Retrosternal goitres, often due to longstanding thyroid enlargement, can compress critical structures like the trachea and oesophagus, necessitating thyroidectomy. Managing the airway while ensuring patient safety presents a significant challenge for anaesthesiologists. This case series explores the complex airway management in three patients with large retrosternal goitres undergoing total thyroidectomy. The patients, aged 50, 60, and 73, presented with long-standing neck swelling, tracheal deviation and symptoms including breathlessness, dysphagia and hoarseness of voice. The goitres had progressively enlarged over many years, leading to significant tracheal compression and deviation, which posed a high-risk for airway obstruction during surgery. Given these challenges, Awake Fiberoptic Intubation (AFOI) was chosen to secure the airway while minimising the risk of airway loss. AFOI was performed under conscious sedation with dexmedetomidine and local anaesthesia, providing effective intubation with minimal discomfort and stable haemodynamics. This approach was critical in managing the anticipated difficult airway due to the retrosternal extension of the goitres and their impact on surrounding structures. Postoperatively, the patients were kept intubated to prevent tracheomalacia, a potential complication arising from prolonged tracheal compression. Tracheomalacia, characterised by the weakening of tracheal walls, can lead to airway collapse after extubation. To ensure airway stability, extubation was delayed until a satisfactory cuff-leak test was performed 24-36 hours after surgery. This case series emphasises the importance of careful preoperative planning and the use of AFOI in managing patients with large retrosternal goitres to avoid a ‘can’t intubate, can’t ventilate’ situation. The successful management of these cases highlights the effectiveness of AFOI in reducing perioperative risks and ensuring patient safety, particularly in scenarios where difficult airway management is anticipated. By implementing appropriate postoperative protocols, the risk of complications such as tracheomalacia can be significantly reduced, leading to improved surgical outcomes.
Introduction
Managing large retrosternal goitres presents a significant challenge, particularly concerning airway management during surgery. These goitres are often the result of longstanding thyroid enlargement and can extend into the mediastinum, causing compression of critical structures like the trachea and oesophagus. Patients with such goitres may present with pressure symptoms, including breathlessness, difficulty in swallowing, and voice changes, all of which signal potential airway compromise [1]. In the context of surgical intervention, particularly total thyroidectomy, securing the airway becomes a paramount concern. The risks associated with tracheal compression and deviation necessitate careful preoperative planning and the use of specialised techniques. AFOI is often preferred in these cases, as it allows for safe and controlled airway management, minimising the risks of airway obstruction during induction [2]. Postoperatively, managing these patients is equally critical, particularly in monitoring for tracheomalacia-a condition where the