The breasts are paired glands of variable size and density that lie superficial to the pectoralis major muscle [1]. A lump or mass in the breast is a source of worry or anxiety, particularly for female patients of all age groups, and it sometimes produces diagnostic difficulties for both clinicians and pathologists [2]. In most nations, benign breast conditions account for 10 times more cases of breast problems in women than breast cancer [3]. Benign breast diseases are often considered aberrations of normal development and involution [4]. Benign pathology is depicted in almost 80% of breast biopsies [5]. Up to 30% of women suffer from a benign breast disorder that requires treatment [6]. A standard method for evaluating breast lumps is the triple assessment, which consists of clinical examination, radiographic imaging, and pathological assessment via core or excision biopsy [7]. In diagnostic breast pathology, distinguishing between benign and malignant lesions is usually straightforward, with well-defined criteria for malignancy. However, some tumours exhibit ambiguous features that fall between benign and malignant, complicating diagnosis and treatment [8]. Borderline breast lesions are a diverse set of non cancerous breast lesions that have a higher risk of developing cancer in the future and have the potential to be upstaged to malignancy during surgery [9].
Choosing the best course of action for a borderline lesion for which a definitive diagnosis of benign or malignant cannot be made can be difficult. The same lesion may be treated differently at different centres or even in the same centre when managed by different doctors. This uncertainty could lead to over-treatment or under-treatment. The risk associated with a particular lesion and awareness of the advantages of action should form the basis of management plans [8]. The main objective of the study was to determine the overall prevalence of benign and borderline breast lesions in the Vindhya region, where, with limited resources, histopathology plays a crucial role in diagnosis. This way, early and appropriate management strategies can be implemented, subsequently improving patient outcomes.
Materials and Methods
The present cross-sectional study was conducted in the Department of Pathology at Shyam Shah Medical College, Rewa, Madhya Pradesh, India from January 2019 to December 2023, comprising a total of 831 cases of breast lesions. Ethical clearance was not required or was waived for this cross-sectional study since it involved pathological specimens. Additionally, no patient data were disclosed.
Inclusion criteria: All lumpectomy and wedge biopsy specimens of breast lesions sent from the Department of Surgery, submitted in properly labeled containers filled with 10% formalin, along with duly filled histopathology requisition forms containing details of the patient’s age, sex, and laterality of the lesion, only benign and borderline lesions (all those lesions that have a higher risk of developing into invasive lesions) were included in the study.
Exclusion criteria: Patients with incomplete demographic information and specimens sent without 10% formalin in the container, or samples sent in containers filled with normal saline, were excluded from the study.
Study Procedure
In each case, data was collected from the requisition forms, including age, sex, duration, laterality of the lesion, signs and symptoms, and significant clinical history. A detailed gross examination of the breast specimens was conducted. Sections of the specimens were taken, followed by processing and embedding in paraffin wax. The sections were cut to a thickness of 5 μm. H&E staining was performed on the sections. The histopathological typing of lesions was conducted, and HPE reports were recorded as benign, borderline, and malignant lesions.
Statistical Analysis
The data collected was entered into Microsoft® Excel® 2019 MSO (Version 2407 Build 16.0.17830.20056) 64-bit, and the descriptive data were expressed as numbers, percentages, and means.
Results
A total of 831 breast lesions were analysed, out of these, 640 (77.0%) cases were benign breast lesions, 15 (1.8%) were borderline lesions, and 176 (21.2%) cases were malignant lesions. There were 631 (96.3%) females and 24 (3.7%) males out of a total of 655 lesions, including benign and borderline breast lesions. The age of the patients ranged from 14 years to 57 years for the benign and borderline breast lesions, with the mean age for benign breast lesions being 27.3 years, while the mean age for borderline lesions was 44.5 years. Involvement of the left-side of the breast was more common, with a frequency of 334 (51%) cases, right breast involvement was seen in 293 (44.7%) cases, and 28 (4.3%) cases involved bilateral breast.
