Tuberculosis, triggered by the bacterium Mycobacterium tuberculosis, is a widely recognised infectious disease that can affect any part of the body [1]. The World Health Organisation (WHO) consistently describes it as a major global health problem. Because it is a highly contagious disease, one person with an active TB infection can spread the infection to 5-15 people in close contact each year. According to the WHO, tuberculosis is the 13th leading cause of death worldwide [2]. In 2021, an international survey of recent tuberculosis cases found that India was the largest contributor among ten countries. The lungs are the primary organs affected by tuberculosis, which is commonly presented as a pulmonary complaint. Numerous diagnostic procedures with high sensitivity and specificity are available to detect pulmonary tuberculosis. An organ other than the lungs affected by tuberculosis is referred to as EPTB. During the primary infection, Mycobacterium invades other organs besides the lungs, but remains dormant in an immunocompetent individual. As the host immune response decreases, reactivation of the latent infection occurs [3].
The spectrum of clinical presentation of EPTB is similar to that of other diseases, which delays diagnosis and increases morbidity. The etiology may be due to reactivation of a latent TB infection or reinfection in an endemic location [4]. EPTB can manifest clinically as fever, Pyrexia of Unknown Origin (PUO), infertility, dysmenorrhea, bacterial infections, anemia, or even as a neoplasm by infecting almost all organs of the body [5]. What we diagnose as EPTB is just the tip of the iceberg. Clinicians take great care to correctly diagnose EPTB because the disease has a non specific appearance and is paucibacillary in nature, presenting diagnostic challenges when collecting clinical samples from deeply infected organs [6]. Furthermore, EPTB cases are resistant to therapy because the appropriate drug concentration is not achieved in the affected area. In contrast, cases of pulmonary tuberculosis are easily recognised based on radiological changes in the lungs and the detection of AFB in sputum.
The cytological and histological procedures routinely performed show granulomas but cannot distinguish them from other causes such as fungal infections, sarcoidosis, foreign bodies, and immune granulomas. In order to diagnose a mycobacterial infection, isolation of the bacteria is essential [7]. However, the isolation of tuberculosis bacteria depends on many factors, including the stage of the disease, the type of organ affected, and the immune status of the host [8]. Nowadays, EPTB, which affects rare sites, can be diagnosed through advanced laboratory diagnostics that are not available in all peripheral regions of a developing country like India [9].
The AFB detection method is the simplest and fastest laboratory method recommended by the WHO and is routinely used to diagnose pulmonary tuberculosis. However, the effectiveness of this method is drastically reduced in cases of EPTB because the samples are paucibacillary in nature. Although mycobacterial culture is considered the gold standard, it has some limitations, as it is time-consuming and difficult to establish a culture in peripheral laboratories. Additionally, the isolation of bacteria varies in all EPTB samples [10].
The Gene Xpert Mycobacterium Tuberculosis (MTB)/Rifampicin (RIF) automated molecular assay Ultra (Cepheid), also known as CBNAAT, is a rapid diagnostic method recommended by the WHO to identify the Deoxyribose Nucleic Acid (DNA) of mycobacteria and also rifampicin-resistant variants in all types of Pulmonary Tuberculosis (PTB) and EPTB samples. It has high sensitivity with minimal laboratory risk in handling the samples [11,12]. The limitation of this test is that it requires frequent calibration and is expensive. Given the diagnostic limitations of each test for diagnosing EPTB, a combined approach utilising all tests can be performed in a resource-limited laboratory. A CRS can be used to diagnose extrapulmonary tuberculosis according to the literature, where bacterial isolation by AFB or CBNAAT, along with necrotising granuloma, is considered CRS positive [13].
Since the prevalence and incidence of PTB and EPTB cases are high in Mayurbhanj district, Odisha, India, at 268 cases per lakh per year [14,15], the aim of the present study was to highlight unexpected atypical presentations of tuberculosis and compare different diagnostic methods. The primary objective of the study was to observe the diversity in the clinical presentation of TB, while the secondary objective was to assess the efficacy of different diagnostic methods in comparison to CRS as the gold standard.
