Introduction
A persistent, precancerous, and frequently debilitating condition, OSMF is characterised by a slowly progressing fibrosis of the oropharynx and oral cavity. Chewing Areca Nut (AN) is the main cause of the illness; 10 to 20% of people worldwide have this addictive habit. The areca catechu palm tree nut is chewed either by itself or in conjunction with other substances to induce euphoria and ease tension, depending on local customs [1]. In India, AN is typically consumed with slaked lime, tobacco, and occasionally spices to form a betel quid. Furthermore, the usage of commercially freeze-dried AN products (like gutkha) has grown in popularity; these products have particularly high AN concentrations and may accelerate the development of OSMF compared to traditional betel quid. The onset of the illness may also be influenced by a hereditary predisposition. OSMF frequently affects young adults who use betel quid. At first, the patient may report a burning sensation or sensitivity to spicy foods. Early disease stages may show vesicles, petechiae, and melanosis upon oral examination. Hyposalivation is also one of the symptoms seen in OSMF patients [1].
Saliva is a valuable oral fluid that is sometimes overlooked, but it is important to understand how crucial it is for preserving oral health. Saliva performs a multitude of tasks in the mouth, including lubrication, shielding the oral mucosa, pellicle formation, digestion, and possessing medicinal qualities. Saliva contains proteins with antiviral, antibacterial, and antifungal characteristics [2]. By protecting the oral cavity from various infections, saliva, in its normal quantity and composition, serves as the most significant component of the host immune system. Any variation in salivary flow can affect its pH, which is crucial for buffering function, leading to tooth enamel demineralisation. Loss of taste is due to damage to taste buds or hyposalivation. Additional complications associated with hyposalivation could include halitosis, or oral malodor, and dental caries, which typically affect smooth surfaces and areas that aren’t usually susceptible to caries, such as the lower incisor region [3]. Additionally, caries can affect roots and can be quite severe and challenging to treat.
Sialogogues are used to stimulate salivation, such as sorbitol, xylitol, and pilocarpine, in patients with hyposalivation. However, sialogogues can have side effects, such as increased sweating and diarrhoea [4]. To overcome this problem, newer techniques like TENS have been used to treat hyposalivation in OSMF.
Using electric current to stimulate nerves for therapeutic purposes, TENS serves as a simple, affordable, and non invasive method. It is a commonly used non-pharmacological pain treatment technique [5]. In the past, TENS was primarily used to treat pain, but not much research has been conducted in clinical trials to determine how electrical nerve stimulation affects salivary flow. Theoretically, applying electric impulses to any one of the three components of the salivary reflex arc should increase salivary production and reduce the long-lasting effects of hyposalivation [2].
A number of investigations and incidents have documented the presence of variable salivary flow. Khader NFA and Dyasanoor S (2015) conducted a study on the alteration of salivary properties and taste [1]. Another study was carried out by Chandra R et al., (2022) to assess the effectiveness of TENS on the salivary flow rate in xerostomia patients [2]. Nonetheless, evidence correlating the number of variations in saliva before and after TENS treatment in OSMF patients is sparse regarding these parameters. This underscores the intention of the present study.
The aim of present study is to evaluate and compare the salivary flow rate in OSMF patients before and after TENS. The primary objective of the study is to evaluate the salivary flow rate in OSMF patients before and after TENS. The secondary objective of the study is to compare the salivary flow rate in OSMF patients before and after TENS.
Null hypothesis: There will be no significant change in salivary flow rate on comparing OSMF patients before and after TENS therapy
Alternate hypothesis: There will be significant change in salivary flow rate on comparing OSMF patients before and after TENS therapy
Review of Literature
Ramesh C et al., undertook a study to determine the effect of TENS on salivary flow rates in healthy adult populations, divided according to gender and age. The study included saliva samples from 130 healthy individuals, collected in both stimulated and unstimulated states, and their TENS flow rates were analysed. They concluded that the maximum salivary flow rate was observed in the age group of 20-29. Additionally, TENS was shown to be a non pharmacological, safer therapy choice for patients with xerostomia [6].