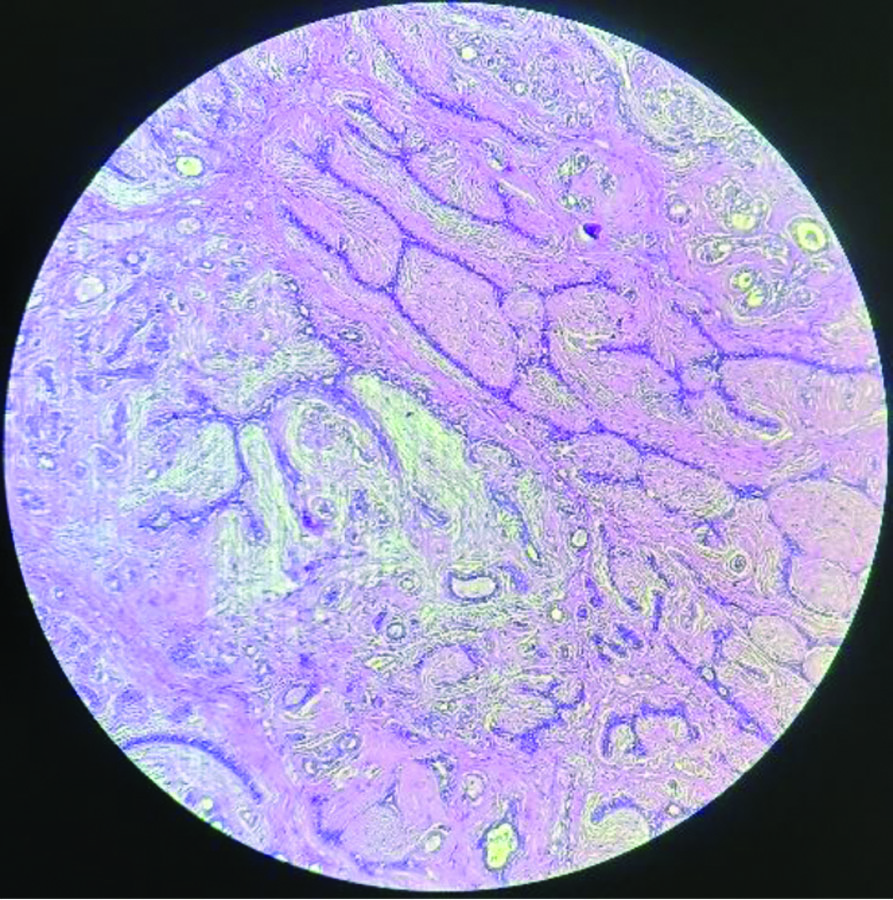
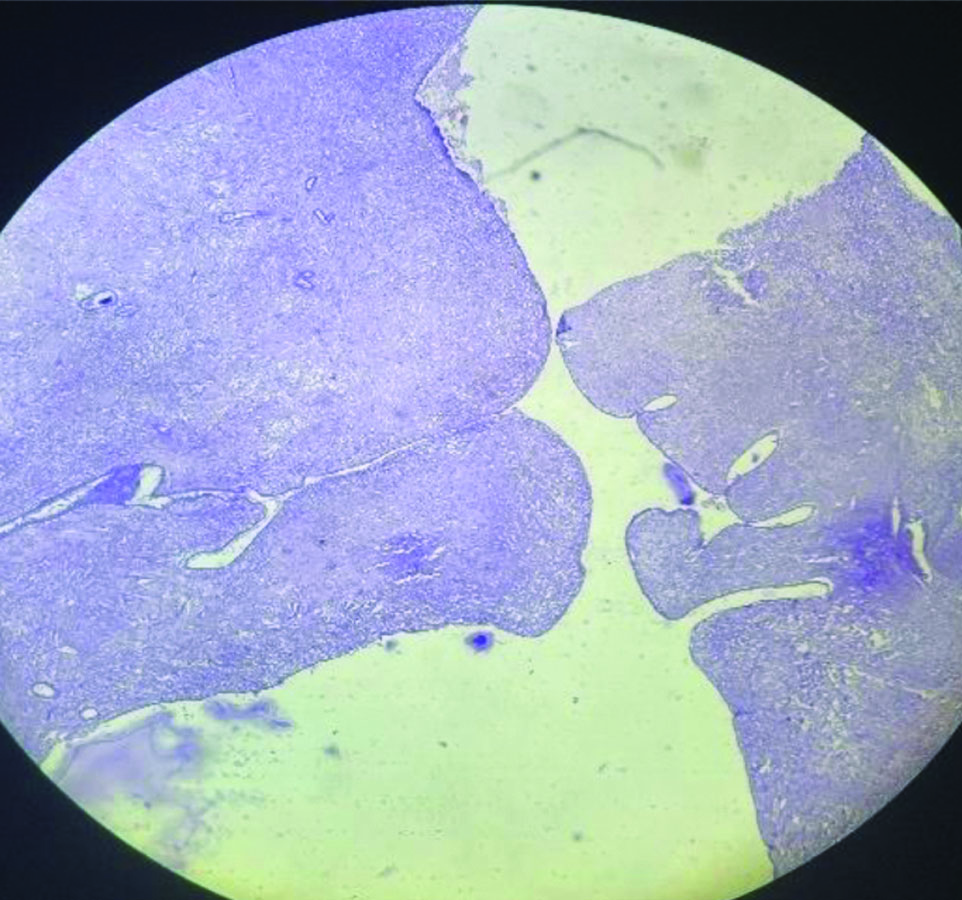
Fibroadenoma was the most common lesion among females, with 419 (50.4%) cases out of all the lesions, constituting 65.5% of all benign lesions (the total benign lesions were 640). Most of the lesions involved the unilateral breast, with a more common involvement of the left breast. The mean age for fibroadenoma was 21.4 years. The mass lesions ranged from 0.5 cm to 5.5 cm, with the cut surface showing slit-like spaces. The microscopy was characterised by varying degrees of overgrowth of both stromal and epithelial components [Table/Fig-1].
