Introduction
Patients with Autoimmune Inflammatory Rheumatic Disease (AIIRD) are at an increased risk of developing infectious diseases. Vaccination is recommended for these patients by various societies as a preventive strategy. Despite this, the coverage of vaccination is exceedingly low, especially in developing countries.
Aim
To estimate the coverage of pneumococcal and influenza vaccinations, as well as Vaccine Effectiveness (VE).
Materials and Methods
This was a cross-sectional study conducted over a duration of one year, from December 2021 to December 2022, in the Department of Internal Medicine and Allied Specialties at the Sher-I-Kashmir Institute of Medical Sciences (SKIMS), Srinagar, Jammu and Kashmir, India. All consenting AIIRD patients aged over 18 years were enrolled in the outpatient department of Internal Medicine and Allied Specialties at SKIMS, Srinagar, Jammu and Kashmir, India. A history of seasonal influenza and pneumococcal vaccinations was obtained. The coverage of vaccination was determined, and patients were followed-up over a period of one year to assess VE. The Chi-square test was used for comparing categorical values, with a p-value of <0.05 considered significant.
Results
This study included 438 patients, of which 348 (79.5%) were females and 90 (20.5%) were males. The mean age of the study population was 38±11.8 years. Out of 438 patients, only 100 (22.8%) were vaccinated against influenza, while a total of 90 (20.5%) patients had received one or more doses of pneumococcal vaccines. The incidence of symptomatic influenza and pneumococcal pneumonia was higher in the unvaccinated groups. Both vaccines were found to be safe and effective, with a VE of 73.21% for the influenza vaccine and 65.26% for the pneumococcal vaccine.
Conclusion
Present study reveals an overall low coverage of these vaccinations among patients with AIIRD in the region, which needs to be addressed. The findings indicate that influenza and pneumococcal vaccines are safe and effective for patients with AIIRD.
Introduction
Patients with AIIRD have an increased susceptibility to infections, largely stemming from both the immune system compromise associated with the disease and the use of immunosuppressive medications. Given this heightened risk, vaccination plays a crucial role in their overall healthcare management. Patients with AIIRD face a higher risk of morbidity and mortality from vaccine-preventable diseases, such as influenza and Streptococcus pneumoniae, compared to the general population [1-5]. Most leading medical societies, including the American College of Rheumatology and the European League against Rheumatism, recommend vaccinations against these diseases for patients with AIIRD [6-11].
Vaccinations, which may be either inactivated or live based on the indication, are required for patients with AIIRD who are either planning to start or are currently undergoing immunosuppression. Inactivated vaccines include Pneumococcal, seasonal influenza, Hepatitis A and B, meningococcus, Haemophilus influenzae, and the recombinant Zoster vaccine, among others. Live, attenuated vaccines include Zoster Vaccine Live (ZVL), Measles, Mumps and Rubella (MMR), yellow fever, and others. To ensure maximum protection, it is recommended that vaccinations be administered several weeks before initiating immunosuppressive therapy. This strategy enhances the probability of eliciting a protective immune response, especially in the case of rituximab, which significantly diminishes humoral immunity [12].
Administering vaccinations before the initiation of immunosuppressive therapy not only allows for the use of necessary live vaccines, which are typically contraindicated once immunosuppression has begun, but also ensures the completion of any required series of inactivated (non live) vaccines prior to starting immunosuppressive medications. Live vaccines should ideally be given at least four weeks before beginning immunosuppression to mitigate the risk of disseminated disease associated with live vaccines [13]. In the majority of AIIRD patients who are on conventional synthetic Disease-Modifying Antirheumatic Drugs (DMARDs), most biologics, and glucocorticoids, vaccinations are anticipated to provide sufficient protection. However, it is worth noting that the immune response to some vaccines may be somewhat diminished [14].