Tabres S et al., (2022) carried out a study to investigate TENS’s effectiveness on the total salivary flow rate through a descriptive observational study. This study included 200 individuals divided into two separate groups, where saliva samples, both stimulated and unstimulated, were gathered in graduated beakers for a period of five minutes with the TENS unit activated at 50 Hz. They concluded that the positive results indicate an increase in salivary secretions in both aged and diabetic patients [4].
Konidena A et al., (2016) conducted a study to stimulate salivation in postmenopausal women, regardless of whether they had dry mouth. Based on their responses to the Xerostomia Inventory, 50 postmenopausal women were enrolled in the study and split into two groups of 25: one group consisted of postmenopausal women who experienced Oral Dryness (PMD+OD), while the other group included those who did not (PMD-OD). Unstimulated whole saliva collection was accomplished using a low-force spitting technique. Following external salivary stimulation of the parotid gland with TENS unit electrodes, repeated sialometry was performed. The salivary flow rates within both groups were measured both before and after stimulation, as well as between the two groups. Lower salivary flow rates were observed in postmenopausal women who reported experiencing dry mouth. Regardless of their level of mouth dryness, 90% of the individuals showed improvement after TENS treatment. In postmenopausal women with or without oral dryness, TENS stimulation significantly increased the overall saliva flow rate [7].
Paim ED et al., (2017) evaluated the effects of TENS on radiation-induced hyposalivation in the head and neck region, involving 15 patients with head and neck cancer. The study used TENS calibrated at a frequency of 50 Hz and a pulse width of 250 μs, with intensity modifications over a 20-minute interval. The patients had an average age of 56.8±6.46 years. Salivary flow increased from 0.05 (0.00; 0.40) mL/min to 0.10 (0.07; 0.40) mL/min following TENS (p=0.0051). Thus, in individuals with radiation therapy-induced hyposalivation, TENS improved salivary flow [8].
Yang LY et al., studied how electrical stimulation of acupoints affected xerostomia in individuals undergoing haemodialysis. The study included a total of 75 participants: 38 in the comparison group and 37 in the Transcutaneous Electrical Acupoint Stimulation (TEAS) group. For a duration of three weeks, three times each week, the comparison group employed a frequency of 50 μs and 2 Hz. In contrast, the TEAS group used frequencies of 50 Hz and a pulse width of 250 μs. Prior to, during, and following the program, authors measured the percentage of Inter-Dialytic Weight Gain (IDWG), salivary flow rates, and dry mouth symptoms. The results demonstrated that xerostomia patients undergoing haemodialysis can effectively manage their symptoms by implementing a TEAS program. Thus, it can be applied to treat the symptoms of xerostomia in patients undergoing haemodialysis [9].
Materials and Methods
The prospective research will be conducted at the Oral Medicine and Radiology (OMR) Department of Sharad Pawar Dental College, Sawangi, Wardha, Maharashtra, India, focusing on Indian subjects. The duration of the study will be two years from July 2024 to July 2026. Study approval has been obtained prior to the study (DMIHER (DU)/IEC/2024/224) from the Institutional Ethics Committee (IEC) of DMIHER (DU), Sawangi, Wardha.
Inclusion criteria: The study will include patients aged 18 to 45 years. Individuals with clinically and functionally established OSMF Stage-I (characterised by a burning sensation in the mouth), OSMF Stage-II (where the buccal mucosa appears mottled and marble-like, with widespread sheets of palpable fibrosis, and an interincisal distance of 26 to 35 mm), OSMF Stage-III (with an interincisal distance of 15 to 25 mm, a pale buccal mucosa that is firmly attached to the underlying tissues, atrophy of the vermilion border, and vertical fibrous bands palpable at the soft palate and buccal mucosa), and OSMF Stage-IV (which presents with severe trismus, interincisal distance of less than 15 mm, thickened faucial pillars, shrunken uvula, restricted tongue movement, and the presence of a circular band around the entire lip and mouth) will be included [10]. Patients with a history of decreased salivation for more than six months will also be incorporated into the study group. Clinical examination will reveal hyposalivation due to habit-induced OSMF.
