The thyroid gland plays a wide range of physiological roles in the body, making it unique among other endocrine organs. The hormones released from the thyroid gland affect all body organs and help maintain homeostasis and bodily integrity [1]. Among all the endocrine disorders, thyroid disorders are the most common in India [2]. The thyroid gland has been the subject of intense research and considerable attention due to the broad spectrum of diseases, ranging from functional and immunologically mediated enlargements to neoplastic lesions. Although chronic thyroid diseases have become a significant global cause of morbidity and mortality, literature is scarce regarding the burden of chronic thyroid diseases in Southern India. These disorders can manifest as either hyperthyroidism or hypothyroidism, or as mass lesions [3]. The enlargements may sometimes be diffuse or nodular, causing noticeable physiological changes. In contrast, patients with papillary carcinoma of the thyroid with secondaries in lymph nodes may remain asymptomatic until a very late stage [4]. Thyroid cancer is the most common endocrine malignancy [5].
Pathology within the endocrine system is not frequently found at autopsy, and when identified, it is even less commonly the cause of death. Nevertheless, the examination of the endocrine system is part of any thorough post-mortem examination and occasionally produces surprises, particularly on histological examination. Studying asymptomatic thyroid lesions in living individuals is a difficult task, and autopsy studies provide the best possible way to investigate these lesions. The data collected during such studies can provide valuable insights for future epidemiological and clinical studies. The present study was undertaken to investigate the histomorphological features and spectrum of thyroid lesions in autopsy specimens.
Materials and Methods
The present study was a descriptive cross-sectional and prospective study carried out on autopsy specimens of the entire thyroid gland, which were dissected from deceased individuals during post-mortem examinations at the Karnataka Institute of Medical Sciences (KIMS), Hubballi, Karnataka, India. The specimens were received in the Department of Pathology, KIMS, Hubballi, from November 1, 2016, to October 31, 2017, adhering to the inclusion criteria established for the study. Ethical clearance was obtained from RGUHS, Bengaluru, Karnataka, with the reference number 01_M012_72709.
Inclusion criteria: All autopsy specimens of the entire thyroid gland were taken from adults aged 18 years and above were included in the study.
Exclusion criteria:
Putrefied and decomposed bodies.
Cases of death due to compression of the neck.
Thyroid-related causes of death.
Special cases (custodial deaths, assaults, murder cases).
Railway accidents.
Autolysed specimens of the thyroid.
Individuals aged below 18 years.
Study Procedure
After adequate fixation using 10% neutral buffered formalin, the specimens were subjected to gross examination and were sectioned serially. A single section from each lobe of the thyroid and the isthmus was sampled in grossly normal thyroid specimens. If any lesions were identified, grossly adequate representative areas were sampled, with a minimum of three sections taken from the lesion proper. Tissue processing was performed according to standard protocols, after which paraffin-embedded sections of 5 μ thickness were cut and stained with Haematoxylin and Eosin (H&E) stain. Stained slides were studied under a microscope and diagnosed based on histopathological findings.
Statistical Analysis
The statistical analysis was carried out using Statistical Packages for Social Sciences (SPSS) software (version 14.0). Descriptive analysis was performed using frequencies and percentages.
Results
During the study period, considering the inclusion and exclusion criteria, 140 autopsy specimens of the entire thyroid gland were included in the study, all of whom had no clinical history of thyroid disease. Males constituted 81 (57.9%) and females 59 (42.1%), resulting in a male-to-female ratio of 1.4:1. The mean age of the study participants was 40 years, with a minimum age of 18 years and a maximum age of 68 years.
The mean weight of the thyroid gland was 19.24 grams, with a minimum of 10 grams and a maximum of 50 grams, and a Standard Deviation (SD) of 8.413 grams. The mean weight of the gland was 17.32±6.13 g in males and 21.86±10.28 g in females.