While there exists a theoretical risk that the immune response triggered by vaccination could lead to exacerbations of autoimmune diseases, the available evidence, though limited, indicates that vaccine administration does not increase disease activity in patients with AIIRD [15-19]. Despite these recommendations, the rate of vaccine uptake remains low among patients with AIIRD [20-23]. For instance, a large multinational cohort study involving 3,920 patients with rheumatoid arthritis revealed that more than half of the patients had never been vaccinated against pneumococcal disease or influenza, and less than a third were appropriately vaccinated [20]. The primary reason cited by patients for not getting vaccinated was the lack of a recommendation from their healthcare provider [21]. In a study that included 310 physicians, including internal medicine specialists, rheumatologists, and primary care physicians, it was found that only 53.9% were aware of vaccine schedules, and only 53.2% recommended vaccines to their patients [24]. The coverage of vaccination, which is an important preventive measure for patients with AIIRD, is largely unknown in our patient population. In this context, the study aimed at addressing the knowledge gap regarding the coverage and efficacy of influenza and pneumococcal vaccination in patients with AIIRD. The primary objective of the present study was to estimate the coverage of pneumococcal and influenza vaccinations. The secondary objective was to confirm Vaccine Effectiveness (VE).
Materials and Methods
This was a cross-sectional observational study conducted over a duration of one year, from December 2021 to December 2022, in the Department of Internal Medicine and Allied Specialties at the Sher-I-Kashmir Institute of Medical Sciences (SKIMS), Srinagar, Jammu and Kashmir, India. The study was approved by the Institutional Ethics Committee (IEC number RP 248/2021). As per the institutional protocol, every participant received both verbal and written information about the study before consenting to participate. Consecutive patients with AIIRD who visited the outpatient department of Medicine and Allied Specialties at our institute were included.
Inclusion criteria: Adult AIIRD patients visiting the outpatient clinic of the Department of Internal Medicine and Allied Specialties who consented to participate were included in the study.
Exclusion criteria: Patients aged less than 18 years and patients who did not provide consent were excluded from the study.
Sample size: Consecutive patients with AIIRD who visited the outpatient department of Medicine and Allied Specialties at the institute were included in the study.
Study Procedure
Demographic and clinical details were recorded, which included age, clinical diagnosis, and vaccination status regarding the influenza vaccine and pneumococcal vaccine. Data were collected during patient interviews and from clinical files. All participants were followed over a duration of one year to monitor the development of symptoms consistent with Influenza Like Illness (ILI), as defined by the World Health Organisation (WHO) [25]. Patients who developed symptoms of lower respiratory tract infections or were admitted with pneumonia (CURB 65 ≥ 2) [26] were subjected to testing for pneumococcal pneumonia using a urinary test for pneumococcal antigen. To test for influenza, throat and nasal swabs were collected in viral transport medium (Hi-mediaTM) and were processed immediately (within 3-4 hours) at the influenza laboratory of the Sher-I-Kashmir Institute of Medical Sciences. Samples were analysed using real-time Reverse Transcriptase Polymerase Chain Reaction (RT-PCR) (Applied Biosystems) following the Centers for Disease Control (CDC) protocol. Samples were further subtyped for influenza A and influenza B.
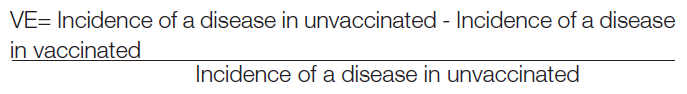
Vaccine Effectiveness (VE) was estimated using the formula [27].
Statistical Analysis
The data recorded on the proforma was compiled in a spreadsheet (WPS Office 2020) and exported to the data editor of the Statistical Package for Social Sciences (SPSS, Version 21.0, IBM SPSS, Armonk, New York, USA). Continuous variables were expressed as mean±SD, and categorical variables were expressed as frequencies and percentages. Data was presented in tabulated form. The Chi-square test was applied for the comparison of categorical variables. A two-tailed p-value was used to calculate statistical significance, with a value of <0.05 considered significant.