Exclusion criteria: The study will exclude patients undergoing treatment for OSMF, those with any salivary gland disorder (regardless of whether they are currently on medication for it), and individuals with a history of stress, systemic conditions or diseases likely to decrease salivation, radiation therapy, mental illness, oral mucosal lesions, and denture wear. Additionally, participants using medications that could affect salivary parameters, such as diuretics, anticholinergics, antihistamines, antihypertensives, and psychotropic substances, will not be considered. Those with prolonged habits of smoking and alcohol consumption are also excluded from the study.
Sample size calculation: The sample size was calculated based on the difference in mean values for the variable salivary flow rate, which is the primary variable, between pre- and postoperative treatment, considering the standard deviation. It is expected that after TENS application, there will be an increase in salivary flow rate. Thus, we are considering an estimated value of a 30% increase in salivary flow rate, i.e., (30 * 23.4) / 100=7.02. Therefore, the increased mean salivary flow rate will be 7.02+23.4=30.42.
Formula using mean difference:
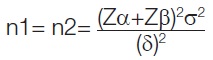
Zα=1.96 at 5% error and CI at 95%
Zβ=0.84=Power at 80%
Mean salivary flow rate (mm) 23.4 and SD=7.1 in OSMF patients [1].
Considering 30% more in flow rate after TENS application in Mean salivary flow rate (mm)=30.42 mm.
Standard deviation=7.1
Thus, sample size=17 per group minimum.
Study Procedure
Patients who are willing to participate in the study and report to the Oral Medicine and Radiology department will be included. Each patient will undergo a detailed clinical examination and history after providing their informed written consent. A thorough medical history will be recorded to rule out systemic illnesses or the use of medications that may alter taste perception. Additionally, a detailed habit history, such as smoking and alcohol consumption, which can affect salivary flow rate, will be noted.
A comprehensive intraoral examination will be performed to assess patients whose mouth opening is reduced as a result of OSMF. This examination will include checking for the absence of mucosal lesions and salivary gland enlargements. Patients will be evaluated based on the following questionnaire [Table/Fig-1] [11,12]. According to the functional classification system established by Khanna JN and Andrade NN in 1995 [10], four groups will be formed based on the responses of patients with OSMF and hyposalivation: Grade 1, Grade 2, Grade 3, and Grade 4 OSMF, with 13 patients in each group.
Xerostomia inventory questionnaire for hyposalivation [11,12].
| Hyposalivation |
|---|
| Higher scores indicate more severe symptoms of chronic xerostomia. The Inventory of Xerostomia (XI) is an 11-element combined grading measures that aggregates replies to 11 separate elements in the same continuous scaled score [11]. The following statements, which relate to the preceding four weeks, are given to the respondents to select among the five answers (“Never”, scoring 1; “Hardly ever”, 2; “Occasionally”, 3; “Fairly often”, 4; and “Very often”, 5). |
| To help with meal swallowing, I drink liquids |
| When I eat, my mouth feels dry/ |
| My mouth feels dry/ |
| I have difficulty in eating dry foods/ |
| I get up in night to drink/ |
| I sip sweets or cough lollipops to ease dry mouth/ |
| I have difficulties swallowing certain foods/ |
| The skin of my face feels dry/ |
| My eyes feel dry/ |
| My lips feel dry/ |
| The inside of my nose feels dry/ |
| The respondents were classified as hypo salivatory subject if they answered Yes to question 1 and/or question 2 in addition to, atleast, one positive answer to one of the symptoms listed in the responses above. To get a single XI score, the responses of each person are scored and added together [11]. |
To minimise bias in the results induced by circadian variation, the study will be conducted in the morning (09:00-11:00 am), and participants will be prohibited from consuming food and beverages for two hours before the scheduled time. Before TENS therapy, the Modified Schirmer Test (MST) will be conducted to measure the unstimulated/resting salivary flow rate in OSMF patients [1]. The MST protocol [1,12] used in this investigation is shown in [Table/Fig-2].