Histologically, thyroid lesions were broadly categorised into normal, non neoplastic, and neoplastic lesions. Normal thyroid specimens contributed to the majority of the autopsy specimens. Non neoplastic lesions were more common than neoplastic lesions. The frequency of various non neoplastic and neoplastic lesions is provided in [Table/Fig-1].
Distribution of non neoplastic and neoplastic lesions.
| Non neoplastic lesions | Number of cases |
|---|
| Adenomatous goitre | 33 |
|---|
| Hashimoto’s thyroiditis | 09 |
| Lymphocytic thyroiditis | 04 |
| Primary hyperplasia | 01 |
| Riedel’s thyroiditis | 01 |
| Thyroglossal cyst | 01 |
| Papillary microcarcinoma, conventional type | 01 |
| Total | 50 |
Out of 140 cases, 90 (64.3%) were normal, 49 (35.0%) were non neoplastic, and 1 (0.7%) was neoplastic. The most common non neoplastic lesion was goitre, accounting for 34 (24.3%) of the cases studied, followed by thyroiditis at 14 (10.0%). One intrathyroidal thyroglossal cyst was observed, accounting for 0.7% of the patients studied. In present study, only one neoplastic lesion was identified: a papillary microcarcinoma, which accounted for 0.7% of the cases studied.
The spectrum of various non neoplastic lesions included adenomatous goitre, which accounted for 67.4%, followed by Hashimoto’s thyroiditis at 18.4% and lymphocytic thyroiditis at 8.2%. Other types of lesions included primary hyperplasia, Reidel’s thyroiditis, and thyroglossal cysts. Most cases of goitre and thyroiditis were distributed among the age group of 31-40 years. [Table/Fig-2] shows the histomorphological spectrum of lesions according to age group. Goitre and thyroiditis were more commonly observed in females than in males. The histomorphological spectrum of lesions according to gender has been depicted in [Table/Fig-3].
Histomorphogical spectrum of lesions according to age group.
| Age groups (in years) | Histomorphological spectrum | Total |
|---|
| Normal | Non neoplastic | Neoplastic |
|---|
| Goitre | Thyroiditis | Thyroglossal cyst | Papillary microcarcinoma, conventional type |
|---|
| 11-20 | 4 | 3 | 3 | 0 | 0 | 10 |
| 21-30 | 20 | 7 | 2 | 0 | 1 | 30 |
| 31-40 | 27 | 10 | 4 | 0 | 0 | 41 |
| 41-50 | 20 | 8 | 2 | 1 | 0 | 31 |
| 51-60 | 16 | 4 | 3 | 0 | 0 | 23 |
| 61-70 | 3 | 2 | 0 | 0 | 0 | 5 |
| Total | 90 | 34 | 14 | 1 | 1 | 140 |
Histomorphogical spectrum of lesions according to sex.
| Categories | Histomorphological spectrum | Gender | Total number of cases |
|---|
| Male | Female |
|---|
| Normal | | 64 | 26 | 90 |
| Non neoplastic | Goitre | 10 | 24 | 34 |
| Thyroiditis | 6 | 8 | 14 |
| Thyroglossal cyst | 1 | 0 | 1 |
| Neoplastic | Papillary microcarcinoma, conventional type | 0 | 1 | 1 |
| Total | | 81 | 59 | 140 |
Non Neoplastic Lesions
Adenomatous goitre: Adenomatous goitre is the most common non neoplastic lesion, accounting for 67.4% of non neoplastic lesions. The male-to-female ratio is 0.4:1. Among 33 cases, nodular goitre comprised 30 (90.9%) cases and colloid goitre 3 (9.1%) cases. Nodularity was observed on the cut surface in 30 cases. The minimum and maximum sizes of the nodules were 0.8 cm and 2.5 cm, respectively, with a mean size of 1.532 cm in diameter and a standard deviation of 0.4792 cm. The cut surface of the gland revealed colloid-filled areas appearing as brown, glassy, and translucent in 24 cases, while nine patients exhibited colloid-filled areas alongside tan-white areas, resulting in a variegated appearance [Table/Fig-4a].