Materials and Methods
The present study is a cross-sectional observational study conducted in the Department of Pathology and Microbiology, PRM Medical College and Hospital (in the tuberculosis endemic zone of Baripada), North Odisha, India, from April 2018 to November 2022. The study was carried out after obtaining approval from the Research Ethics Committee (Ref No.-10/Dt 29/05/2019). This medical college, located in the northern part of Odisha, serves as a referral centre for many primary healthcare facilities. Patients with EPTB presented to Outpatient Departments such as Medicine, Surgery, Pulmonary Medicine, Dermatology, and Obstetrics and Gynaecology with complaints of fever, glandular swellings of the head and neck, altered bladder and bowel habits, disturbed menstrual cycles and infertility.
Inclusion criteria: All patients of all age groups suspected of having a tubercular infection, both pulmonary and extrapulmonary, were included in the study.
Exclusion criteria: Patients currently undergoing anti-tubercular treatment, those with malignancies, other infections, non co-operative patients, and those with serious co-morbidities were excluded from the study.
Study Procedure
Written informed consent was obtained from all patients. A total of 400 cases of both PTB and EPTB were collected for pathological diagnosis and microbiological confirmation. Demographic data, clinical history, PPD skin tests, and relevant laboratory and radiological results were collected from medical records. Clinicians referred suspected cases of tubercular infection for Fine Needle Aspiration Cytology (FNAC) and excised specimens for histopathological examination. Initially, 278 cases of FNAC and 122 cases of biopsy were diagnosed as tubercular infections. For microbiological confirmation, all 400 cases were processed for AFB staining and CBNAAT determination.
Cytology: Patients presenting with various swellings and non healing ulcers with scars were examined in the cytology laboratory. After proper aseptic procedures, the swellings were aspirated using a 22 gauge needle with an aspirator. The aspirated material was divided into three parts. One part was sent in a sterile cartridge container for molecular detection of mycobacteria to an intermediate reference laboratory, following the manufacturer’s instructions. The second part was expelled onto a slide, and a smear of adequate thickness was prepared using a spreader slide. The smears were fixed with methanol. The air-dried and wet-fixed smears were stained with Giemsa and Haematoxylin and Eosin (H&E) stains, respectively. Cytomorphological classification of the smears was performed based on the presence of granuloma and caseous necrosis. Type I had granuloma without necrosis, type II had caseous necrosis with epithelioid granuloma and type III exhibited extensive caseous necrosis without definite granuloma. AFB staining was performed on the third part of the material on an air-dried smear [16].
Histology: The surgically resected biopsy specimens were fixed in 10% neutral buffered formalin for paraffin embedding. The paraffin blocks were placed on an ice-cold plate. Initially, all the blocks were trimmed. Sections of 4 μ in thickness were collected for routine H&E staining and ZN staining. Additionally, CT-guided core biopsy samples of suspected nodular and cavitary lung lesions, as well as miliary lesions in other organs, were also processed.
CBNAAT: Cytological aspirates were sent to the laboratory in a sterile cartridge for nucleic acid amplification. In the paraffin blocks, deparaffinisation was performed using xylene, followed by rinsing in ethanol and buffered saline. The tissue was homogenised by adding proteinase K, and DNA extraction was carried out. According to the manufacturer’s instructions for the Cepheid GeneXpert® MTB/RIF system, GeneXpert reagent was added to the tissue homogenate and allowed to settle for 15 minutes in a cartridge. The cartridge was then placed in the designated chamber of the Cepheid machine, and the barcode was scanned. After automatic filtration and washing, the microorganisms present in the sample were lysed, releasing the DNA. PCR reagent was added to the extracted DNA of the tuberculosis bacteria. Amplification of the TB nucleic acid was performed using hemi-nested PCR, and target sequencing of the TB genome was obtained as a result [17].
AFB stain: Cytological samples and received sputum materials were stained with an acid-fast stain. The ZN-stained slides were examined under oil immersion at 1000x magnification. Biopsies with necrotising granulomas were stained with conventional ZN stain. After adjusting to the water level, slides were stained with hot carbol fuchsin for 45 seconds. Following this, the slides were washed in running tap water, and 25% sulfuric acid was applied to the slides and allowed to stand for 2-4 minutes. The slides were then gently rinsed with tap water, and 0.1% methylene blue was applied for 30 seconds for counterstaining [8].
