Ameloblastic carcinoma is a rare, aggressive, malignant form of ameloblastoma with a low incidence rate, accounting for 0.3-3.5% of all odontogenic tumours of the jaws and has a poor prognosis. It exhibits a 5:1 mandibular predilection, with the lungs being the most common metastatic site. Clinically, these lesions behave more aggressively than conventional ameloblastomas. The most common sign is an asymptomatic swelling, with less frequent findings of pain, rapid growth, trismus and dysphonia. About 38% of cases may present without typical clinical symptoms or unique clinical presentations. The present case is a rare case report of 40-year-old male patient of ameloblastic carcinoma presenting with a unique clinical manifestation as osteomyelitis. Initially, the patient reported the presence of an unhealed extraction site, followed by gradual swelling with discharge and pain over the past 20 days. After the necessary diagnostic procedures, the case was diagnosed as ameloblastic carcinoma and referred to higher centres for treatment. The lack of typical clinical presentation makes the diagnosis of these cases difficult. To prevent morbidity and mortality associated with these aggressive cases, they must be diagnosed and treated as early as possible.
Case Report
A 40-year-old male patient presented with a chief complaint of pain in the lower left back tooth region for the past 20 days and swelling on the left lower side of the face for one year. Upon inquiry, he reported a history of pain that was insidious, intermittent, dull aching in nature, with moderate intensity and non radiating. The pain was aggravated by eating and relieved by medication. He also experienced yellowish discharge, altered taste sensation, food lodgment and bleeding while brushing. There was no relevant medical history reported. The patient mentioned that he had a lower left back tooth removed three years ago at a local dental clinic. He subsequently noticed a gradual, slow-growing swelling and an unhealed socket at that site. For this, he took analgesics and antibiotics but has not undergone any treatment in the last three years as he was out of the country. Initially, the swelling was mild and slow-growing, but it has now reached its current size, accompanied by numbness on the left-side of the face.
On general examination, all vital signs were normal and no palpable regional lymph nodes were detected. Upon extraoral examination, there was a diffuse swelling evident on the left lower third of the face, measuring approximately 5×4 cm, extending anteroposteriorly about 2 mm away from the corner of the mouth to the tragus of the ear and superoinferiorly from the canthomeatal line to the lower border of the mandible. This swelling caused elevation of the left earlobe and its colour was normal compared to the adjacent skin, with no evident secondary changes. On palpation, the swelling was smooth with a local rise in temperature, hard in consistency, neither tender nor compressible, nor reducible, nor fluctuating, nor pulsatile, nor pinchable, with evident signs of paraesthesia [Table/Fig-1a,b].
Extraoral images (a) Frontal view (b) Lateral view.

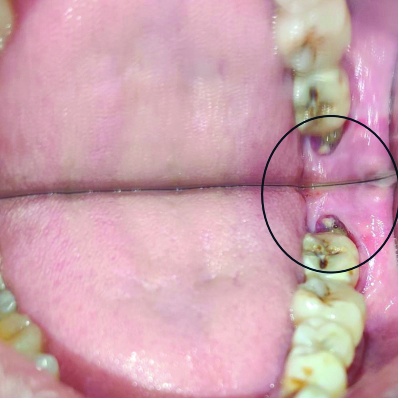
On intraoral examination [Table/Fig-2], an unhealing socket was observed in the region of tooth 38, with granulation tissue present. Upon palpation, necrotic bone was evident, along with buccal wall expansion causing vestibular obliteration from the region of tooth 37 to the ascending ramus, accompanied by pus discharge. Based on these findings, a provisional diagnosis of osteomyelitis of the left posterior mandible was made.