Fibroadenoma breast (H&E, 10x).
Among males, gynaecomastia was the most common breast lesion, constituting 21 (2.5%) cases of total lesions and 3.2% of all benign lesions. There was frequent involvement of the left breast, with the most common presentation occurring in the age group between 15 years to 25 years, and the mean age being 17 years. Grossly, the masses were well-circumscribed with firm consistency, and microscopy revealed the ducts exhibiting epithelial hyperplasia of varying degrees, encased by a significant proliferation of the surrounding stroma.
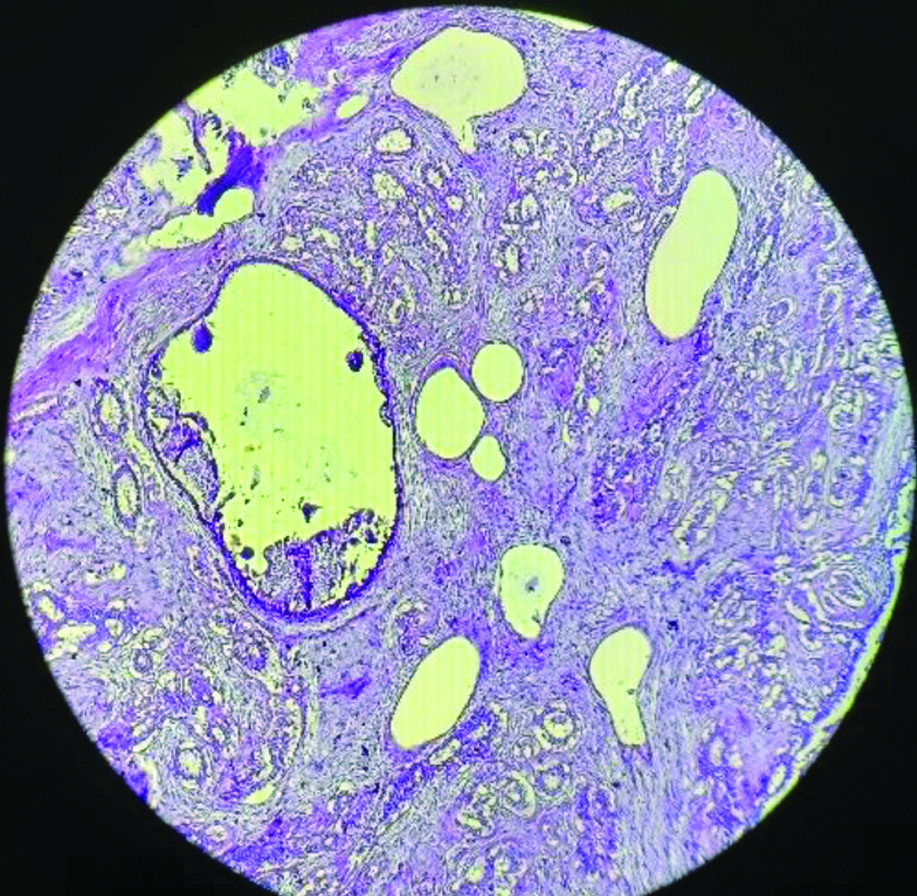