Composite Reference Standard (CRS): Since the culture facility was unavailable at the present study Institute, CRS was considered positive (gold standard) when bacterial isolation was confirmed either by AFB stain or by CBNAAT, along with the observation of caseating granuloma in the pathological examination [18]. The authors have classified all the cases into two categories: CRSa and CRSb for analysing, FNAC and biopsy cases separately. CRSa included TB-positive cases identified by AFB stain and/or CBNAAT, accompanied by necrotising granuloma in FNAC, whereas CRSb comprised TB-positive cases identified by AFB stain and/or CBNAAT, with histomorphology demonstrating well-formed granuloma with caseous necrosis [16]. All tests were compared with the reference standard to measure their diagnostic accuracy.
Statistical Analysis
The data analysis was conducted using the Statistical Package for Social Sciences (SPSS) software, version 23.0. To assess the diagnostic utility of different tests, sensitivity, specificity, positive predictive value and negative predictive value, along with their 95% confidence intervals, were calculated using GraphPad Prism 5.0 software. For comparison, McNemar’s test was performed, and a p-value of less than 0.05 was considered statistically significant for all statistical analysis.
Results
A total of 400 cases of EPTB and, combined PTB and EPTB were studied during the specified period, involving all age groups (1-74 years). The analysis revealed a male-to-female ratio of 1:1.02, indicating that more females than males over the age of 20 years were affected. Pulmonary tuberculosis cases numbered 39 (9.75%), while extrapulmonary TB cases totaled 361 (90.25%). Both cytological aspirations (n=278) and biopsy specimens (n=122) were received. In the 0-20 years age group, males were more affected, whereas above the age of 20 years, a female preponderance was observed, with female patients (n=202) outnumbering male patients (n=198) [Table/Fig-1].
Demographic data of PTB and EPTB (N=400).
| Parameters | PTB (n=39)n (%) | EPTB (n=361)n (%) |
|---|
| Gender |
| Male | 22 (56.41) | 176 (48.75) |
| Female | 17 (43.58) | 185 (51.24) |
| Age group (years) |
| 0-20 | 03 (7.69) | 86 (23.82) |
| 21-40 | 18 (46.15) | 137 (37.95) |
| 41-60 | 15 (38.46) | 117 (32.40) |
| >60 | 03 (7.69) | 21 (5.81) |
| Cytology +ve | 18 (46.15) | 148 (40.99) |
| Histology +ve | 27 (69.23) | 58 (7.47) |
| AFB +ve | 3 (7.69) | 58 (7.47) |
| CBNAAT +ve | 34 (87.17) | 221 (61.21) |
| CRS +ve | 37 (94.87) | 261 (72.29) |
*Differences between the two groups for none of the variables were found significant
Clinically, the initial impression was EPTB in 172 (47.64%) cases. The remaining cases were misdiagnosed as other bacterial infections, 78 (21.6%), chronic inflammatory lesions, 93 (25.76%), and neoplastic lesions, 18 (4.98%) [Table/Fig-2]. The initial clinical diagnosis included inflammatory lesions in organs such as joints, breast, eyelid and axillary lymph nodes. Diagnosis of tuberculosis was confirmed through FNAC and biopsy, followed by a CBNAAT test.
Initial clinical impression of EPTB (n=361).
| Tuberculosis (EPTB) | Inflammatory lesion | Bacterial infection | Malignancy |
|---|
| 172 (47.64%) | 93 (25.76%) | 78 (21.6%) | 18 (4.98%) |
Values presented as n (%)
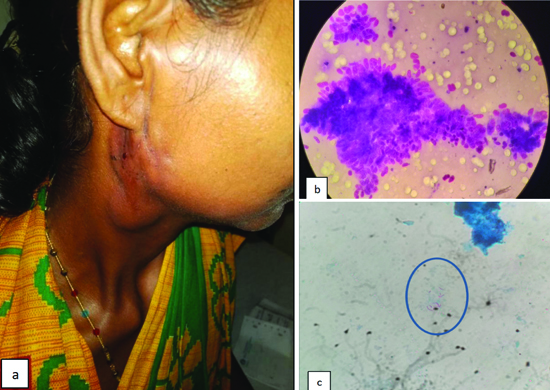
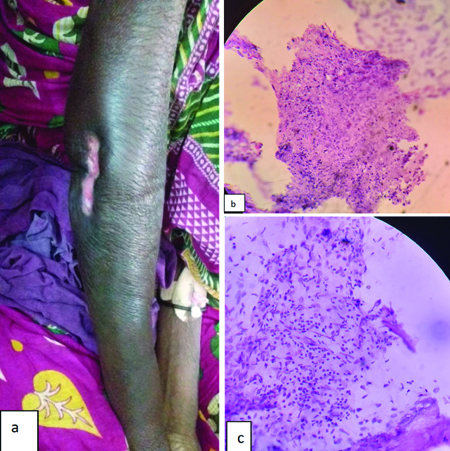
The most affected sites were lymph nodes, 134 (33.5%), followed by bones, 64 (16%). The cervical group of lymph nodes was the most commonly affected, 73 (18.25%), followed by the axillary group, 48 (12%) [Table/Fig-3]. In [Table/Fig-4], a female presented with a discharging sinus involving the upper cervical group of lymph nodes [Table/Fig-4a]. Cytosmears demonstrated granuloma [Table/Fig-4b] and the AFB stain revealed rod-shaped, curved bacilli [Table/Fig-4c].