Before the test, the patient will be instructed to swallow all saliva in their mouth and to refrain from swallowing during the test, following a three-to-five-minute rest interval. To prevent the test strip from making contact with the tongue during the procedure, the patient will also be asked to rest their tongue on the hard palate. Using a cotton plier to hold the MST strip vertically, the rounded end of the strip will be placed at the floor of the mouth. Saliva will move up the strip when its rounded end comes into contact with moisture, and its length will be measured at one, two, and three minutes, recorded immediately.
After the MST procedure, the salivary flow rate in OSMF patients will be evaluated prospectively using TENS (Sodexo HTM healthcare technology management, Sodexo India Services Pvt., Ltd.) at 40 Hz for 15 minutes during the first visit. Pads will be placed bilaterally over the preauricular region and cheek region, as shown in [Table/Fig-3]. After TENS therapy, a modified Schirmer test will be conducted to measure the stimulated salivary flow rate in patients with OSMF. All findings relevant to the salivary flow rate in OSMF will be recorded in tabular format and subjected to statistical evaluation.
Transcutaneous Electric Nerve Stimulation (TENS).

Outcome variables: The salivary flow rate, which will be assessed using the Modified Schirmer Test (MST).
Primary outcome: Quantitative information about the salivary flow rate will be assessed using the MST before and after TENS therapy. The statistical significance of the change in flow rate will be evaluated using modified Schirmer strips, which are scaled from 5 to 35 mm at 1 mm intervals. The wetting of the strip will be measured after one, two, and three minutes [13].
Secondary outcome: A subjective assessment of the improvement in salivary flow rate will be conducted by administering a xerostomia questionnaire [11].
Statistical Analysis
All results will be calculated using R-Studio software version 4.3.2. The full analysis data set will include all study participants with no missing values for any parameters in the data set. The study subjects will consist of participants who fulfill the inclusion and exclusion criteria. All data will be summarised with baseline characteristics for demographic variables (age, sex, address, occupation, socioeconomic status). These will be described by frequency and percentage for categorical data, and by mean and standard deviation for continuous data. Outcome variables will be analysed over continuous variables, which will be summarised with the minimum, maximum, mean, standard deviation, standard error, and 95% confidence interval for parametric data. Data related to the continuous outcome variables will first be tested for normality using the Kolmogorov-Smirnov test at a 5% level of significance (p≤0.05). If the null hypothesis is rejected, the data will be considered non normal; otherwise, parametric tests will be used to determine significance. The Analysis of Variance (ANOVA) test will be employed to find significant differences at a 5% level (p≤0.05) for four comparative groups before and after intervention therapy. Non normal data will be described by the mean, median, and lower and upper quartiles, and will be analysed using non-parametric tests. The Kruskal-Wallis test will be used to assess significance. Categorical variables will be summarised by frequency (N) and percentage values (%), and analysed using the Chi-square test to determine significance at a 5% level.