tracheal walls become weakened due to prolonged compression, potentially leading to airway collapse after extubation. To mitigate this risk, patients may be kept intubated for an extended period, with extubation only performed after confirming airway stability through a cuff-leak test [3]. This case series explores the perioperative and postoperative strategies employed in three patients with large retrosternal goitres, highlighting the importance of meticulous management to ensure patient safety and optimise surgical outcomes.
Case Series
Case 1
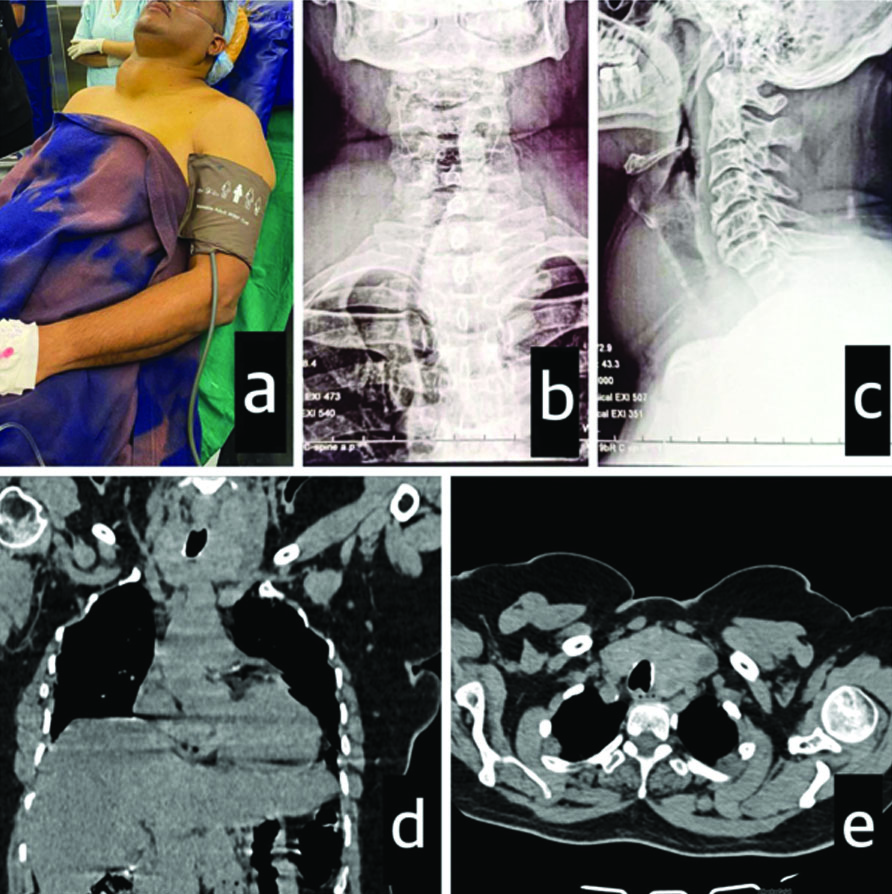
A 50-year-old male patient with a BMI of 30 kg/m2 presented with a large midline neck swelling that had progressively increased over the past 10 years [Table/Fig-1a]. For the past two months, he has been experiencing breathlessness when supine. He was diagnosed with hypertension one month ago and was started on tablet Telmisartan 40 mg+Amlodipine 5 mg once daily. He had no other co-morbidities. Physical examination revealed a firm, nodular neck swelling that moved with deglutition. It was not possible to palpate below the swelling. The trachea was deviated to the right. Airway examination revealed difficult mask ventilation and intubation due to a heavy jaw and Mallampati grade III. Neck flexion was limited due to the swelling, but extension was normal. Indirect laryngoscopy showed normal vocal cords. Thyroid Function Tests (TFT) were normal. Ultrasonography showed a large multinodular goitre compressing the trachea. X-rays of the chest and neck showed tracheal deviation to the right and compression [Table/Fig-1b,c]. Computed Tomography (CT) of the neck revealed a 6×7 cm lesion in the right lobe of the thyroid, a 3×5 cm lesion involving the isthmus, and a 7×8 cm lesion arising from the left lobe with retrosternal extension, compressing and displacing the trachea to the right [Table/Fig-1d,e].
Case 1: a) Patient with swelling on the anterior aspect of neck; b) X-ray neck anteroposterior view; c) X-ray neck lateral view; d) CT neck coronal view; e) CT neck axial view.
Case 2
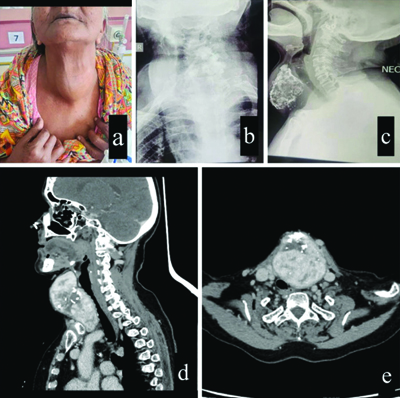
A 73-year-old female presented with a progressively enlarging midline neck swelling for 30 years, associated with breathlessness in the supine position and dysphagia for three months. She had no other co-morbidities. Physical examination revealed a multinodular swelling on the anterior aspect of the neck that moved with deglutition and extended retrosternally [Table/Fig-2a]. Airway examination revealed a Mallampati grade II. Neck movements were normal. Video laryngoscopy showed normal vocal cords. Thyroid function tests were normal. An X-ray of the neck revealed tracheal deviation to the right [Table/Fig-2b,c]. CT of the neck confirmed a lobulated multinodular lesion (9.8×7×8.4 cm) arising from the isthmus and left lobe of the thyroid gland, with retrosternal extension abutting the left common carotid artery, internal jugular vein, and brachiocephalic vein. It also showed displacement of the larynx, trachea, and oesophagus towards the right [Table/Fig-2d,e].
Case 2: a) Patient with swelling on the anterior aspect of the neck; b) X-ray neck anteroposterior; c) X-ray neck lateral; d) CT neck sagittal view; e) CT neck axial view.