Gross photograph and photomicrograph of multinodular goitre: a) Cut surface showing colloid-filled nodules; b) Low power view showing thyroid gland with multiple nodules of varying sizes (H&E; x10); c) Low power view showing follicles of varying sizes filled with colloid and cyst macrophages (H&E; x10); d) High power view showing cystic changes (H&E; x40).
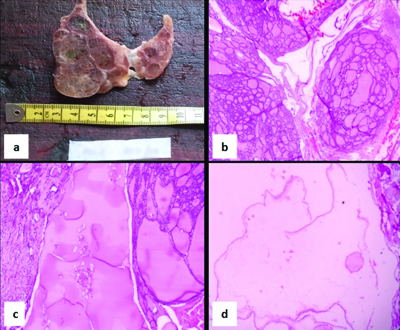
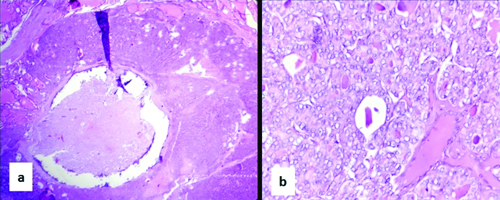
Microscopically, the lesions showed follicles arranged in varying sizes, consisting of macro, micro, normofollicles, and cystic follicles [Table/Fig-4b]. The follicles were filled with variable amounts of colloid, ranging from abundant to moderate to scant [Table/Fig-4c]. Most follicles were predominantly lined by cuboidal cells, followed by flattened and columnar cells. These cells exhibited moderate eosinophilic to amphophilic cytoplasm and round to oval nuclei. Cystic changes were noted in three cases, and hyperplastic adenomatous nodules were present in 10 patients. The smallest nodule measured 1 cm, while the largest was 2.5 cm in diameter [Table/Fig-4d]. All lesions exhibited incomplete to complete irregularly thick reactive fibrous walls, and the adjacent thyroid demonstrated features of adenomatous goitre in all cases. Incomplete fibrous walls were observed in two patients, while entirely irregularly thick fibrous walls were seen in eight cases [Table/Fig-5a,b].
Photomicrograph of multinodular goitre with secondary hyperplasia: a) Low power view showing thyroid gland with nodule surrounded by an irregularly thickened capsule (H&E; x10); b) High power view showing follicles arranged back to back with scant colloid (H&E; x40).
Focal dense lymphocytic aggregates, suggesting an association with lymphocytic thyroiditis, were noted in two cases. In one case, lymphoid follicles with germinal centre formation, focal destruction of follicles, and Hürthle cell change were identified, indicating an association with Hashimoto’s thyroiditis. Additionally, 11 cases showed scattered lymphocytic infiltrates, and one case exhibited acute inflammatory cell infiltrate in the stroma.
The most common stromal change observed was fibrosis, which was present in all cases. Congestion and haemorrhage were also seen in most cases.
Thyroiditis: In present study, 14 cases (10%) of thyroiditis were observed, accounting for 28.6% of non neoplastic lesions. The male-to-female ratio was 0.7:1. Among the cases of thyroiditis, Hashimoto’s thyroiditis was the most common, followed by lymphocytic thyroiditis, with one case of Reidel’s thyroiditis also noted.
Hashimoto’s thyroiditis was the second most common non neoplastic lesion, constituting 64.3% (9 cases) and 18.4% of neoplastic lesions. Three cases occurred in males, while six cases were reported in females. Most cases were observed in the age group of 31-40 years. Among these cases, 8 (88.9%) were of the classic type, and 1 (11.1%) was of the nodular type of Hashimoto’s thyroiditis [Table/Fig-6a]. In addition to these nine cases, one case was seen in association with adenomatous goitre. Grossly, eight cases exhibited a lobular surface, while one case showed nodularity. The cut surface of all cases was diffusely tan-yellow to tan-white.