Results
The study included 438 patients, of which 348 (79.5%) were females and 90 (20.5%) were males. The mean age of the study population was 38±11.8 years. The majority of patients, 122 (27.9%), belonged to the age group of 31-40 years. The most common AIIRD was rheumatoid arthritis, affecting 320 patients (73.1%), followed by systemic lupus erythematosus, which affected 74 patients (16.9%). Demographic data, underlying AIIRD, and co-morbid conditions are shown in [Table/Fig-1].
Demographic and clinical details of the patients.
| Parameters | n (%)/M±SD |
|---|
| Mean age (years) | 38±11.8 |
| Females | 348 (79.5) |
| Males | 90 (20.5) |
| Mean eGFR (mL/min/1.73 m2) | 88 |
| Hypertension | 27 (6.2) |
| Diabetes mellitus | 9 (2.1) |
| Hypothyroidism | 8 (1.8) |
| ILD | 9 (2.1) |
| Rheumatoid arthritis | 320 (73.1) |
| SLE | 74 (16.9) |
| Other AIIRD | 44 (10.0) |
eGFR: estimated glomerular filtration rate; ILD: Interstitial lung disease; SLE: Systemic lupus erythematosus; AIIRD: Autoimmune inflammatory rheumatic disease
Regarding the treatment of the underlying rheumatologic disorder, 427 patients (97.5%) had a history of steroid exposure, and 345 patients (78.8%) had been exposed to DMARDs. Out of the 438 patients, only 100 (22.8%) were vaccinated against influenza, while a total of 90 (20.5%) patients had received one or more doses of pneumococcal vaccines. Among those vaccinated, 84 patients (92.6%) were vaccinated on the recommendation of a physician, while six patients (7.4%) opted for vaccination on their own [Table/Fig-2].
The incidence of influenza was significantly higher in the unvaccinated group as compared with the vaccinated group (p-value 0.012, Chi-square test).
| Developed influenza | Did not develop influenza | Total |
|---|
| Vaccinated against influenza | 3 | 97 | 100 |
| Not vaccinated against influenza | 38 | 300 | 338 |
| Total | 41 | 397 | 438 |
Nineteen patients (4.3%) developed Influenza A, while 22 patients (5.0%) developed Influenza B. The estimated VE was 81.3% for Influenza A and 66.11% for Influenza B. The seasonal influenza vaccine significantly reduced the incidence of symptomatic influenza, with an overall VE of 73.21%.
A total of 36 patients (8.2%) developed pneumococcal pneumonia. The pneumococcal vaccine reduced the incidence of pneumococcal pneumonia; however, it did not reach statistical significance [Table/Fig-3]. The VE for pneumococcal pneumonia was 65.26%.
The incidence of pneumococcal pneumonia was significantly higher in the unvaccinated group (p-value 0.058, Chi-square test).
| Developed pneumococcal pneumonia | Did not develop pneumococcal pneumonia | Total |
|---|
| Vaccinated against pneumococcus | 3 | 87 | 90 |
| Not vaccinated against pneumococcus | 33 | 315 | 348 |
| Total | 36 | 402 | 438 |
Discussion
A total of 438 patients were included in this study, out of which 348 (79.5%) were females, resulting in a female-to-male ratio of 3.9. The female predominance in AIIRD is well known and may be attributed to various genetic, epigenetic, hormonal, and environmental factors [28]. The most prevalent disease was rheumatoid arthritis (73.1%), followed by SLE (16.9%). Out of 438 patients, only 100 (22.8%) were vaccinated against influenza, while only 90 (20.5%) were vaccinated against pneumococcus. These numbers reflect the overall poor coverage of vaccinations among patients with AIIRD in our region. Likely causes include a lack of awareness, vaccine hesitancy among patients in general, and the cost of vaccines, particularly for patients with limited financial resources. Additionally, a low enthusiasm among treating physicians regarding prescribing vaccines and a failure to counsel patients about the benefits of vaccination may also contribute to such poor coverage.