Case 3
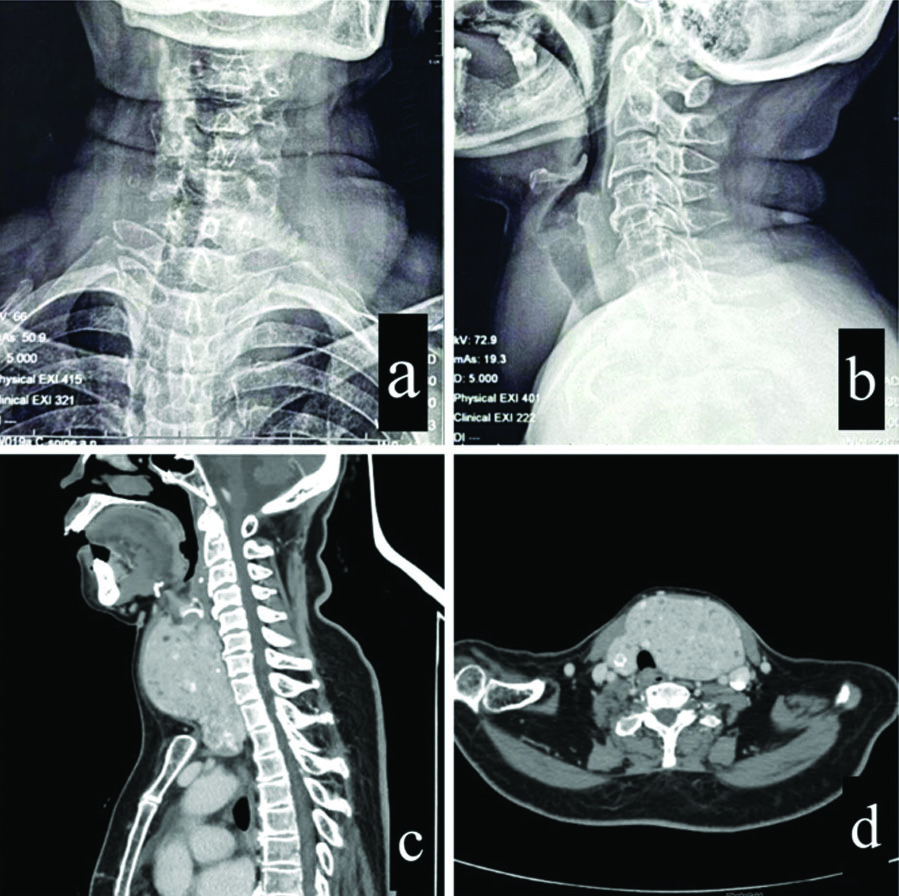
A 60-year-old woman presented with a midline neck swelling that had progressively increased over the past 15 years. For the past month, this swelling had been accompanied by dysphagia and hoarseness of voice. She did not report any other pressure symptoms such as dyspnoea, dysphagia, or stridor. She had no other co-morbidities. Physical examination revealed a multinodular swelling that moved with deglutition. It was not possible to palpate beneath the swelling. There was a deviation of the trachea towards the right. Neck flexion was restricted due to the swelling, but extension was normal. Video laryngoscopy showed normal vocal cords. Thyroid function tests were normal. X-ray of the neck showed right tracheal deviation and compression [Table/Fig-3a,b]. CT of the neck revealed a multinodular goitre, with the left lobe of the thyroid markedly enlarged, measuring 12 × 5 × 8 cm, extending retrosternally, and causing mediastinal shift to the right. There was narrowing of the trachea along with displacement of the trachea, larynx, and oesophagus to the right. It was abutting and displacing the left common carotid artery and internal jugular vein [Table/Fig-3c,d].
Case 3: a) X-ray neck anteroposterior view; b) X-ray neck lateral view; c) CT meck sagittal view; d) CT neck axial view.
In all three cases, patients had symptomatic long-standing goitres and were scheduled for total thyroidectomy under general anaesthesia with planned AFOI. Written informed consent was obtained, and the risks of prolonged ventilation and Intensive Care Unit (ICU) stay were explained. Adequate blood and blood products were reserved. Two 18G cannulas were inserted. The patients were positioned on the operating table in a semirecumbent position to prevent desaturation due to tracheal compression that could occur in the supine position [Table/Fig-1a]. Standard monitors were attached, and vital signs were noted. Glycopyrrolate 0.2 mg was given intramuscularly as premedication 30 minutes before induction to reduce salivary gland and respiratory tract secretions. The patients were nebulised with 2 mL of 4% lignocaine and 20 μg dexmedetomidine. Nasal packing with 2% lignocaine-adrenaline and xylometazoline hydrochloride 0.1% drops was performed. A 10% lignocaine solution was sprayed on the posterior pharyngeal wall with the help of a tongue depressor. Conscious sedation was achieved with dexmedetomidine infusion at a rate of 0.2-0.3 μg/Kg/h. Nasal fiberoptic intubation was successfully performed using a flexometallic tube while spraying 4% lignocaine (spray-as-you-go technique) via a fiberoptic drug port to prevent reflexes. After confirming the correct placement of the endotracheal tube (through direct visualisation, chest auscultation, and capnography), intravenous fentanyl 2 μg/kg was administered, and the patients were induced with propofol 2 mg/kg. Maintenance was achieved with sevoflurane and vecuronium. A left radial arterial line was inserted for meticulous haemodynamic monitoring. Paracetamol 1 g and tramadol 50 mg were administered intravenously.
