029-7844(99)00564-510711558 [Google Scholar] [CrossRef] [PubMed]
[7]. Granese R, Coco C, Jeanty P, The value of single umbilical artery in the prediction of fetal aneuploidy: Findings in 12,672 pregnant womenUltrasound Q 2007 23:117-21.10.1097/01.ruq.0000263848.07808.0217538487 [Google Scholar] [CrossRef] [PubMed]
[8]. Thummala MR, Raju TN, Langenberg P, Isolated single umbilical artery anomaly and the risk for congenital malformations: A meta-analysisJ Pediatr Surg 1998 33:580-85.10.1016/s0022-3468(98)90320-79574755 [Google Scholar] [CrossRef] [PubMed]
[9]. Leung AK, Robson WL, Single umbilical artery. A report of 159 casesAm J Dis Child 1989 143:108-11.10.1001/archpedi.1989.021501301180302910035 [Google Scholar] [CrossRef] [PubMed]
[10]. Mohapatra I, Samantaray SR, Persistent right umbilical vein in association with single umbilical artery: A case report and review of literatureCureus 2023 15(3):e3654410.7759/cureus.36544 [Google Scholar] [CrossRef]
[11]. Li J, Yuan Q, Ding H, Yang Z, Wang B, Wang B, Ultrasonic detection of fetal persistent right umbilical vein and incidence and significance of concomitant anomaliesBMC Pregnancy Childbirth 2020 20(1):61010.1186/s12884-020-03310-233036561PMC7547413 [Google Scholar] [CrossRef] [PubMed]
[12]. Shah N, Prenatal diagnosis of persistent right umbilical vein: Is it significant?J Fetal Med 2018 5:49-51.10.1007/s40556-017-0142-2 [Google Scholar] [CrossRef]
[13]. Chaoui R, Kalache KD, Hartung J, Application of three-dimensional power Doppler ultrasound in prenatal diagnosisUltrasound Obstet Gynecol 2001 17:22-29.10.1046/j.1469-0705.2001.00305.x11244651 [Google Scholar] [CrossRef] [PubMed]