Gross photograph and photomicrograph of Hashimoto’s thyroiditis: a) External surface showing nodularity and cut surface showing lobulated homogenous colloid depleted grey white to grey tan areas; b) High power view showing Hurthle cell change (H&E; x40); c) Dense lymphocytic infiltration forming lymphoid follicle with the germinal centre within the thyroid parenchyma (H&E; x10); d) Giant cell reaction with lymphocytic infiltration is seen (H&E; x40).
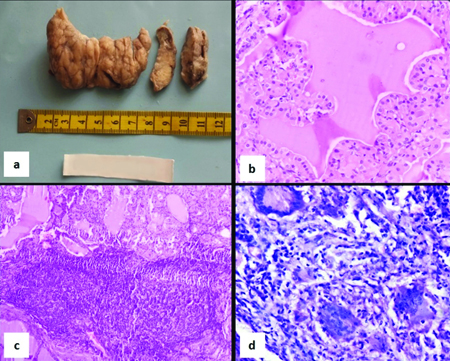
Microscopically, the follicular cells were predominantly cuboidal and flattened, with round to oval nuclei, delicate chromatin, and a moderate amount of cytoplasm. The follicles varied in size. All cases exhibited Hurthle cell change, characterised by abundant eosinophilic granular cytoplasm, vesicular nuclei, and prominent nucleoli. Moderate amounts of colloid were observed in most cases. All cases showed minimal stromal fibrosis. Dense lymphocytic infiltrates were seen in eight patients, and germinal centre formation was observed in one case. All cases displayed plasma cell infiltration and destruction of the follicles [Table/Fig-6b-d].
Chronic (focal) lymphocytic thyroiditis constituted 4 (28.6%) cases of thyroiditis cases and 8.2% of non neoplastic lesions. In two cases, the cut surface of the gland appeared unremarkable, while the other two patients exhibited tan-yellow to tan-white areas. Microscopically, all four cases showed dense lymphocytic aggregates. In addition to these cases, two were seen in association with nodular goitre. In all these cases, there was no associated stromal fibrosis, oncocytic cytoplasmic change, or follicular cell atrophy, except in two cases associated with nodular goitre, which exhibited stromal fibrosis.
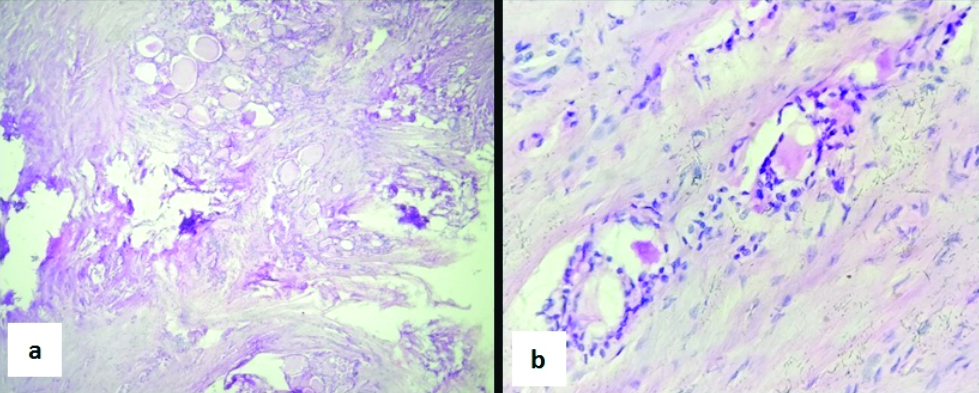
In present study, one case of Reidel’s thyroiditis was diagnosed, accounting for 7.1% of thyroiditis cases and 2.0% of non neoplastic lesions. It was observed in a 38-year-old female. Grossly, the gland exhibited a firm to hard consistency; the external surface showed an opaque, thickened capsule, and the cut surface was tan-white with fibrosis. Microscopically, the parenchyma was replaced by dense fibrosis, with remnants of thyroid follicles present. Fibrosis was more prominent in the isthmus, leading to the entrapment of the follicles within the collagen. Chronic inflammatory cell infiltrates were noted [Table/Fig-7a,b].