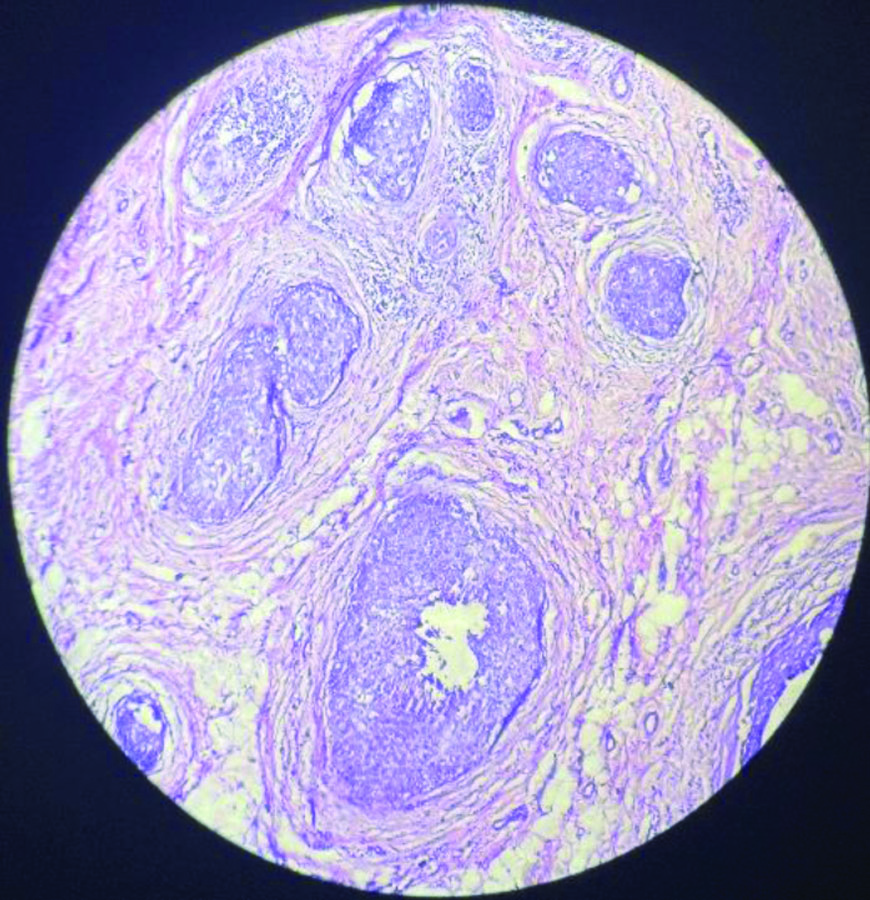
The second most common breast lesion was fibrocystic disease of the breast, with a total of 148 cases (17.8%) among all benign, borderline, and malignant lesions. The ages ranged from 27 to 50 years, with a mean age of 33.5 years. Grossly, the tumours were firm and fibrosed, with the cut surface showing cysts measuring from 0.2 to 1.5 cm. Microscopy revealed cystic dilatation of the glands, with the presence or absence of eosinophilic secretions inside the dilated glands and the surrounding fibrosed stroma [Table/Fig-2].
Fibrocystic disease of breast (H&E, 10x).