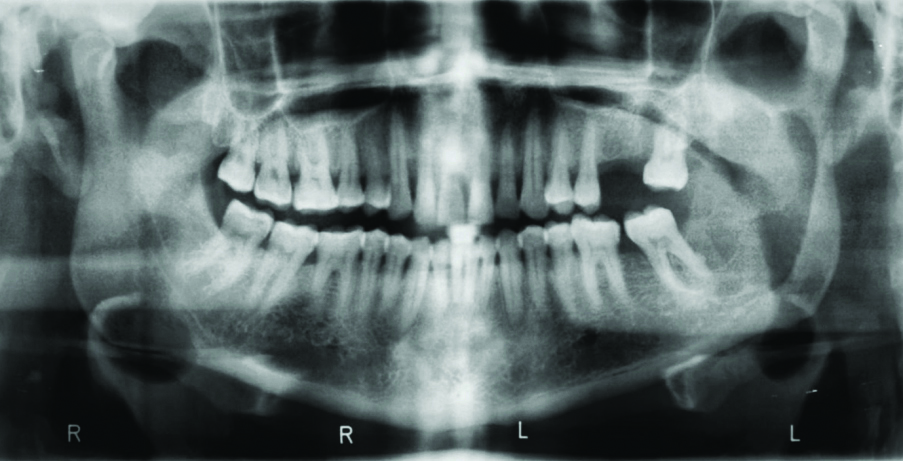
Radiographic examination via Orthopantomogram (OPG) [Table/Fig-3] depicted a localised, unilateral radiolucency extending anteroposteriorly from the mesial root of tooth 37 to the posterior border of the ramus and superoinferiorly from 1 cm below the sigmoid notch to the lower border of the mandible. Inferior displacement of the mandibular nerve was evident.
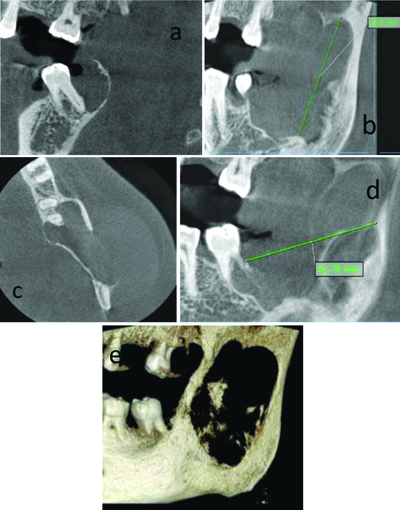
For further confirmation, a Cone Beam Computed Tomography (CBCT) [Table/Fig-4a-e] was performed, which revealed a unilateral, round to ovoid, ill-defined hypodense area measuring approximately 41×42×28 mm. This area extended from the mesial surface of tooth 37 to the posterior border of the ramus anteroposteriorly and superoinferiorly from 3 mm below the sigmoid notch to 4 mm above the lower border of the mandible. There was thinning of the bone mediolaterally, buccal and lingual cortical bone expansion and evident erosion of the buccal cortical plate towards the ascending ramus. Thinning of the lingual cortical bone distal to tooth 37 was also observed, with involvement of the inferior alveolar nerve canal and mild root resorption of tooth 37. Thinning of the sigmoid notch was also evident. The radiographic diagnosis was unicystic ameloblastoma, with radiographic differential diagnosis of infected residual cyst and Odontogenic Keratocyst (OKC). The case was subjected to histopathological examination.
Cone beam computed tomography. a) Sagittal view showing lesion involving whole ramus; b) Sagittal view showing lesion close sigmoid notch; c) Axial section showing buccolingual expansion with erosion of buccal cortical plate; d) Sagittal view showing tooth resorption with greatest anterioposterior dimension; e) 3D image of the lesion.
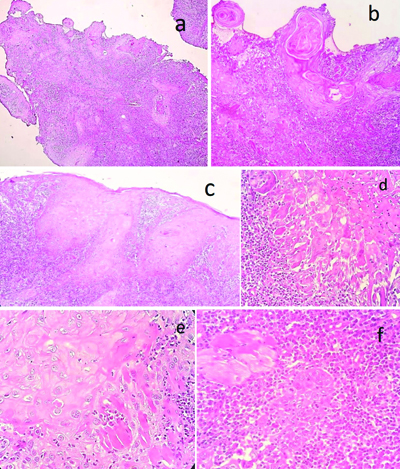
Surprisingly, the histopathological report of Haematoxylin and Eosin (H&E)-stained soft tissue sections [Table/Fig-5a-f] revealed islands, sheets, nests and cords of highly cellular odontogenic epithelium densely packed in an infiltrative pattern within a fibrous stroma. The peripheral cells of the epithelium exhibited hyperchromatic nuclei with reversal of polarity, along with cytoplasmic vacuolations. The epithelial cells displayed varied morphology, including round, oval, angular and spindle shapes, with features such as nuclear enlargement, cellular and nuclear pleomorphism, nuclear hyperchromatism, an altered nuclear-cytoplasmic ratio and a few mitotic figures. The connective tissue was dense and fibrous, with collagen fibres interspersed with flat to plump fibroblasts. Chronic inflammatory infiltrate was predominantly composed of macrophages, neutrophils and plasma cells. Areas of haemorrhage were evident. A focal area showed non keratinised hyperplastic stratified squamous epithelium with areas of acanthosis, cellular and nuclear pleomorphism. Based on these findings, a definitive diagnosis of ameloblastic carcinoma of the mandible was made and the case was referred to a higher centre.