Photomicrograph of Riedel’s thyroiditis: a,b) Low and high power views showing replacement of the parenchyma by dense fibrosis and remnants of thyroid follicles (H&E; x40).
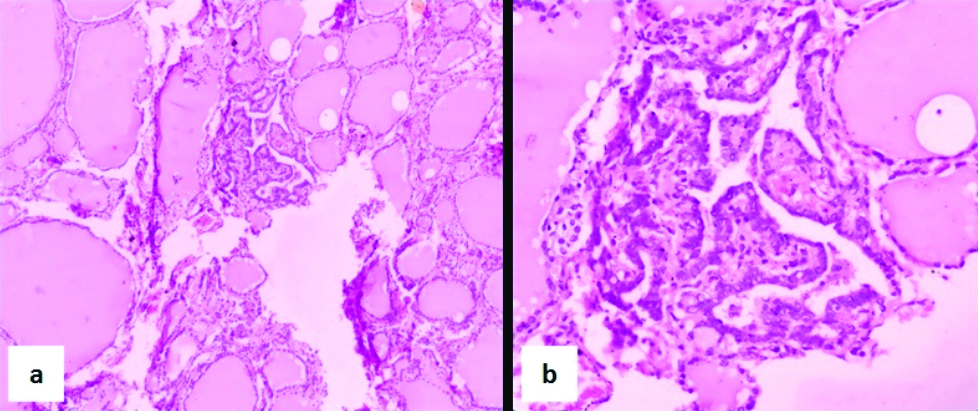
Primary hyperplasia/diffuse toxic goitre: one instance was documented in present study, accounting for 2.0% of non neoplastic lesions and 2.9% of goitre cases. The present case involved a 38-year-old female. Grossly, the gland weighed 40 grams and showed diffuse symmetrical enlargement. The cut surface appeared diffusely tan-yellow to tan-white with a lobulated appearance. Microscopically, follicular cells were arranged in normofollicles, macrofollicles, and a few areas exhibited papillary arrangements. The cells were cuboidal to columnar, with abundant amphophilic cytoplasm, round to oval nuclei, and coarse chromatin in some areas. A moderate amount of colloid was present, with scalloping of the colloid observed. There were dense lymphocytic infiltrates with areas of germinal centre formation, and the stroma showed congested blood vessels [Table/Fig-8a,b].
Photomicrograph of primary hyperplasia (Diffuse toxic goitre): a) Low power view showing follicular cells were arranged in normofollicles, macrofollicles and a few areas showing papillary arrangement (H&E; x10); b) The cells were cuboidal to columnar with abundant amphophilic cytoplasm, round to oval nucleus and coarse chromatin at places. A moderate amount of colloid with scalloping of colloid is seen (H&E; x40).
Thyroglossal cyst: Regarding the thyroglossal cyst, one case of an intrathyroidal thyroglossal cyst was identified in present study, accounting for 2.0% of non neoplastic lesions. This case involved a 45-year-old male. The cut surface revealed a cyst in the left lobe measuring 1.5 cm in diameter; the cyst was smooth-walled and contained colloid. Microscopically, the cyst wall was lined by columnar epithelium, while the rest of the thyroid gland appeared unremarkable.
Neoplastic Lesion
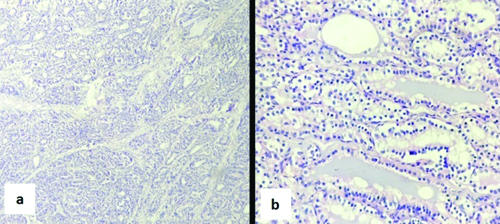
Papillary carcinoma: One case of papillary microcarcinoma, a conventional type, was observed in this study, accounting for 0.7% of the total cases. It was seen in a 30-year-old female; grossly, the lesion was not visible. Microscopically, a non encapsulated tumour arranged in a papillary pattern was identified. The tumour cells exhibited round to oval nuclei, dispersed chromatin, and moderate eosinophilic cytoplasm. Features such as nuclear crowding, overlapping, Orphan Annie nuclei, and nuclear grooves were noted [Table/Fig-9a,b].