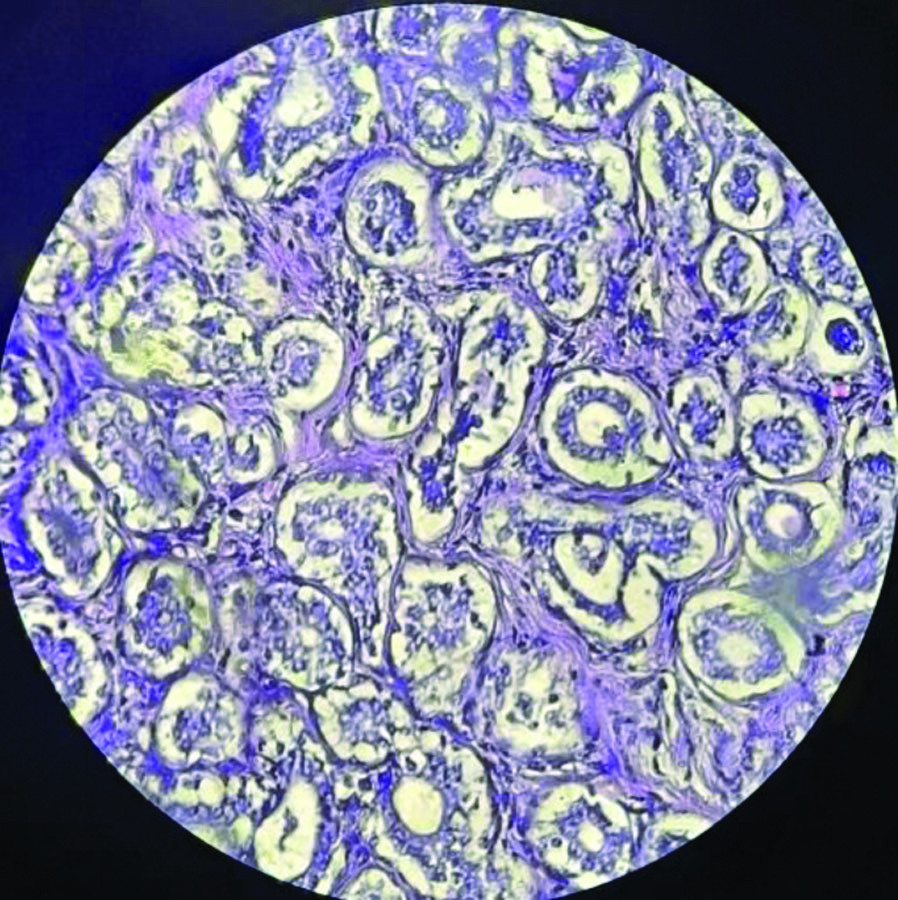
Among other benign breast lesions, there were 21 cases (2.5%) of inflammatory breast diseases, which included 10 cases of chronic mastitis, five cases of granulomatous mastitis, three cases of breast abscess, two cases of necrotising mastitis, and one case of acute suppurative mastitis. There were eight cases of microglandular adenosis, seven cases of each tubular adenoma [Table/Fig-3] and sclerosing adenosis [Table/Fig-4], four cases of benign phyllodes tumour [Table/Fig-5], and two cases of lactational adenoma. Additionally, there were two cases (0.3%) of lipoma and one case (0.15%) of hamartoma. The detailed distribution of all the benign lesions is presented in [Table/Fig-6].
Tubular adenoma of breast (H&E,40x).