[1]. Khader NFA, Dyasanoor S, Assessment of salivary flow rate and pH among areca nut chewers and oral submucous fibrosis subjects: A comparative studyJournal of Cancer Prevention 2015 20(3):20810.15430/JCP.2015.20.3.20826473160 [Google Scholar] [CrossRef] [PubMed]
[2]. Chandra R, Bhakta P, Beniwal J, Dhanda R, Saxena V, Sinha S, Evaluation of the efficacy of transcutaneous electrical nerve stimulation (TENS) on salivary flow rate in patients with xerostomia - A case control studyJ Family Med Prim Care 2022 11(2):767-71.10.4103/jfmpc.jfmpc_922_2135360757 [Google Scholar] [CrossRef] [PubMed]
[3]. Vijayalaxmi N, Ramesh T, Reddy R, Lavanya R, Swapna L, Effects of protocol utilised for collection of whole saliva stimulated by TENS in healthy adult IndiansCumhuriyet Dental Journal 2012 15:235-40.10.7126/cdj.2012.1462 [Google Scholar] [CrossRef]
[4]. Tabres S, Patil N, Sareen M, Meena M, Tyagi N, Kaswan S, Efficacy of Transcutaneous Electric Nerve Stimulation (TENS) on whole salivary flow rate: A descriptive observational studyJ Dent (Shiraz) 2022 23(1 Suppl):214-21. [Google Scholar]
[5]. Singh B, Sheikh S, Pallagatti S, Kaur K, Sohi R, Evaluation of salivary calcium and salivary parathyroid levels in postmenopausal women with and without oral drynessContemp Clin Dent 2013 4(4):488-92.10.4103/0976-237X.12305124403794 [Google Scholar] [CrossRef] [PubMed]
[6]. Ramesh C, Sawant SS, Kolte DR, Kumar B, Kranthi K, Patil TR, Efficacy of transcutaneous electrical nerve stimulation on salivary flow rates in normal healthy adults according to gender and age groupsAsian J Neurosurg 2021 16(4):770-76.10.4103/ajns.AJNS_48_2135071076 [Google Scholar] [CrossRef] [PubMed]
[7]. Konidena A, Sharma D, Puri G, Dixit A, Jatti D, Gupta R, Effect of TENS on stimulation of saliva in postmenopausal women with or without oral dryness - An interventional studyJ Oral Biol Craniofac Res 2016 6(Suppl 1):S44-50.10.1016/j.jobcr.2016.01.00427900250 [Google Scholar] [CrossRef] [PubMed]
[8]. Paim ÉD, Macagnan FE, Martins VB, Zanella VG, Guimarães B, Berbert MCB, Transcutaneous Electrical Nerve Stimulation (TENS) on hyposalivation induced by radiotherapy in the head and neck region: A preliminary studyCodas 2018 30(3):e2017014310.1590/2317-1782/2018201714329898038 [Google Scholar] [CrossRef] [PubMed]
[9]. Yang LY, Lee BO, Lee KN, Chen CA, Effects of electrical stimulation of acupoints on xerostomia for patients who undergo hemodialysisHealthcare (Basel) 2022 10(3):49810.3390/healthcare1003049835326976 [Google Scholar] [CrossRef] [PubMed]
[10]. More CB, Gupta S, Joshi J, Varma SN, Classification system for oral submucous fibrosisJournal of Indian Academy of Oral Medicine and Radiology 2012 24(1):2410.5005/jp-journals-10011-1254 [Google Scholar] [CrossRef]
[11]. Thomson WM, Measuring change in dry-mouth symptoms over time using the Xerostomia InventoryGerodontology 2007 24(1):30-35.10.1111/j.1741-2358.2007.00137.x17302928 [Google Scholar] [CrossRef] [PubMed]
[12]. Brott NR, Zeppieri M, Ronquillo Y, Schirmer TestIn: StatPearls [Internet] 2024 Jan Treasure Island (FL)StatPearls Publishing[Updated 2024 Feb 24]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559159/ [Google Scholar]
[13]. Schoppmeier CM, Helpap J, Hagemeier A, Wicht MJ, Barbe AG, Using the modified Schirmer test for dry mouth assessment: A cross-sectional studyEuropean Journal of Oral Sciences 2022 130(4):e1288010.1111/eos.1288035692181 [Google Scholar] [CrossRef] [PubMed]