Photomicrograph of papillary microcarcinoma: a,b) Low and high power views showing tumour cells arranged in complex branching papillae with cells showing nuclear features of papillary carcinoma. (H&E; x10, x40).
Other Microscopic Findings
Focal lymphocytic infiltration: Focal non specific lymphocytic infiltration was observed in 13 (14.4%) cases of the normal thyroid tissue, with four patients being female and nine male.
Parathyroid: In present study, eight cases involved the parathyroid glands, accounting for 5.7% of the total cases. In 5 (3.6%) patients, the parathyroid gland was found extrathyroidally, while in 3 (2.1%), it was located intrathyroidally. One of the five cases with an extrathyroidal parathyroid gland showed microscopic features consistent with parathyroid adenoma.
Discussion
The true prevalence and nature of thyroid lesions are not documented in the North Karnataka region, and autopsy studies can provide insights into the prevalence of thyroid disease in the community. The morphology of the thyroid gland in autopsy specimens was characterised in this study. In the present study, out of 140 cases, 90 (64.3%) cases were normal, while another study conducted in Kolkata by Das MM et al., reported an incidence of 54.6% [6]. Other studies have reported data varying from 28% to 73.1% for normal thyroids.
The variation in the incidence of normal thyroids among various studies is likely due to differences in the methodology of thyroid examination, variations in the range of alterations that define an abnormal gland, and demographic differences.
In present study, the mean weight of the thyroid gland was 19.24 grams (with a minimum of 10 grams and a maximum of 50 grams) and a standard deviation of 8.413 grams. The mean weight of the gland was 17.32±6.13 g in males and 21.86±10.28 g in females. The mean weight of the thyroid gland in males was comparable to that found in the Indian study conducted by Harjeet A et al., (15.01±7.69 g) [7]. However, the mean weight was less compared to other studies conducted by Das MM et al., (30.57 g) [6]. The mean weight of the thyroid gland in females was comparable to a Turkish study (21.93±7.98 g) [8].
The mean weight was higher compared to another study by Harjeet A et al., (13.16±5.64 g), but lower compared to the study conducted by Das MM et al., which reported a mean weight of 39.43 g [6,7].
Non Neoplastic Lesions
In present study, out of 140 cases, 90 (64.3%) patients were normal, 49 (35.0%) cases were non neoplastic, and 1 (0.7%) case was neoplastic.
Adenomatous goitre: In the present study, adenomatous goitre was the most common non neoplastic lesion, accounting for 67.4% of non neoplastic lesions and 23.6% of all the cases studied. In an Indian study conducted by Das MM et al., the incidence was 20.0%, which does not align with the findings of the present study; this discrepancy may be attributed to demographic variations [6]. Other studies have reported incidences ranging from 7.8% to 50.0% for adenomatous goitre. [Table/Fig-4] compares the distribution of adenomatous goitre and thyroiditis in the present study with that of various other studies.
According to the World Health Organisation (WHO), the upper limit of the weight of a normal gland is 40 grams; however, several studies suggest that a gland weighing more than 35 grams is considered goitrous. In this study, 66.7% of the cases that were histologically proven goitre weighed less than 35 grams. The incidence of diffuse colloid goitre in the present study was 2.1% of the total cases studied and 9.1% among those with adenomatous goitre. Other studies have reported data ranging from 3.3% to 14.3% for diffuse colloid goitre.