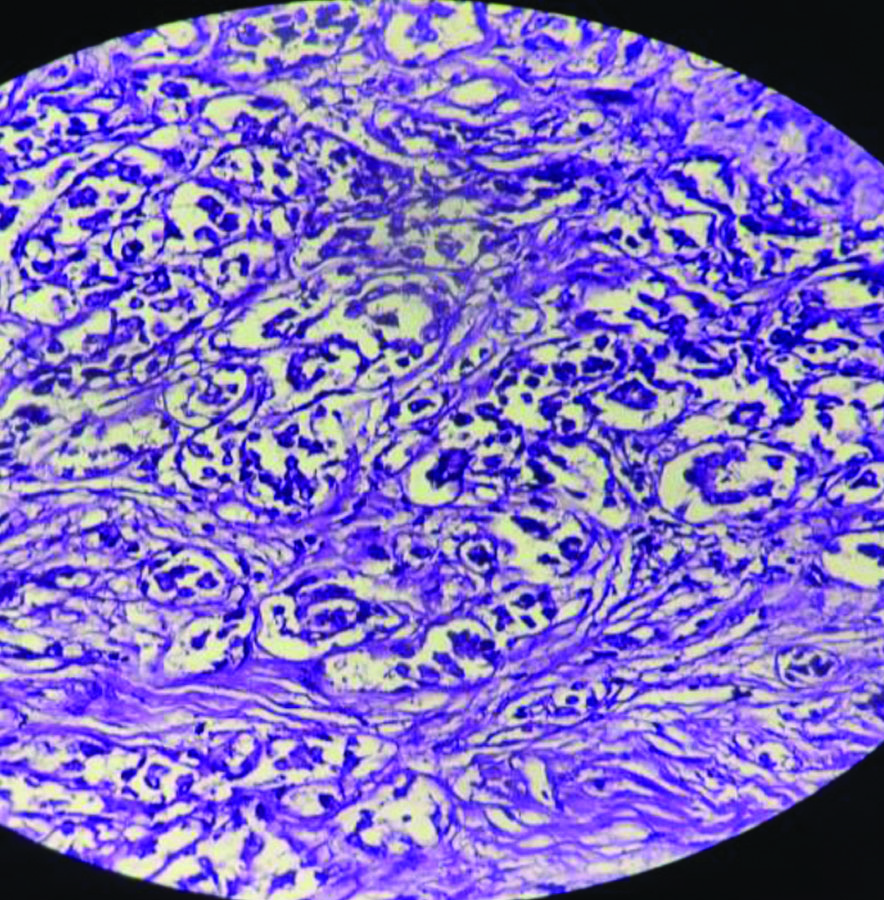
Benign phyllodes (H&E,4x).
Distribution of benign breast lesions by age.
| Age (years)Lesions | 11-20 | 21-30 | 31-40 | 41-50 | 51-60 | Total | Sex distribution, n (%) | Percentage among TLS | Percentage among BLS | Mean age (years) |
|---|
| Female | Male |
|---|
| Gynaecomastia | 9 | 7 | 4 | 1 | 0 | 21 | 0 | 21 (100) | 2.5 | 3.2 | 17 |
| Inflammatory conditions | 5 | 10 | 6 | 0 | 0 | 21 | 20 (95.2) | 1 (4.8) | 2.5 | 3.2 | 29.2 |
| Lactational adenoma | 0 | 2 | 0 | 0 | 0 | 2 | 2 (100) | 0 | 0.24 | 0.31 | 23 |
| Fibroadenoma | 153 | 179 | 57 | 29 | 1 | 419 | 419 (100) | 0 | 50.4 | 65.4 | 21.4 |
| Sclerosing adenosis | 0 | 0 | 5 | 2 | 0 | 7 | 7 (100) | 0 | 0.84 | 1.09 | 37 |
| Microglandular adenosis | 0 | 0 | 2 | 5 | 1 | 8 | 8 (100) | 0 | 0.96 | 1.2 | 41.3 |
| Fibrocystic disease | 0 | 2 | 81 | 65 | 0 | 148 | 146 (98.6) | 2 (1.4) | 17.8 | 23.1 | 33.5 |
| Tubular adenoma | 0 | 6 | 1 | 0 | 0 | 7 | 7 (100) | 0 | 0.84 | 1.09 | 28.5 |
| Benign phyllodes | 0 | 0 | 4 | 0 | 0 | 4 | 4 (1000 | 0 | 0.48 | 0.62 | 35 |
| Others (Lipoma and Hamartoma) | 0 | 2 | 1 | 0 | 0 | 3 | 3 (100) | 0 | 0.36 | 0.46 | 22.7 |
| Total | 167 | 208 | 161 | 102 | 2 | 640 | 616 (96.25) | 24 (3.75) | | | |
TLS: Total lesions studied i.e., benign, borderline and malignant lesions; BLS: Benign lesions studied
Under the borderline category, there were a total of 15 cases, constituting nine cases (1.08%) of atypical ductal hyperplasia, three cases (0.36%) of Ductal Carcinoma In-situ (DCIS) [Table/Fig-7], two cases (0.24%) of borderline phyllodes, and one case (0.12%) with the possibility of infiltrating ductal carcinoma in a wedge biopsy from breast tissue. All the borderline lesions were exclusively identified in females [Table/Fig-8].