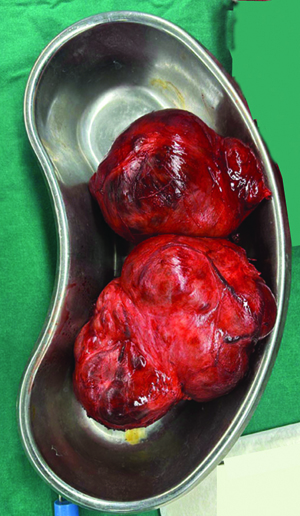
Total thyroidectomy was successfully performed, and the patients remained haemodynamically stable throughout the procedure [Table/Fig-4]. After surgery, the patients were kept intubated due to the potential risk of tracheomalacia and were transferred to the ICU. On the first postoperative day, a successful T-piece trial was followed by extubation after a satisfactory cuff-leak test of more than 110 mL (or >10% of the tidal volume) [4].
Thyroid specimen: Case 1- post thyroidectomy.
Discussion
Thyroid goitres can be associated with pressure symptoms and signs such as dyspnoea (exertional or positional), stridor, cough (often positional), choking sensation, hoarseness (due to recurrent laryngeal nerve compression), dysphagia, phrenic nerve palsy, Horner’s syndrome, and superior vena cava syndrome. Retrosternal goitres often cause tracheal deviation and compression, but they are not always associated with obstructive symptoms [1]. Thyroidectomy is often necessary to relieve symptoms such as compression of nearby structures, thyroid dysfunction, or suspected malignancy [5]. Managing the airway while ensuring patient safety presents a significant challenge for anaesthesiologists when dealing with large-sized goitres. The reported incidence of difficult intubation during thyroid surgery is 11.1% of cases [6]. Difficult airway was anticipated in present series patients due to the large goitre extending into the retrosternal space, compressing and deviating the trachea, oesophagus, and larynx from the midline. Airway manipulation by surgeons, along with potential airway compromise during induction, intubation, and the intraoperative and postoperative phases, can collectively contribute to cardiovascular and respiratory adverse events [7].
Direct mechanical pressure on the trachea or main bronchi from the goitre may lead to complete airway obstruction, while external compression on major vessels, such as the superior vena cava, pulmonary artery, or even the heart, could lead to cardiovascular collapse, potentially resulting in fatal outcomes [8]. Anticipating difficult mask ventilation and intubation due to a bulky goitre, authors opted against direct laryngoscopy. With a large goitre, the induction of anaesthesia may cause the soft palate and epiglottis to collapse onto the posterior pharyngeal wall, further complicating airway management by limiting space for bronchoscope maneuvering and obstructing visualisation [9]. In such scenarios, AFOI offers the advantage of a low potential for airway loss [2]. Awake intubation maintains the natural airway, allows for spontaneous ventilation, and protects against the risk of reflux [10]. Moreover, tracheostomy is hindered by a large, highly vascular thyroid gland [11].
The discomfort experienced during airway manipulation in awake patients is undesirable, given its potential to cause haemodynamic compromise in these patients. Utilising a local-sedative approach, AFOI stands out as a safe and efficient method for managing anticipated difficult airways with minimal discomfort and significant haemodynamic stability [12,13]. Authors employed a combination of methods to effectively anaesthetise the upper airway [14]. This included nebulisation with lignocaine and dexmedetomidine, nasal packing with lignocaine-adrenaline, and the use of xylometazoline hydrochloride drops in the nostrils. Lignocaine spray was also used as described above. Nerve blocks such as the transtracheal block could not be performed due to poor anatomical landmarks caused by a large thyroid mass. Dexmedetomidine infusion was used for conscious sedation, as it does not cause respiratory depression. This helped reduce patient anxiety, discomfort, and pain while allowing the patient to remain awake and responsive.