In a research study led by Jiang Y et al., in China, which focused on the knowledge, attitudes, and practices concerning vaccination among patients with rheumatic diseases, it was discovered that only one out of 235 patients had received the influenza vaccine, and none had been vaccinated against pneumococcus. A mere 3.8% had received a doctor’s recommendation for influenza or pneumococcal vaccines. The primary reasons cited for not getting vaccinated were the perception of vaccines as “unnecessary” and “troublesome to take” [29]. Similarly, in a previously cited study [24], it was found that only 53.9% of physicians out of 310 knew about vaccine schedules, and only 53.2% recommended vaccines to their patients. In another study that included 222 AIIRD patients, it was observed that 68.5% of patients were vaccinated against influenza and 34.7% against Streptococcus pneumoniae [30].
Out of 100 patients vaccinated with the influenza vaccine, three patients developed influenza (A and/or B) during follow-up. Statistical analysis revealed a significant difference (p-value: 0.012) between the incidence of influenza in vaccinated and unvaccinated patients, suggesting that the influenza vaccine has significant overall protective efficacy against influenza A and B in patients with AIIRD. The estimated VE was 81.3% for influenza A and 66.11% for influenza B, respectively. A study conducted by Rose A et al., on 122 subjects demonstrated that the vaccine efficacy against influenza A was 62% [31]. A regional study conducted by Mir H et al., on VE against influenza-related acute respiratory infections revealed a VE against influenza A/H1N1 of 55% [32]. The comparatively higher VE in present study can be attributed to the COVID-19 pandemic during the study period, which witnessed a lockdown and the implementation of COVID-19 appropriate behaviour (wearing masks, maintaining social distancing, using hand sanitizers, frequent hand washing, avoiding crowded places, etc.), leading to an overall decrease in the transmission of respiratory/airborne infections. The VE against influenza B in present study was in agreement with a study conducted by Skowronski DM et al., on 683 patients, which revealed a VE of 69% (57-77) against influenza B [33].
Among 90 patients vaccinated with the pneumococcal vaccine, three developed pneumococcal pneumonia, whereas among 348 unvaccinated patients, 33 developed pneumococcal pneumonia. Statistical analysis revealed a p-value of 0.058, suggesting that pneumococcal vaccination has a protective (but not statistically significant) role against pneumococcal pneumonia in patients with AIIRD. The VE turned out to be 65.26%. This suggests that vaccinated patients with AIIRD have a 65.26% lower chance of developing pneumococcal pneumonia. Similar findings were noted in a population-based study on elderly patients conducted by Vila-Corcoles A et al., which reported a VE of 66% [34].
The findings of present study reveal a considerably low rate of vaccination in patients with AIIRD. These patients are at high-risk of infection due to the underlying disease and immunosuppressive therapies. This calls for increased awareness among both physicians and patients. Moreover, both influenza and pneumococcal vaccines are safe and effective in patients with AIIRD, which should help to alleviate the phenomenon of vaccine hesitancy.
Limitation(s)
The limitations of present study include its observational nature, which makes it prone to biases and confounding factors. Matching for baseline characteristics was not performed, which may have confounded the results. Additionally, being a hospital-based study, it is susceptible to referral and selection biases. Nevertheless, present study demonstrates the safety and efficacy of vaccination in patients with AIIRD.
Conclusion(s)
The present study revealed an overall low coverage of vaccinations among patients with AIIRD in the region, which needs to be addressed. It is crucial to raise awareness among both physicians and patients regarding these vaccinations. This will ensure that more patients can avail themselves of the protective benefits of these vaccines. Present study also indicates that the Influenza and Pneumococcal vaccines are safe and effective for patients with AIIRD. These vaccines represent an important public health measure in preventing respiratory infections among patients with AIIRD, similar to their benefits for the general population and other patients.