Ductal carcinoma in situ (H&E, 10x).
Distribution of borderline breast lesions by age.
| Age (years)Lesions | 11-20 | 21-30 | 31-40 | 41-50 | 51-60 | Total | Percentage among TLS | Mean age (years) |
|---|
| Borderline Phyllodes | 0 | 0 | 0 | 2 | 0 | 2 | 0.24 | 43.6 |
| ADH | 0 | 0 | 2 | 7 | 0 | 9 | 1.08 | 37.8 |
| DCIS | 0 | 0 | 0 | 2 | 1 | 3 | 0.36 | 51.9 |
| Possibility of IDC | 0 | 0 | 0 | 1 | 0 | 1 | 0.12 | 50 |
| Total→ | 0 | 0 | 2 | 12 | 1 | 15 | | |
TLS: Total lesions studied
Discussion
Breast lesions are the primary reason patients with breast concerns seek surgical consultation. The present study was conducted to assess the histopathological studies of breast lesions. In present study, which covered a duration of five years, benign lesions (77.0%) were more common than borderline and malignant breast lesions. This finding was comparable to the studies by Mrudula A et al., in which benign lesions constituted 78.5% [10].
In the current study, involvement of the left-side of the breast was more commonly observed, with a frequency of 334 (51%) cases compared to the right-side (44.7%) and bilateral involvement (4.3%). This conclusion was consistent with the previous study conducted by Kumbhakar D and Talukdar P which showed a higher incidence of left breast involvement at 50.76% of cases, right breast involvement at 44.31%, and bilateral involvement at 4.93% [11]. Present study found that females in the reproductive age group (14-39 years) were more commonly affected than older females, which was supported by the previous study done by Pudale S and Tonape SD [12]. Abhijit Maji A reported that the mean age at diagnosis for benign breast lesions was 28.6 years, similar to the findings of the current study, which reported a mean age of 27.3 years [13].
Fibroadenoma was the most common finding in present study, constituting 65.4% of all benign cases. Most of the cases were observed in the age group of 21-30 years, followed by 11-20 years. This was consistent with the findings of Padmom L et al., [14] Fibrocystic disease was the second most common lesion, responsible for 23.1% of all benign lesions in the current study, mostly occurring in the fourth decade. This was supported by the studies conducted by Kapoor B et al., and Anushree CN et al., which accounted for 22.85% and 20% of cases respectively [5,15].
Lesions of the male breast were observed in 24 cases. Among males, the most common finding was gynaecomastia (3.2%) among benign breast lesions, which was similar to the findings of Pudale S and Tonape SD, as well as Parajuli S et al., regarding all benign breast lesions [12,16]. The incidence was most common in the second decade of life, followed by the third decade.
Padmom L et al., found that the incidence of inflammatory breast diseases was 2.9% among all lesions, which aligns with present study finding of 2.5% for inflammatory lesions among all breast lesions (benign, borderline, and malignant) [14]. However, Pai SG reported this incidence to be 9.8%, [17]. Other benign breast lesions have also been analysed and compared with findings from other studies, as shown in [Table/Fig-9] [5,12,14,16-19].
Comparision of studies for benign breast lesions [5,12,14,16-19].