Thus, in present series patients, mild sedation and local anaesthesia facilitated a smooth intubation without any respiratory compromise. Patil VH et al., also stated in their study that awake fiberoptic intubation using a local anaesthesia-sedation technique is a suitable option for a selected group of patients with a potential for airway obstruction [12]. According to a study by Ghai A et al., AFOI should be planned in cases of significant airway obstruction [15]. Bhiwal AK et al., as well as Raval CB and Rahman SA, mentioned in their study that AFOI in cases of large retrosternal goitres can prevent a “can’t ventilate and can’t intubate” situation that can occur after the induction of anaesthesia due to complete tracheal collapse. They also highlighted the importance of awake extubation, considering it as important as awake intubation, especially when the goitre is chronic [10,16]. Srivastava D and Dhiraaj S also reported a case of successful fiberoptic intubation using a loco-sedative technique in a patient with a longstanding huge goitre who had a history of failed intubations in the past with direct laryngoscopy [17].
Considering the risk of cardiovascular decompensation and expected blood loss, it is advisable to employ invasive haemodynamic monitoring through the placement of an arterial catheter. Additionally, ensuring the availability of sufficient blood and blood products is essential [18]. Numerous complications can arise post-thyroidectomy, such as airway oedema, haemorrhage, stridor due to vocal cord palsy, and tracheomalacia [19]. All of the patients had a history of longstanding goitre. Prolonged compression of the trachea by a large goitre can lead to the atrophy and erosion of tracheal rings. Risk factors contributing to post-thyroidectomy tracheomalacia include a history of goitre for over five years, tracheal narrowing or deviation, retrosternal extension of the goitre, preoperative recurrent laryngeal nerve palsy, challenging tracheal intubation, and thyroid malignancy [20]. Following extubation, this can result in anterior-posterior collapse of the trachea due to loss of support from surrounding tissues, leading to desaturation [21]. Typically, this is a self-resolving condition as the strength of the tracheal wall is restored after relieving pressure [5]. Studies have reported varying rates of tracheomalacia following thyroidectomy in patients with large goitres, ranging from 0 to 5.3%, and in some instances, as high as 10% [5,22,23]. Thorough preoperative assessments and appropriate postoperative measures can significantly diminish the occurrence of post-thyroidectomy tracheomalacia. One study suggests delaying extubation for 36 hours to prevent tracheomalacia [3]. Present study maintained the patients in an intubated state as a preventive measure against tracheomalacia. After a satisfactory cuff-leak test 24-36 hours postsurgery (>110 mL or >10% of tidal volume), the patients were extubated uneventfully [4,17].
Conclusion(s)
In patients with large goitres, securing the airway poses significant challenges. AFOI offers a reliable approach with minimal risk of airway loss, ensuring patient comfort and stable haemodynamics. Combining mild sedation with local anaesthesia facilitates smooth intubation without compromising respiratory function. Proper postoperative protocols, including delayed extubation and a cuff leak test, help reduce the risk of post-thyroidectomy tracheomalacia. These strategies enable anaesthesiologists to manage airway difficulties effectively, prioritising patient safety and improving surgical outcomes.