Distribution of tuberculosis according to various sites.
| Organs | Number of cases (n) | Percentage(%) |
|---|
| Lymph nodes (n=134) | Cervical | 73 | 18.25 |
| Axillary | 48 | 12 |
| Mediastinum | 03 | 0.75 |
| Inguinal | 03 | 0.75 |
| Paratracheal | 02 | 0.5 |
| Supraclavicular | 05 | 1.25 |
| Bone and joints (n=64) | Hip | 11 | 2.75 |
| Elbow | 10 | 2.5 |
| Knee | 27 | 6.75 |
| Femur | 9 | 2.25 |
| Wrist | 7 | 1.75 |
| Omentum | 13 | 3.25 |
| Small intestine | 19 | 4.75 |
| Liver | 2 | 0.5 |
| Breast | 9 | 2.25 |
| Soft-tissue | 61 | 15.25 |
| Lungs | 39 | 9.75 |
| Epiglottis | 5 | 1.25 |
| Periorbital | 2 | 0.5 |
| Testis | 11 | 2.75 |
| Endometrium | 9 | 2.25 |
| Cervix | 7 | 1.75 |
| Ovary | 9 | 2.25 |
| Fallopian tube | 9 | 2.25 |
| Central nervous system | 7 | 1.75 |
| Total | 400 | 100 |
a) Right upper cervical adenitis with discharging sinus; b) Cytosmear demonstrates clusters of epithelioid cells (H&E, 1000x); c) Z-N stain demonstrates rod shaped, curved Acid Fast Bacilli (AFB, 1000x).
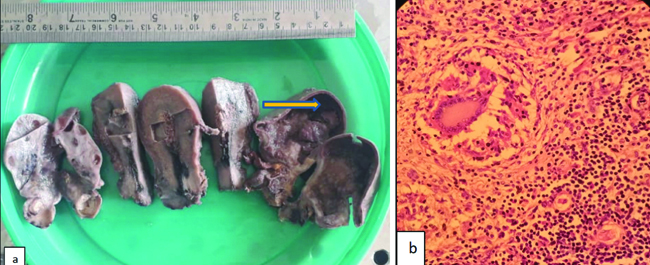
Pulmonary involvement was 39 (9.75%) cases. Among bone lesions, EPTB involving the knee joint was the most common, 27 (6.75%), followed by the hip joint, 11 (2.75%). In terms of EPTB infection in reproductive organs, the order of prevalence was as follows: testis (n=11, 2.75%), endometrium, ovary and fallopian tube {each, 9 (2.25%)}, and cervix (1.75%). A clinically diagnosed tubo-ovarian mass was received, where the uterus, cervix and bilateral appendages were identified. The right ovary was cystically dilated, and its contents resembled dirty, caseous material [Table/Fig-5a]. The microscopic photograph in [Table/Fig-5b] demonstrated granuloma with classical Langhans-type giant cells.
a) Cut-section of uterus, cervix and bilateral appendages. Right ovary was cystically dilated and filled with dirty caseous material (arrow); b) Granuloma with Langhans type of giant cell (H&E, 400x).