| Lesion name | Present study | Pudale S and Tonape SD (2015) [12] | Padmom L et al., (2020) [14] | Kapoor B et al., (2020) [5] | Parajuli S et al., (2011) [16] | Pai SG (2019) [17] | Hemrajani D et al., (2018) [18] | Patil V et al., (2017) [19] |
|---|
| FA | 50.4% (TLS)65.4% (BLS) | 40% (BLS) | 57% (TLS) | 51.42% (BLS) | 39.47% (TLS) | 64.7% (BLS) | 56.74% (BLS) | 65.7% (BLS) |
| FCD | 17.8% (TLS)23.1% (BLS) | 32.78% (BLS) | 10% (TLS) | 22.85% (BLS) | 18.42% (TLS) | 16.3% (BLS) | 6.1% (BLS) | 10% (BLS) |
| LA | 0.24% (TLS) 0.31% (BLS) | 1.67% (BLS) | - | - | - | 2.6% (BLS) | 1.53% (BLS) | 2.5% (BLS) |
| Adenosis | 0.84% (TLS) 1.09% (BLS) | - | 16.26% (TLS) | - | - | - | 0.3% (BLS) | 1.87% (BLS) |
| Inflammatory | 2.52% (TLS) 3.2% (BLS) | | 2.9% (TLS) | 12.8% (BLS) | 6.9% (TLS) | 9.8% (BLS) | 12.76% (BLS) | 4.37% (BLS) |
| Benign phyllodes | 0.48% (TLS) 0.62% (BLS | 0.55% (BLS) | 0.5% (TLS) | 2.85% (BLS) | - | 5.2% (BLS) | 1.22% (BLS) | 5.6% (BLS) |
| TA | 0.84% (TLS) 1.09% (BLS) | 0.55% (BLS) | - | - | - | - | 1.53% (BLS) | 0.62% (BLS) |
| MGA | 0.96% (TLS) 1.2% (BLS) | - | - | - | 1.75% (TLS) | - | - | - |
| Gynaecomastia | 2.52% (TLS) 3.2% (BLS) | 2.23% (BLS) | - | - | 6.14% (TLS) | 3.2% (BLS) | 11.96% (BLS) | 6.25% (BLS) |
FA: Fibroadenoma; FCD: Fibrocystic disease; LA: Lactational adenoma; MGA: Microglandular adenosis; TA: Tubular adenoma; BLS: Benign lesions studied; TLS: Total lesions studied (i.e., Benign, Borderline and Malignant)
There were a total of nine cases of atypical ductal hyperplasia, which constituted an incidence of 1.08% among all the breast lesions (benign, borderline, and malignant) studied. This was consistent with the findings of Maji A et al., who reported the incidence to be 1.81% [13].
Nikumbh DB et al., in his seven-year study, found the incidence of borderline phyllodes tumours to be 0.21%, which corresponds with present study finding of 0.24% for borderline phyllodes [20]. Diagnosing DCIS poses a formidable challenge in clinical practice. The incidence of DCIS, according to Dayanand V et al., and Bhavani C et al., was reported to be 0.46% and 0.64%, respectively, which was consistent with present study finding of 0.36% [21,22]. Nonetheless, Kumbhakar D et al., reported the incidence to be 2.37% [11]. Among benign and borderline breast lesions, fibroadenoma is one of the leading causes of palpable breast lesions, followed by fibrocystic disease. Therefore, the authors aim to raise awareness about benign and borderline breast lesions among clinicians.
Limitation(s)
This was a hospital-based, single-centre study; therefore, the data may not be applicable to a larger population. Additionally, long-term follow-up of the patients was not conducted, which impedes the evaluation of the course and outcome of the disease.
Conclusion(s)
Benign breast diseases comprise a diverse range of disorders and constitute a significant source of breast-related issues among females, surpassing malignant and premalignant lesions. These conditions are fairly common in younger females of reproductive age, and it is crucial to differentiate these benign lesions from malignant and borderline conditions through histopathological examination. Borderline lesions were less prevalent in the current study, with the majority of cases being Atypical Ductal Hyperplasia (ADH). A thorough evaluation and a systematic approach to all cases of breast lesions are recommended to rule out the potential for breast cancer. Early diagnosis, treatment, and adequate follow-up are essential for achieving the most favourable outcome for the patient.
TLS: Total lesions studied i.e., benign, borderline and malignant lesions; BLS: Benign lesions studied
TLS: Total lesions studied
FA: Fibroadenoma; FCD: Fibrocystic disease; LA: Lactational adenoma; MGA: Microglandular adenosis; TA: Tubular adenoma; BLS: Benign lesions studied; TLS: Total lesions studied (i.e., Benign, Borderline and Malignant)