eGFR: estimated glomerular filtration rate; ILD: Interstitial lung disease; SLE: Systemic lupus erythematosus; AIIRD: Autoimmune inflammatory rheumatic disease
[1]. Wolfe F, Mitchell DM, Sibley JT, Fries JF, Bloch DA, Williams CA, The mortality of rheumatoid arthritisArthritis Rheum 1994 37(4):481-94.10.1002/art.17803704088147925 [Google Scholar] [CrossRef] [PubMed]
[2]. Glück T, Müller-Ladner U, Vaccination in patients with chronic rheumatic or autoimmune diseasesClin Infect Dis 2008 46(9):1459-65.10.1086/58706318419456 [Google Scholar] [CrossRef] [PubMed]
[3]. Westra J, Rondaan C, van Assen S, Bijl M, Vaccination of patients with autoimmune inflammatory rheumatic diseasesNat Rev Rheumatol 2015 11(3):135-45.10.1038/nrrheum.2014.20625486980 [Google Scholar] [CrossRef] [PubMed]
[4]. Meroni PL, Zavaglia D, Girmenia C, Vaccinations in adults with rheumatoid arthritis in an era of new disease-modifying anti-rheumatic drugsClin Exp Rheumatol 2018 36(2):317-28. [Google Scholar]
[5]. Wakabayashi A, Ishiguro T, Takaku Y, Miyahara Y, Kagiyama N, Takayanagi N, Clinical characteristics and prognostic factors of pneumonia in patients with and without rheumatoid arthritisPLoS One 2018 13(8):e020179910.1371/journal.pone.020179930075013 [Google Scholar] [CrossRef] [PubMed]
[6]. Singh JA, Saag KG, Bridges SL Jr, Akl EA, Bannuru RR, Sullivan MC, 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid ArthritisArthritis Rheumatol 2016 68(1):01-26.10.1002/art.3948026545940 [Google Scholar] [CrossRef] [PubMed]
[7]. Rubin LG, Levin MJ, Ljungman P, Davies EG, Avery R, Tomblyn M, Infectious Diseases Society of America. 2013 IDSA clinical practice guideline for vaccination of the immunocompromised hostClin Infect Dis 2014 58(3):309-18.10.1093/cid/cit81624421306 [Google Scholar] [CrossRef] [PubMed]
[8]. Ledingham J, Gullick N, Irving K, Gorodkin R, Aris M, Burke J, BSR and BHPR Standards, Guidelines and Audit Working Group. BSR and BHPR guideline for the prescription and monitoring of non-biologic disease-modifying anti-rheumatic drugsRheumatology (Oxford) 2017 56(6):865-68.10.1093/rheumatology/kew47928339817 [Google Scholar] [CrossRef] [PubMed]
[9]. Singh JA, Furst DE, Bhara A, Curtis JR, Kavanaugh AF, Kremer JM, 2012 update of the 2008 American College of Rheumatology recommendations for the use of disease-modifying antirheumatic drugs and biologic agents in the treatment of rheumatoid arthritisArthritis Care & Research 2012 64(5):625-39.10.1002/acr.2164122473917 [Google Scholar] [CrossRef] [PubMed]
[10]. Papp KA, Haraoui B, Kumar D, Marshall JK, Bissonnette R, Bitton A, Vaccination Guidelines for patients with immune-mediated disorders on immunosuppressive therapiesJ Cutan Med Surg 2019 23(1):50-74.10.1177/120347541881133530463418 [Google Scholar] [CrossRef] [PubMed]
[11]. Furer V, Rondaan C, Heijstek MW, Agmon-Levin N, van Assen S, Bijl M, 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseasesAnn Rheum Dis 2020 79(1):39-52.10.1136/annrheumdis-2019-21588231413005 [Google Scholar] [CrossRef] [PubMed]
[12]. Bingham CO 3rd, Looney RJ, Deodhar A, Halsey N, Greenwald M, Codding C, Immunization responses in rheumatoid arthritis patients treated with rituximab: Results from a controlled clinical trialArthritis Rheum 2010 62(1):64-74.10.1002/art.2503420039397 [Google Scholar] [CrossRef] [PubMed]