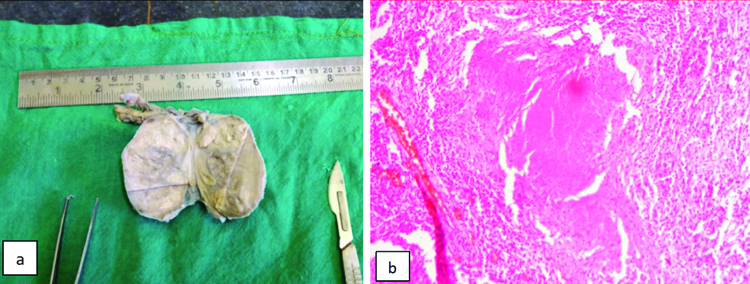
Tuberculosis affecting the testis in a 40-year-old male presented with scrotal swelling. An orchidectomy specimen was received, and the cut section showed multiple whitish necrotic areas [Table/Fig-6a]. Caseous necrosis with granuloma was evident upon histopathological examination [Table/Fig-6b].
a) Testis on cut-section shows homogenous yellowish white with focal necrotic areas; b) Granuloma shows central caseating necrosis (H&E, 200x).
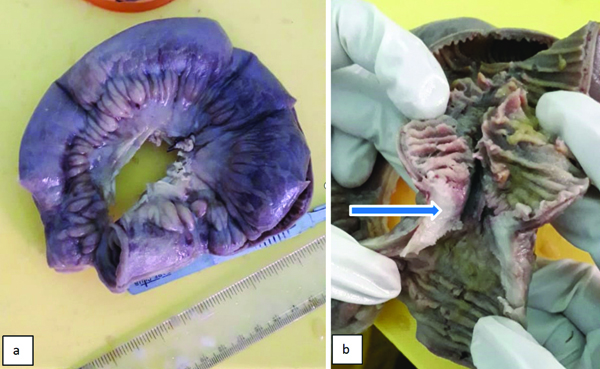
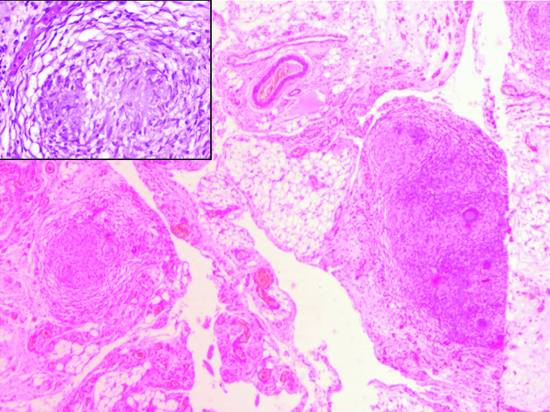
Small intestinal tuberculosis presented as obstruction and ulcers in (3.25%) cases, followed by omental tuberculosis in 13 cases. [Table/Fig-7a] demonstrates a part of the small intestine measuring 32 cm × 2.5 cm. There was a constricted section 4 cm away from one end, and the cut section revealed a whitish nodule measuring 1×1 cm [Table/Fig-7b]. The attached omentum measured 5×4 cm. Omental fatty tissue showed granulomatous foci containing multinucleated giant cells and clusters of epithelioid cells [Table/Fig-8].
Small intestine segment showing transverse stricture 4 cm away from one end.
Section of omentum demonstrates granuloma (H&E, 50x). Inset shows cluster of epithelioid cells (H&E, 200x).
Tubercular infection involving the chest wall with sinus formation was diagnosed in a one-year-old male child. In [Table/Fig-9a], a 50-year-old female exhibited swelling and an ulcer on the lateral aspect of the right elbow joint for four months. Clinically, TB osteomyelitis was suspected. A minute tissue sample was received, and microscopy demonstrated dead bone [Table/Fig-9b], necrosis, along with tubercular granuloma [Table/Fig-9c]. The CBNAAT of the tissue confirmed the disease as tubercular in origin. Periorbital structures were also affected by EPTB, accounting for 0.5% of cases. Miliary tuberculosis was observed in three cases.
a) An ulcer over lateral aspect of right elbow joint; b) Photomicrograph shows dead bone (H&E, 50x); c) Granuloma and epithelioid cell clusters (H&E, 100x).