Histopathological images. a) Dysplastic epithelial cells arranged in the form of nests, islands and sheets in the connective tissue (H&E, 4x); b) Dyskeratosis with in the epithelium (H&E, 10x); c) Keratin pearl formation (H&E, 10x); d) Skeletal muscle invasion (H&E, 40x); e) Tumour giant cells (H&E, 40x); f) Abnormal mitotic figures (H&E, 40x).
Discussion
Various synonyms have been provided for carcinomas derived from ameloblastomas, such as malignant ameloblastoma, metastatic carcinoma and primary intra-alveolar epidermoid carcinoma. There is controversy surrounding the classification and definition of ameloblastic carcinoma since this term was introduced by Elzay RP in 1982 [1]. In 1984, Slootweg PJ and Muller H proposed a definition and nomenclature to distinguish ameloblastic carcinoma from malignant ameloblastoma [2].
Ameloblastic carcinoma belongs to the family of malignant epithelial odontogenic tumours, accounting for about 11 cases out of 5,231 total odontogenic tumours of the jaw. In other countries, it is reported to account for approximately 1.6-2.2% of all odontogenic tumours [3,4]. It is classified into primary and secondary types. The primary type arises de novo, whereas the secondary type arises from pre-existing ameloblastoma, which is extremely rare. The exact mechanism for malignant transformation remains unknown due to the limited number of cases. The present case is classified as the primary type, as there is no evidence of a pre-existing ameloblastoma.
In contrast to ameloblastoma, ameloblastic carcinoma exhibits more aggressive clinical behaviour, such as rapid growth, perforation of the cortex and painful swelling. According to past cases reported in the literature [Table/Fig-6] [2,3,5-17], about 17% of cases reported painful swelling involving the mandible [8,11,16]. Additionally, 17% of cases reported paresthesia [3,9,10], while 76% of cases reported aggressive behaviour with indistinct borders and bone destruction [2,3,6-9,11,13-17]. Furthermore, 17% of cases reported an abnormal extracted socket [2,14,16], which was consistent with the present case. In the present case, an unhealed extracted socket was evident, with the presence of necrotic bone along with pus discharge.
List of cases reported in previous literature [2,3,5-17].
| Author/year | Country | Age/gender | Site | Clinical findings | Imagining findings |
|---|
| Pain | Swelling | Paraesthesia | Discharge | Other features | Bone destruction |
|---|
| Augustine D et al., (2013) [6] | India | 44 years Female | Mandible | - | + | | - | Dysphagia, dysarthria | + |
| Roy S and Garg V (2013) [7] | India | 27 years Male | Mandible | + | + | - | - | - | + |
| Sozzi D et al., (2014) [8] | Italy | 14 years Male | Maxilla | - | + | - | - | Tooth mobile | + |
| Srikanth MD et al., (2014) [9] | India | 60 years Male | Mandible | - | + | + | _ | - | + |
| Yunaev M et al., (2014) [10] | Sydney | 40 years Female | Mandible | - | + | + | - | Tooth mobile | Unknown |
| Dutta M et al., (2014) [11] | India | 56 years Male | Mandible | + | + | - | - | Induration | + |
| Kallianpur S et al., (2014) [12] | India | 24 years Male | Mandible | - | + | - | - | - | Unknown |
| Owosho AA et al., (2015) [13] | Pennsylvania | 69 years Male | Mandible | + | - | - | - | Infection | + |
| Matsushita Y et al., (2015) [14] | Japan | 69 years Male | Mandible | - | + | - | - | Abnormal sockets of extracted tooth | + |
| Kishore M et al., (2015) [15] | India | 30 years Male | Mandible | - | + | - | | Extraoral draining sinus | + |
| Kodati S et al., (2016) [16] | India | 16 years Male | Mandible | - | + | _ | _ | Ulceration | Unknown |
| 33 years Female | Mandible | + | + | _ | _ | Bleeding and difficulty in mouth openingIn the extraction site | + |
| 25 years Male | Mandible | - | + | - | - | Mobility of the anterior teeth | Unknown |
| Aoki T et al., (2018) [5] | Japan | 80-year-old man | Maxilla | - | + | | - | Trismus and nasal congestion | + |
| Landeen K et al., (2019) [17] | USA | 27 years Female | Mandible | + | - | - | - | Nasal discharge, nasal dyspnoea | + |
| Cho BH et al., (2020) [2] | Korea | 45 years Male | Mandible | - | + | - | - | Abnormal extracted site | + |
| Ogane S et al., (2023) [3] | Japan | 72 years Female | Mandible | + | - | + | - | Ulceration | + |
| Sowmya (2024) | India | 40 years Male | Mandible | + | + | + | + | Abnormal extraction site, necrotic bone | + |
According to Ogane S et al., the diagnosis rate was difficult, accounting for about 39% [3]. In the past 10 years, 13 (61.9%) out of 21 cases were diagnosed as benign tumours. On the other hand, 7 cases (33.3%) were diagnosed as malignant tumours.