[13]. Bühler S, Eperon G, Ribi C, Kyburz D, van Gompel F, Visser LG, Vaccination recommendations for adult patients with autoimmune inflammatory rheumatic diseasesSwiss Med Wkly 2015 145:w1415910.4414/smw.2015.1415926218860 [Google Scholar] [CrossRef] [PubMed]
[14]. Friedman MA, Winthrop KL, Vaccines and disease-Modifying antirheumatic drugs: Practical implications for the rheumatologistRheum Dis Clin North Am 2017 43(1):01-13.10.1016/j.rdc.2016.09.00327890167 [Google Scholar] [CrossRef] [PubMed]
[15]. Kuruma KA, Borba EF, Lopes MH, de Carvalho JF, Bonfá E, Safety and efficacy of hepatitis B vaccine in systemic lupus erythematosusLupus 2007 16(5):350-54.10.1177/096120330707822510.1177/096120330707822517576737 [Google Scholar] [CrossRef] [CrossRef] [PubMed]
[16]. Pasoto SG, Ribeiro AC, Viana VS, Leon EP, Bueno C, Neto ML, Short and long-term effects of pandemic unadjuvanted influenza A(H1N1)pdm09 vaccine on clinical manifestations and autoantibody profile in primary Sjögren’s syndromeVaccine 2013 31(14):1793-98.10.1016/j.vaccine.2013.01.05723395584 [Google Scholar] [CrossRef] [PubMed]
[17]. Shinjo SK, de Moraes JC, Levy-Neto M, Aikawa NE, de Medeiros Ribeiro AC, Schahin Saad CG, Pandemic unadjuvanted influenza A (H1N1) vaccine in dermatomyositis and polymyositis: Immunogenicity independent of therapy and no harmful effect in diseaseVaccine 2012 31(1):202-06.10.1016/j.vaccine.2012.10.06323123020 [Google Scholar] [CrossRef] [PubMed]
[18]. Mok CC, Ho LY, Fong LS, To CH, Immunogenicity and safety of a quadrivalent human papillomavirus vaccine in patients with systemic lupus erythematosus: A case-control studyAnn Rheum Dis 2013 72(5):659-64.10.1136/annrheumdis-2012-20139322589375 [Google Scholar] [CrossRef] [PubMed]
[19]. Nakafero G, Grainge MJ, Myles PR, Mallen CD, Zhang W, Doherty M, Association between inactivated influenza vaccine and primary care consultations for autoimmune rheumatic disease flares: A self-controlled case series study using data from the Clinical Practice Research DatalinkAnn Rheum Dis 2019 78(8):1122-26.10.1136/annrheumdis-2019-21508631036623 [Google Scholar] [CrossRef] [PubMed]
[20]. Hmamouchi I, Winthrop K, Launay O, Dougados M, Low rate of influenza and pneumococcal vaccine coverage in rheumatoid arthritis: Data from the international COMORA cohortVaccine 2015 33(12):1446-52.10.1016/j.vaccine.2015.01.06525659279 [Google Scholar] [CrossRef] [PubMed]
[21]. Hua C, Morel J, Ardouin E, Ricard E, Foret J, Mathieu S, Reasons for non-vaccination in French rheumatoid arthritis and spondyloarthritis patientsRheumatology (Oxford) 2015 54(4):748-50.10.1093/rheumatology/keu53125667433 [Google Scholar] [CrossRef] [PubMed]
[22]. Costello R, Winthrop KL, Pye SR, Brown B, Dixon WG, Influenza and pneumococcal vaccination uptake in patients with rheumatoid arthritis treated with immunosuppressive therapy in the UK: A retrospective cohort study using data from the clinical practice research datalinkPLoS One 2016 11(4):e015384810.1371/journal.pone.015384827096429 [Google Scholar] [CrossRef] [PubMed]