Thyroiditis: In present study, 14 cases (10%) of thyroiditis were observed, accounting for 28.6% of non neoplastic lesions. In an Indian study conducted by Das MM et al., the incidence was reported to be 17.5%, which does not align with the findings of the present study [6]. Other studies reported varying incidences of thyroiditis ranging from 1.3% to 29.6% [Table/Fig-10] [6,9].
Comparison of the distribution of Adenomatous goitre and thyroiditis in the present study with other studies of the last 5 years [6,9].
| Authors | Total number of cases examined | Adenomatous goitre (%) | Thyroiditis (%) |
|---|
| Das MM et al., Kolkata (2017) [6] | 240 | 20.0 | 17.5 |
| Fadesewa O et al., Nigeria (2019) [9] | 150 | 24.7 | 4.6 |
| Present study | 140 | 23.6 | 10.0 |
Autoimmune thyroiditis: According to "Rosai and Ackerman’s Surgical Pathology," autoimmune thyroiditis is characterised by extensive lymphocytic infiltration of the gland, which is associated with germinal centre formation [10]. The appearance of the intervening follicles typically determines the category to which a given case belongs: In Grave’s disease, the follicles are diffusely hyperplastic; lymphocytic thyroiditis exhibits relatively normal follicles; and in Hashimoto’s thyroiditis, the follicles are lined by cells showing extensive oncocytic change. Autoimmune thyroiditis includes Hashimoto’s thyroiditis, lymphocytic thyroiditis, and Grave’s disease [10].
The present study identified autoimmune thyroiditis in 16 cases, comprising seven males and nine females. The histological features suggestive of lymphocytic thyroiditis were noted in five cases, two of which were associated with nodular goitre, while Hashimoto’s thyroiditis was identified in ten cases, with one case also associated with adenomatous goitre. Additionally, one case demonstrated features of Grave’s disease.
Scopa CD et al., studied thyroid glands obtained from 120 autopsies and found thyroiditis in 9% of cases, of which Hashimoto’s thyroiditis was seen in 2.5%. Lymphocytic thyroiditis was observed in 7% of cases; of these, six cases were isolated, and two cases were associated with goitre [11]. In a study conducted by Das MM et al., in Kolkata, Hashimoto’s thyroiditis was seen in four cases (1.7%), and lymphocytic thyroiditis was seen in 18 cases (7.5%) [6]. Although autopsy studies regarding autoimmune thyroiditis in India are scarce, a cross-sectional, multicentric epidemiological study was conducted in eight major cities (Bengaluru, Chennai, New Delhi, Goa, Mumbai, Hyderabad, Ahmedabad, and Kolkata) to examine the prevalence of hypothyroidism among the adult population. Antithyroid peroxidase antibodies suggesting autoimmunity were detected in 21.85% (n=1171) of patients [12].
Reidel’s thyroiditis: In present study, non neoplastic lesion, such as Reidel’s thyroiditis (0.7%) were observed. Reidel’s thyroiditis is a rare disease with a reported prevalence of 0.06% to 0.3%, affecting women more than men, and primarily occurring in adults [6]. In the present study, there was only one case of Reidel’s thyroiditis, which accounted for 0.7% of the total cases; this case was seen in a 38-year-old female.
Thyroglossal cyst: An intra-thyroid thyroglossal cyst in an adult is an unusual finding. The present study identified an intra-thyroid thyroglossal cyst in a 45-year-old male, which also accounted for 0.7% of the total cases.
Neoplastic Lesions
In present study, only one neoplastic lesion was observed: papillary microcarcinoma, the conventional type, accounting for 0.7% of the cases studied. In a study conducted by Das MM et al., in Kolkata, the incidence was reported to be 5%, which does not align with the findings of the present study [6]. Other studies have reported data varying from 5% to 37.1% for neoplastic lesions.
In the present study, no benign neoplasms or metastatic lesions were found. In an Indian study by Das MM et al., there were no metastatic lesions to the thyroid; however, benign lesions were present [8]. No benign neoplastic lesions were seen in present study. In contrast, various studies have documented benign lesions, with the most common being follicular adenoma, as reported by Das MM et al., Fadesewa O et al., and Menderico GM et al., [6,9,13].
