Lichen Scrofulosorum (LS) is an uncommon tuberculid that was initially described by Hebra in 1868 and typically affects children and young adults. Tuberculids are hypersensitivity reactions in the skin caused by internal Mycobacterium tuberculosis infection. These eruptive lesions result from bacilli spreading through the bloodstream in a host with high resistance to Mycobacterium tuberculosis. Although uncommon, this condition can be a valuable indicator of tuberculosis. Patients with LS typically exhibit a strong tuberculin reaction, concomitant tuberculous involvement of lymph nodes, bone, or other organs, and they show a good response to Antitubercular Therapy (ATT). Hereby, the authors present a case report of a 35-year-old female who presented with multiple papules on her face for five years. A detailed examination revealed no tuberculin reaction, no lymph node involvement, and a good response to ATT. Therefore, LS is a tuberculid that may resemble several other dermatological disorders, necessitating a thorough effort to verify the diagnosis.
Antitubercular therapy, Cutaneous tuberculosis, Langhans giant cells, Mantoux test, Tuberculids
Case Report
A 35-year-old female presented to the Dermatology Outpatient Department (OPD) with complaints of skin-coloured papules on her face for the past five years. These lesions progressively increased in size over the last six months. There was no history of itching, pain, upper respiratory tract infections, trauma, evening rise in temperature, weight loss, loss of appetite, or any drug intake prior to the onset of the lesions. There was no similar family history reported. She was initially diagnosed with sarcoidosis five years ago after a skin biopsy, for which she was given hydroxychloroquine for six months with partial response, after which she discontinued treatment on her own.
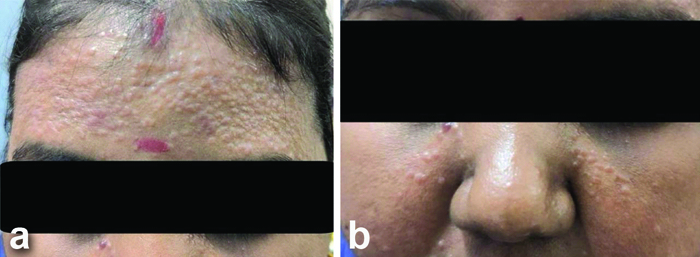
The patient revisited the Outpatient Department with a history of aggravation in the number and size of the lesions over the last six months and was re-evaluated. Cardiovascular, respiratory, abdominal, and central nervous system examinations were normal. Upon general examination, there were no signs of pallor, icterus, cyanosis, clubbing, lymphadenopathy, or pedal oedema. Cutaneous examination revealed multiple closely grouped, smooth, soft to firm skin-coloured, non tender papules measuring 1 mm to 3 mm over the forehead [Table/Fig-1a] and bilateral malar region, with no evidence of any discharge. No lymphadenopathy was noted [Table/Fig-1b]. Examination of the scalp, nails, oral cavity, palms, soles, and genitalia showed no abnormalities.
a,b) Showing multiple skin coloured, smooth, papules over the forehead and malar region.
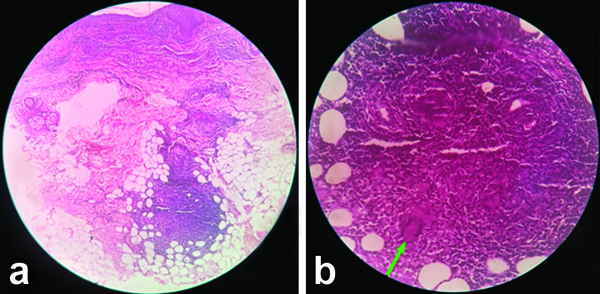
Based on the history and clinical findings, differential diagnoses of papular sarcoid, lupus miliaris disseminatus faciei, and leprosy were considered. A 4 mm punch biopsy from the forehead lesions was taken, which microscopically showed dense dermal inflammatory infiltrate in the upper dermis, with adnexal structures extending to the subcutis. There was evidence of occasional giant cells [Table/Fig-2a]. On high-power view, there were multiple epithelioid granulomas with Langhans-type giant cells and no evidence of necrosis. Histopathology {Haematoxylin and Eosin (H&E)} did not reveal any nerves or perineural infiltrate [Table/Fig-2b]. Acid-fast staining, Mantoux test, and radiological examination of the chest were normal. Haematological findings were within normal limits. The human immunodeficiency virus test, venereal disease research laboratory test, and hepatitis B surface antigen test were negative.