A total of 278 cytology samples were diagnosed as tubercular granuloma, out of which the maximum number of cases (59.7%) showed a type II pattern with caseating necrosis and granuloma. Type III, characterised by extensive necrosis, was seen in 27.3% of cases [Table/Fig-10]. Out of 122 biopsy cases, typical necrotising granuloma was identified in 69.6% of cases, while only granuloma was observed in 19.6% of cases. Suppurative infection was also noted in 4.09% of cases. In all cytology and biopsy samples, the CBNAAT test returned positive in 63.75% of cases, and AFB stains were positive in 15.25%.
Pathological patterns of inflammation in histopathology and cytopathology.
| Histological patterns (n=122) | n (%) | Cytological patterns (n=278), n (%) |
|---|
| Necrotising granulomatous inflammation | 85 (69.6) | Type I (Granuloma without necrosis) | 36 | 13% |
| Granulomatous inflammation | 24 (19.6) | Type II (Caseous necrosis with granuloma) | 166 | 59.7% |
| Suppurative lesion | 5 (4.09) | Type III (Extensive caseous necrosis only) | 76 | 27.3% |
| Chronic inflammation | 3 (2.4) | - | - | - |
| Necrotising inflammation | 5 (4.09) | - | - | - |
Out of a total of 400 samples, CRS was positive in 298 cases. In the 278 positive cytology cases, CRSa positivity was seen in 230 cases. Similarly, in biopsy samples, 68 cases were CRSb positive [Table/Fig-11].
Different investigation methods and Composite Reference Standard (CRS).
| Type of test | Diagnosed as tuberculosis, n (%) | CRS (Positive), n (%) |
|---|
| FNAC (n=278) | 166 (59.71%) | (CRSa) 230 (82.73%) |
| Biopsy (n=122) | 85 (69.67%) | (CRSb) 68 (55.73%) |
| CBNAAT (n=400) | 255 (63.75%) | 298 (74.5%) |
| AFB (n=400) | 61 (15.25%) | 298 (74.5%) |
The CBNAAT test demonstrated the highest diagnostic accuracy (92.8%) among all four tests, whereas the highest sensitivity was observed in the histopathological method, followed by CBNAAT (85.6%). The FNAC method showed a sensitivity of 72.2%, while the AFB staining method yielded disappointing results (20.5%) [Table/Fig-12].
Diagnostic accuracy of AFB, FNAC, biopsy and CBNAAT compared to gold standard reference (CRS).
| CRS vs test | Observation | CRS | Sensitivity | Specificity | PPV | NPV | Accuracy | Kappa co-efficient | p-value |
|---|
| Positive | Negative |
|---|
| CRS a vs FNAC | Positive | 166 | 0 | 72.2 | 100 | 100 | 42.9 | 86.1 | 0.719 | <0.001* |
| Negative | 64 | 48 |
| CRS b vs Biopsy | Positive | 68 | 17 | 100 | 68.52 | 80 | 100 | 86.07 | 0.3663 | <0.001* |
| Negative | 0 | 37 |
| CRS vs CBNAAT | Positive | 255 | 0 | 85.6 | 100 | 100 | 100 | 92.8 | 0.9102 | <0.001* |
| Negative | 43 | 102 |
| CRS vs AFB | Positive | 61 | 0 | 20.5 | 100 | 100 | 30.1 | 60.2 | 0.8682 | <0.001* |
| Negative | 237 | 102 |
McNemar’s test; *The p-value <0.05 was considered statistically significant
Discussion
Though the pathology, pathogenesis, natural history and course of the disease are well established, it remains a major global health issue. Clinically, 47.64% of cases suspected of TB infection were correctly diagnosed. General symptoms like fever, malaise and weight loss were initially misdiagnosed as chronic inflammatory conditions or bacterial infections. Gastrointestinal tuberculosis presented as adhesions, obstructions and weight loss. Yoon HJ et al., reported TB infection in their study as the initial clinical impression in 67.8% of cases [6]. In the present study, the clinical presentation of EPTB affected the lymph nodes in the maximum number of cases (33.5%), followed by the osteoarticular system (16%), gastrointestinal tract, soft tissue, reproductive organs, breast and CNS. Similar to the current study, Sunnetcioglu A et al., reported lymph nodes (39.4%) as the most common EPTB site, followed by the pleura, peritoneum and bone (7.4%) [19]. In another study by Njau AN et al., lymph node involvement was 38%, followed by the female genital system (19%) and abdominal tissue (13.9%) [20]. Guler SA et al., also highlighted the lymph node as the most common site of EPTB (12%), followed by the pleura (10.8%) [3].