[23]. Subesinghe S, Rutherford AI, Ibrahim F, Harris H, Galloway J, A large two-centre study in to rates of influenza and pneumococcal vaccination and infection burden in rheumatoid arthritis in the UKBMC Musculoskelet Disord 2016 17:32210.1186/s12891-016-1187-427491386 [Google Scholar] [CrossRef] [PubMed]
[24]. Badak SÖ, Vaccines in adults with autoimmune inflammatory rheumatic disease: What are the knowledge and attitudes of physicians?Arch Rheumatol 2022 37(3):456-65.10.46497/ArchRheumatol.2022.930336589615 [Google Scholar] [CrossRef] [PubMed]
[25]. WHO surveillance case definitions for ILI and SARI. [Internet][cited 2014 Jan]. Available from: https://www.who.int/teams/global-influenza-programme/surveillance-and-monitoring [Google Scholar]
[26]. Lim WS, van der Eerden MM, Laing R, Boersma WG, Karalus N, Town GI, Defining community acquired pneumonia severity on presentation to hospital: an international derivation and validation studyThorax 2003 58(5):377-82.10.1136/thorax.58.5.37712728155 [Google Scholar] [CrossRef] [PubMed]
[27]. Habibzadeh F, Habibzadeh P, Yadollahie M, On measuring vaccine effectiveness with observational study designsActa Med Acad 2022 51(2):134-46.10.5644/ama2006-124.38336318007 [Google Scholar] [CrossRef] [PubMed]
[28]. Fairweather D, Frisancho-Kiss S, Rose NR, Sex differences in autoimmune disease from a pathological perspectiveAm J Pathol 2008 173(3):600-09.10.2353/ajpath.2008.07100818688037 [Google Scholar] [CrossRef] [PubMed]
[29]. Jiang Y, Zhang X, Lv Q, Qi J, Guo X, Wei Q, Knowledge, attitude, and practice regarding infection and vaccination in patients with rheumatic diseases in ChinaHum Vaccin Immunother 2019 15(5):1100-05.10.1080/21645515.2019.156816030689509 [Google Scholar] [CrossRef] [PubMed]
[30]. Krasselt M, Wagner U, Seifert O, Influenza, pneumococcal and herpes zoster vaccination rates in patients with autoimmune inflammatory rheumatic diseasesVaccines 2023 11(4):76010.3390/vaccines1104076037112672 [Google Scholar] [CrossRef] [PubMed]
[31]. Rose A, Kissling E, Emborg HD, Larrauri A, McMenamin J, Pozo F, Interim 2019/20 influenza vaccine effectiveness: Six European studies, September 2019 to January 2020Euro Surveill 2020 25(10):20001531560-7917.ES.2020.25.10.200015332183932 [Google Scholar] [CrossRef] [PubMed]
[32]. Mir H, Haq I, Koul PA, Poor vaccine effectiveness against Influenza B-related severe acute respiratory infection in a temperate north Indian state (2019-2020): A call for further data for possible vaccines with closer matchVaccines (Basel) 2021 9(10):109410.3390/vaccines910109434696202 [Google Scholar] [CrossRef] [PubMed]
[33]. Skowronski DM, Zou M, Sabaiduc S, Murti M, Olsha R, Dickinson JA, Interim estimates of 2019/20 vaccine effectiveness during early-season co-circulation of influenza A and B viruses, Canada, February 2020Euro Surveill 2020 25(7):200010310.2807/1560-7917.ES.2020.25.7.200010332098644 [Google Scholar] [CrossRef] [PubMed]
[34]. Vila-Corcoles A, Ochoa-Gondar O, Guzmán JA, Rodriguez-Blanco T, Salsench E, Fuentes CM, EPIVAC Study GroupEffectiveness of the 23-valent polysaccharide pneumococcal vaccine against invasive pneumococcal disease in people 60 years or olderBMC Infect Dis 2010 10:7310.1186/1471-2334-10-7320298596 [Google Scholar] [CrossRef] [PubMed]