a) Showing dense inflammatory infiltrate in the upper dermis and around the adnexal structures extending to the subcutis (H&E, 4x); b) Showing a granuloma composed of lymphocytic infiltrates with Langhans giant cell (green arrow) (H&E, 40x).
Based on the clinical, laboratory, and histopathological findings, a diagnosis of leprosy was confirmed, and the patient was started on ATT along with a short course of low-dose methylprednisolone (4 mg once a day) for two months. A response to treatment was noted within two weeks of starting the therapy. The patient completed six months of ATT with complete resolution of the lesions [Table/Fig-3].
Showing complete resolution of lesions after completion of six months of ATT.

Discussion
The LS (Lichen Simplex) commonly affects children and adolescents with active tuberculosis and manifests as a lichenoid eruption of minute papules, primarily observed in the Indian subcontinent and Sub-Saharan Africa [1]. Globally, tuberculosis is a leading cause of illness and death, with an estimated 1.3 million cases and 450,000 associated deaths among children each year [2]. The current tuberculosis outbreak is attributed to several factors, including Acquired Immune Deficiency Syndrome (AIDS), the emergence of drug-resistant Mycobacterium tuberculosis strains, poverty, immigration, and insufficient tuberculosis control measures [3]. The overall incidence of cutaneous tuberculosis was estimated to be 0.7% (131 of 18,720 outpatients), and LS was the fourth most common variant, with an 11.2% prevalence, after scrofuloderma (36.5%), lupus vulgaris (31%) and tuberculosis verruca cutis (12.9%). A large study in Hong Kong found that the incidence of LS was the lowest among the three tuberculids at 2%, highlighting the significance of this important marker for possibly undetected cases of tuberculosis [4].
A tuberculid is a cutaneous immune response to the bacterium Mycobacterium tuberculosis, which is frequently latent in other parts of the body. Historically, many different skin manifestations have been diagnosed as tuberculids, but papulonecrotic tuberculid, LS, and erythema induratum of Bazin are the only three entities currently recognised as authentic tuberculids [4,5]. LS is a delayed-type hypersensitivity reaction. The diagnostic criteria for LS include the identification of tuberculoid granuloma on histopathology, indications of concurrent or prior tuberculous foci elsewhere, a strongly positive Mantoux test result, the absence of Mycobacterium tuberculosis in smear and culture, and the resolution of the cutaneous lesion with ATT [6].
The clinical manifestation consists of small, skin-coloured, perifollicular grouped papules, as seen in the current case. The abdomen, trunk, back, proximal limbs, face, vulva, palms, and soles are the primary sites where they typically appear. Their smooth surfaces are covered with tiny scales; however, in this scenario, the patient had lesions only on the face [6,7]. In the current case, there was only a skin-coloured papule on the face, which progressively increased in size, with no lesions elsewhere. Risk factors include overcrowding, direct contact with M. tuberculosis-infected individuals, and low socioeconomic status. The likely factors determining the age distribution of this condition include a greater prevalence of extrapulmonary TB in children and a steady decline in delayed hypersensitivity with age [7,8]. Histopathology shows non caseating epithelioid cell granuloma in the papillary dermis, usually encircling the appendages, with no evidence of necrosis, as observed in the current case.
The granuloma is made up of lymphocytes and epithelioid cells, with a few Langhans giant cells. It is difficult to cultivate tubercle bacilli from skin biopsy material, and they are not visible in the pathological sections. The Mantoux test is positive in LS; however, in present case, it was negative, yet the clinical and histopathological features were suggestive of LS. The diagnosis was confirmed retrospectively due to the response to ATT [9].