Histopathologic features of ameloblastic carcinoma include pleomorphism, fission, focal necrosis, perineural invasion and hyperchromasia of the nuclei. In addition to these, Hall et al., reported the absence of a central stellate reticular region and the presence of epithelial cell aggregates, cytosolic plexiform or insular patterns, hyperchromatin, dense cellular arrangement, atypical nucleoli, focal necrosis and neural and vascular invasion, which can make it difficult to distinguish from ameloblastoma [18].
Surgical resection is the first choice for treatment, followed by reconstruction. Postoperative radiation therapy is beneficial in some cases with invasive behaviour and positive margins. In the present case, based on clinical, radiographic and histopathological changes, resection of the mandible, preserving the condyles, followed by reconstruction and later postoperative radiotherapy, can be advised, as the lesion was aggressive. Furthermore, various radiotherapy devices, such as the gamma knife, helical tomotherapy and carbon ion therapy, have been developed. Recent advancements in molecular biological techniques have improved tumour therapy [6].
The survival rate is about five years in 69.1-83.2% of cases, which is relatively high, but it decreases to 0-21.4% in metastatic cases. The recurrence rate is about 20.9-38.4%. As for distant metastases, the lungs are the predominant site, with an incidence of 15.4-22.0% [3]. Ameloblastic carcinoma has a higher chance of recurrence or distant metastasis; thus, long-term follow-up is mandatory. Therefore, early-stage diagnosis, close periodic screening for metastasis and adequate treatment are necessary to improve patient prognosis.
Conclusion(s)
Ameloblastic carcinoma is a rare entity with no classic symptoms. It exhibits a range of clinical and radiographic manifestations, varying from benign to malignant. Ameloblastic carcinoma can present with rapid growth, pain, paresthesia, trismus, mobility, ulceration, or severe cortical bone resorption and it can potentially be lethal. In the present case, an abnormal extracted socket was observed along with necrotic bone and evident pus discharge. Therefore, alongside clinical and radiographic investigations, a prompt histopathological investigation is necessary. Early diagnosis and close periodic screening for recurrence and metastasis are essential for a better prognosis.
[1]. Elzay RP, Primary intraosseous carcinoma of the jaws Review and update of odontogenic carcinomasOral Surg Oral Med Oral Pathol 1982 54:299-303.10.1016/0030-4220(82)90099-86957827 [Google Scholar] [CrossRef] [PubMed]
[2]. Cho BH, Jung YH, Hwang JJ, Ameloblastic carcinoma of the mandible: A case reportImaging Sci Dent 2020 50(4):359-63.Available from: https://doi.org/10.5624/isd.2020.50.4.35910.5624/isd.2020.50.4.35933409146 [Google Scholar] [CrossRef] [PubMed]
[3]. Ogane S, Fujii A, Suzuki T, Hashimoto K, Hashimoto S, Takano M, Ameloblastic carcinoma of the mandible: A case reportMaxillofac Plast Reconstr Surg 2023 45:17Available from: https://doi.org/10.1186/s40902-023-00380-y10.1186/s40902-023-00380-y37101080 [Google Scholar] [CrossRef] [PubMed]
[4]. Li J, Du H, Li P, Zhang J, Tian W, Tang W, Ameloblastic carcinoma: An analysis of 12 cases with a review of the literatureOncol Letters 2014 8:914-20.Available from: https://doi.org/10.3892/ol.2014.223010.3892/ol.2014.223025013517 [Google Scholar] [CrossRef] [PubMed]