Earlier studies on EPTB have shown an increased predilection for women in the age group of 20 years and above [3,19,20]. Male preponderance was observed below 20 years. In contrast, pulmonary TB cases were observed more frequently in males, which may be explained by smoking habits. Females were mostly affected by EPTB, possibly due to low living standards, unawareness of the initial symptoms, and inaccessibility to healthcare facilities in this northern Odisha population.
Necrotising granuloma observed in Type II (59.7%) cytomorphological patterns and histological examinations of necrotising granuloma (69.6%) were considered as confirmed TB. Secondary infections of these granulomas containing neutrophils were observed in 4% of cases. A low immune host response usually results in suppurative inflammation [21]. Similar observations were reported by Ahmed HGE et al., with 68% of necrotising granulomas [22]. Almobarak AO et al., documented that 88.3% of smears demonstrated caseating granulomas along with suppurative inflammation [23].
The diagnostic utility of four tests- FNAC, biopsy, CBNAAT and AFB stain was analysed in comparison to the gold standard, CRS. Although the culture test is always considered the gold standard for diagnosing TB infection, its sensitivity is low in the case of EPTB specimens. This can be explained by the absence of viable bacilli [24,25]. The invention of newer molecular detection techniques, such as GeneXpert MTB/RIF Ultra, allows for the detection of DNA from dead bacteria and from paucibacillary tissue, with high sensitivity even in culture-negative samples. The AFB detection method had the lowest diagnostic accuracy (20.5%). A similar observation was documented by Polepole P et al., who reported a sensitivity of 94% [17].
The CBNAAT method detects only the Mycobacterium tuberculosis complex, while AFB stains highlight TB bacilli, as well as, non TB bacilli, which can create a false positive impression in TB-endemic regions. Additionally, the ZN stain exhibited the lowest sensitivity in tissue biopsies in other studies, as well [26]. The sensitivity of the Xpert MTB/RIF CBNAAT method was found to be lower (85.6%) compared to histologically confirmed cases. The presence of caseating granuloma in histopathology may be observed even after the degeneration of bacilli, as cellular changes have already occurred. However, CBNAAT detects these cases as negative, as it only identifies viable DNA material of Mycobacterium tuberculosis. Polepole P et al., found the sensitivity of the Xpert MTB/RIF assay to be 30% and the PCR assay to be 42%. The yield of Mycobacterium tuberculosis in fresh biopsy specimens is higher than that in paraffin-embedded tissues [17].
The efficiency of the Xpert MTB/RIF assay in EPTB was highest in lymph node samples, while moderate positivity was observed in tubercular meningitis [27]. A study by Uddin MKM et al., concluded that the Xpert MTB/RIF assay had a diagnostic accuracy of 83.7% when compared to CRS [28]. Similar results for the Xpert MTB method were reported, ranging from 87.3-95% in other studies [27-29]. The sensitivity of Xpert/MTB varies according to the type of specimen. Interferon gamma (IFN-γ) release assays and Adenosine Deaminase (ADA) assays are some useful additional tests in CBNAAT-negative samples [16].
Limitation(s)
The present study was conducted based on laboratory detection methods, which may not truly reflect the prevalence of the disease and the disease status in the population. The immune status of all the patients was not available in the records. Additionally, the extraction of DNA material from formalin-fixed old tissues was variable, as it depends on the time of fixation of the sample and the strength of formalin used. Histopathology alone cannot differentiate between tubercular and non tubercular granulomas; confirmation by an additional method of bacilli isolation is necessary.
Conclusion(s)
Considering tuberculosis as a major public health problem, the diagnosis is of utmost importance. Since no single test is perfect for accurately diagnosing EPTB, a combination of tests is necessary to increase sensitivity and specificity. Clinical insight, along with a couple of diagnostic methods, will definitely raise the number of EPTB cases identified in endemic regions with resource-limited laboratories.
*Differences between the two groups for none of the variables were found significant
Values presented as n (%)
McNemar’s test; *The p-value <0.05 was considered statistically significant