Only one primary malignant lesion was seen in this study, accounting for 0.7% of the cases. In Das MM et al., study in Kolkata, the incidence of primary malignant lesions was 2.5%, which does not agree with the present findings [Table/Fig-11] [6,9,13].
Comparison of distribution of neoplastic lesions in the present study with various last five year studies [6,9,13].
| Authors | Total number of cases examined | Neoplastic lesions (%) |
|---|
| Benign | Malignant |
|---|
| Total | Benign | Total | Primary | Metastatic |
|---|
| Das MM et al., Kolkata (2017) [6] | 240 | 5 | 2.5 | 2.5 | 2.5 | 0.0 |
| Fadesewa O et al., Nigeria (2019) [9] | 150 | 10 | 10 | 0.0 | 0.0 | 0.0 |
| Menderico GM et al., Brazil (2021) [13] | 100 | 0.0 | 0.0 | 12.82% | 12.82% | 0.0 |
| Present study | 140 | 0.0 | 0.0 | 0.7 | 0.7 | 0.0 |
The frequency of thyroid microcarcinomas varies from 1% to 35.6%. This wide range of incidence can be attributed to different methods of pathological examination, as well as epidemiological and environmental factors. In our study, the incidence of microcarcinoma was 0.7%, being the only malignant lesion identified. Most thyroid microcarcinomas are papillary carcinomas, although other histologic types can be rarely observed.
The low incidence of malignant lesions in present study may be attributed to the possibility that microcarcinoma foci could be missed, especially since, the thyroid gland appeared grossly normal. Additionally, in a study by Scopa CD et al., five of the seven microcarcinomas were not macroscopically visible, and two were found in goitrous thyroids [10].
Other Microscopic Findings
Parathyroid: The thyroid usually develops in conjunction with pharyngeal or branchial pouches, so derivatives of these structures can sometimes be observed in the thyroid. In our study, eight cases showed parathyroid glands, accounting for 5.7% of the cases. In 5 (3.6%) cases, the parathyroid gland was located extrathyroidally, while in 3 (2.1%) patients, the gland was found intrathyroidally. Various authors have estimated that the actual occurrence of intrathyroidal parathyroid tissue is 0.2% [14]. In a study conducted by Scopa CD et al., the incidence was 6% [11].
Focal lymphocytic infiltration: The study noted focal lymphocytic infiltration in 13 cases (14.4%). These cases did not conform to the morphological diagnosis of autoimmune thyroiditis. Focal non specific collections of lymphocytes are observed at autopsy in the thyroids of about one-half of females and one-fourth of males; this finding is regarded as a subclinical manifestation of focal lymphocytic thyroiditis [10]. In a study by Das MM et al., in Kolkata, focal lymphocytic infiltration was observed in 20 cases (8%) [6].
Limitation(s)
The sample size is small, and the number of neoplastic lesions in the present study is limited. A more extensive study population is required from different institutions to compile comprehensive data on thyroid lesions. Exact clinical details regarding the thyroid status of these cases were not available, as they were autopsy cases. The cause of death was not available for all patients. In comparison to the general population, the present study has limitations, including a small sample size and a predominance of the male population. However, the findings from gross examination and microscopy, along with adequate postmortem examination, can help us understand the variations in the normal and natural course of diseases in the thyroid gland.
Conclusion(s)
The present study provides data regarding the distribution of different types of thyroid pathologies in autopsy specimens from the North Karnataka region. Although females constituted only 42.1% of the study population, they exhibited a higher percentage of various diagnostic pathological lesions, such as adenomatous goitre, thyroiditis, and conventional-type papillary microcarcinoma. These incidental lesions suggest that there could be a significant burden of thyroid lesions in our region that might have been detected through routine screening tests available for thyroid conditions.