[5]. Aoki T, Akiba T, Kondo Y, Sasaki M, Kajiwara H, Ota Y, The use of radiation therapy in the definitive management of ameloblastic carcinoma: A case reportOral Surg Oral Med Oral Pathol Oral Radiol 2019 127(2):e56-e60.10.1016/j.oooo.2018.09.00930393089 [Google Scholar] [CrossRef] [PubMed]
[6]. Augustine D, Sekar B, Murali S, Large ameloblastic carcinoma: A rare case with managementDent Res J (Isfahan) 2013 10(6):809-12. [Google Scholar]
[7]. Roy S, Garg V, Alpha smooth muscle actin expression in a case of ameloblastic carcinoma: A case reportJ Oral Maxillofac Res 2013 4(1):e410.5037/jomr.2013.410424422027 [Google Scholar] [CrossRef] [PubMed]
[8]. Sozzi D, Morganti V, Valente GM, Moltrasio F, Bozzetti A, Angiero F, Ameloblastic carcinoma in a young patientOral Surg Oral Med Oral Pathol Oral Radiol 2014 117(5):e396-e402.10.1016/j.oooo.2013.08.01224184061 [Google Scholar] [CrossRef] [PubMed]
[9]. Srikanth MD, Radhika B, Metta K, Renuka NV, Ameloblastic carcinoma: Report of a rare caseWorld J Clin Cases 2014 2(2):48-51.10.12998/wjcc.v2.i2.4824579073 [Google Scholar] [CrossRef] [PubMed]
[10]. Yunaev M, Abdul-Razak M, Coleman H, Mayorchak Y, Kalnins I, A rare case of ameloblastic carcinomaEar Nose Throat J 2014 93(9):E34-E36.10.1177/01455613140930090825255357 [Google Scholar] [CrossRef] [PubMed]
[11]. Dutta M, Kundu S, Bera H, Barik S, Ghosh B, Ameloblastic carcinoma of mandible: Facts and dilemmasTumouri 2014 100(5):e189-e96.Available from: https://doi.org/10.1700/1660.1819010.1177/1660.18190 [Google Scholar] [CrossRef]
[12]. Kallianpur S, Jadwani S, Misra B, Sudheendra US, Ameloblastic carcinoma of the mandible: Report of a case and reviewJ Oral Maxillofac Pathol 2014 18(Suppl 1):S96-S102.Available from: https://doi.org/10.4103/0973-029X.14133610.4103/0973-029X.14133625364189 [Google Scholar] [CrossRef] [PubMed]
[13]. Owosho AA, Potluri A, Bauer Iii RE, Bilodeau EA, Ameloblastic carcinoma of the mandible manifesting as an infected odontogenic cystGen Dent 2015 63(1):e1-4. [Google Scholar]
[14]. Matsushita Y, Fujita S, Yanamoto S, Yamada S, Rokutanda S, Yamashita K, Spindle cell variant of ameloblastic carcinoma: A case report and literature reviewOral Surg Oral Med Oral Pathol Oral Radiol 2016 121(3):e54-e61.10.1016/j.oooo.2015.06.03426238174 [Google Scholar] [CrossRef] [PubMed]
[15]. Kishore M, Panat SR, Aggarwal A, Upadhyay N, Agarwal N, Amelo blastic carcinoma: A case reportJ Clin Diagn Res 2015 9(7):ZD27-ZD28.Available from: https://doi. org/10.7860/JCDR/2014/8246.6248 [Google Scholar]
[16]. Kodati S, Majumdar S, Uppala D, Namana M, Ameloblastic carcinoma: A report of three casesJ Clin Diagn Res 2016 10(10):ZD23-ZD25.Available from: https://doi.org/10.7860/JCDR/2016/21100.869710.7860/JCDR/2016/21100.869727891485 [Google Scholar] [CrossRef] [PubMed]
[17]. Landeen K, Spanos WC, Powell S, A rare presentation of ameloblastic carcinoma of the sinus cavity and skull baseCureus 2019 11(12):e626510.7759/cureus.626531903302 [Google Scholar] [CrossRef] [PubMed]
[18]. Hall JM, Weathers DR, Unni KK, Ameloblastic carcinoma: An analysis of 14 casesOral Surg Oral Med Oral Pathol Oral Radiol Endod 2007 103:799-807.Available from: https://doi.org/10.1016/j.tripleo.2006.11.04810.1016/j.tripleo.2006.11.04817448710 [Google Scholar] [CrossRef] [PubMed]