The LS is frequently overlooked or misdiagnosed as other follicular disorders, such as keratosis pilaris, pityriasis rubra pilaris, lichen spinulosus, lichen nitidus, and lichenoid sarcoidosis, due to its hidden and asymptomatic presentation [10]. LS shows a marked response to the ATT regimen, with lesions resolving completely without pigmentation or scarring within 12 weeks [11,12], on average, between three to eight weeks.
Conclusion(s)
The LS is a tuberculid that can mimic a number of other dermatological conditions, and meticulous work is required to confirm the diagnosis.
[1]. Singal A, Kaur I, Pandhi D, Gandhi V, Jakhar D, Grover C, Clinico-epidemiological profile of lichen scrofulosorum: A 22-year, single-center, retrospective studyInternational Journal of Dermatology 2021 60(10):1278-84.10.1111/ijd.1573734181284 [Google Scholar] [CrossRef] [PubMed]
[2]. Singal A, Bhattacharya SN, Lichen scrofulosorum: A prospective study of 39 patientsInternational Journal of Dermatology 2005 44(6):489-93.10.1111/j.1365-4632.2005.02499.x15941438 [Google Scholar] [CrossRef] [PubMed]
[3]. Selva PS, Mantoux skin test induced Lichen scrofulosorumJournal of Evolution of Medical and Dental Sciences 2014 3(53):12360-64.10.14260/jemds/2014/3640 [Google Scholar] [CrossRef]
[4]. Khayyam SU, Khayyam KU, Muzammil S, Mohan K, Clinical profile of lichen scrofulosorum, a cutaneous manifestation with focus on tubercular lymphadenitis in a 15-year-old male-a case reportSch J Med Case Rep 2024 3:385-88.10.36347/sjmcr.2024.v12i03.038 [Google Scholar] [CrossRef]
[5]. Thami GP, Kaur S, Kanwar AJ, Mohan H, Lichen scrofulosorum: A rare manifestation of a common diseasePediatric Dermatology 2002 19(2):122-26.10.1046/j.1525-1470.2002.00053.x11994173 [Google Scholar] [CrossRef] [PubMed]
[6]. Rajendiran R, Bolia R, Khuraijam S, Singh A, Lichen scrofulosorum: Cutaneous manifestation of tuberculosisThe Journal of Pediatrics 2021 239:246-47.10.1016/j.jpeds.2021.07.04034293370 [Google Scholar] [CrossRef] [PubMed]
[7]. Meghe SR, Singh A, Bhatt DM, Gupta SN, Hanumanthaiah V, Talasila SR, A Case report on Scrofuloderma: A cutaneous manifestation of tuberculosisCureus 2024 16(6):e6256510.7759/cureus.62565 [Google Scholar] [CrossRef]
[8]. Jazia EB, Hachfi W, Trimech M, Hmissa S, Jeddi CH, Omezzine-Letaief A, Detection of mycobacterial tuberculosis DNA in lichen scrofulosorumJournal of the American Academy of Dermatology 2006 55(2):S54-S55.10.1016/j.jaad.2005.08.04816843126 [Google Scholar] [CrossRef] [PubMed]
[9]. Otto AI, Harsing J, Herjavecz I, Kiss M, Karpati S, Scrofuloderma associated with granuloma annulare-like lichen scrofulosorumActa Dermato-Venereologica 2009 89(6):640-42.10.2340/00015555-071719997700 [Google Scholar] [CrossRef] [PubMed]
[10]. Smith NP, Ryan TJ, Sanderson KV, Lichen scrofulosorum: A report of four casesBr J Dermatol 1976 94:319-25.10.1111/j.1365-2133.1976.tb04391.x1252363 [Google Scholar] [CrossRef] [PubMed]
[11]. Evans RG, Warner J, Lichen scrofulosorum following BCGArch Dis Child 1967 42:44810.1136/adc.42.224.4484951645 [Google Scholar] [CrossRef] [PubMed]
[12]. Molpariya A, Ramesh V, Lichen scrofulosorum: Importance of early recognitionClinical and Experimental Dermatology 2017 42(4):369-73.10.1111/ced.1305028258598 [Google Scholar] [CrossRef] [PubMed]