[1]. Kleyenstuber T, Anaesthesia for retrosternal thyroidectomySouth Afr J Anaesth Analg 2022 28(5 Suppl 1):S193-S196.10.36303/SAJAA.2022.28.5.2880 [Google Scholar] [CrossRef]
[2]. Rajan H, Jacob A, Anaesthetic management of retrosternal thyroid: A case reportKerala Med J 2024 17(1):49-51.10.52314/kmj.2024.v17i1.633 [Google Scholar] [CrossRef]
[3]. Shaikh SI, Atlapure BB, Airway challenges in thyroid surgeryKarnataka Anaesth J 2015 1:28-30.10.4103/2394-6954.149717 [Google Scholar] [CrossRef]
[4]. Paulo L, Silva EM, Rego S, Lima MH, Carreira C, Costa G, Positive cuff leak test in a patient with post-extubation stridor after total thyroidectomy: How to deal with it?Revista da Sociedade Portuguesa de Anestesiologia 2018 27(4):108-11. [Google Scholar]
[5]. Kaur H, Kataria AP, Muthuramalingapandian M, Kaur H, Airway considerations in case of a large multinodular goiterAnaesth Essays Res 2017 11(4):1097-100.PMCID: PMC573545910.4103/aer.AER_86_1629284884 [Google Scholar] [CrossRef] [PubMed]
[6]. Amathieu R, Smail N, Catineau J, Poloujadoff MP, Samii K, Adnet F, Difficult intubation in thyroid surgery: Myth or reality?Anaesth Analg 2006 103:965-68.10.1213/01.ane.0000237305.02465.ee17000813 [Google Scholar] [CrossRef] [PubMed]
[7]. Kamath S, Naik S, Pratiksha N, Retrosternal goitre- an anaesthetic challengeJ Clin Diagn Res 2019 13:01-03.10.7860/JCDR/2019/38445.12565 [Google Scholar] [CrossRef]
[8]. Olusomi BB, Aliyu SZ, Babajide AM, Sulaiman AO, Adegboyega OS, Gbenga HO, Goitre-related factors for predicting difficult intubation in patients scheduled for thyroidectomy in a resource-challenged health institution in North Central NigeriaEthiop J Health Sci 2018 28(2):169-76.10.4314/ejhs.v28i2.829983514 [Google Scholar] [CrossRef] [PubMed]
[9]. Nandi PR, Charlesworth CH, Taylor SJ, Nunn JF, Doré CJ, Effect of general anaesthesia on the pharynxBr J Anaesth 1991 66:157-62.10.1093/bja/66.2.1571817614 [Google Scholar] [CrossRef] [PubMed]
[10]. Bhiwal AK, Patidar NC, Desai SH, Mandot P, Anaesthetic challenges for total thyroidectomy in a patient with large thyroid mass with retrosternal extension: A case reportDev Anaesth Pain Manag 2023 2(4):DAPM.00054210.31031/DAPM.2023.02.000542 [Google Scholar] [CrossRef]
[11]. Dempsey GA, Snell JA, Coathup R, Jones TM, Anaesthesia for massive retrosternal thyroidectomy in a tertiary referral centreBr J Anaesth 2013 111:594-99.10.1093/bja/aet15123690528 [Google Scholar] [CrossRef] [PubMed]
[12]. Patil VH, Huddar KS, Barsagade WS, Rao AU, Airway management of huge thyroid swelling having tracheal deviation: Challenges facedIndian J Clin Anaesth 2022 9(4):514-17.10.18231/j.ijca.2022.103 [Google Scholar] [CrossRef]
[13]. Shamim F, Yahya M, Ikram M, Awake fiberoptic intubation in a patient with known difficult airway due to huge thyroid goiterAnaesth Pain Intensive Care 2017 21(1):94-97. [Google Scholar]
[14]. Pani N, Rath SK, Regional & topical anaesthesia of the upper airwaysIndian J Anaesth 2009 53(6):641-48. [Google Scholar]
[15]. Ghai A, Hooda S, Wadherra R, Garg N, Gross tracheal deviation: Airway challenges and concerns-two case reportsActa Anaesthesiol Belg 2011 62:203-06. [Google Scholar]
[16]. Raval CB, Rahman SA, Difficult airway challenges-intubation and extubation matters in a case of large goiter with retrosternal extensionAnaesth Essays Res 2015 9(2):247-50.10.4103/0259-1162.15242126417136 [Google Scholar] [CrossRef] [PubMed]
[17]. Srivastava D, Dhiraaj S, Airway management of a difficult airway due to prolonged enlarged goiter using loco-sedative techniqueSaudi J Anaesth 2013 7(1):86-89.PMCID: PMC365793410.4103/1658-354X.10982923717240 [Google Scholar] [CrossRef] [PubMed]
[18]. Choudhary N, Kumar A, Wadhawan S, Bhadoria P, Panwar V, Retrosternal goitre: Anaesthetic implications and managementIndian J Clin Anaesth 2018 5(3):453-56.10.18231/2394-4994.2018.0085 [Google Scholar] [CrossRef]
[19]. Valizadeh N, Mohammadi P, Mahmodlou R, Seyed Mokhtari SA, Ramezani G, Tracheomalacia after thyroidectomy: Does it truly exist?Niger J Surg 2020 26(1):59-62.10.4103/njs.NJS_31_1932165838 [Google Scholar] [CrossRef] [PubMed]
[20]. Wong P, Liew GH, Kothandan H, Anaesthesia for goitre surgery: A reviewProc Singapore Healthc 2015 24:165-70.10.1177/2010105815596095 [Google Scholar] [CrossRef]
[21]. Pan Y, Chen C, Yu L, Zhu S, Zheng Y, Airway management of retrosternal goiters in 22 cases in a tertiary referral centerTher Clin Risk Manag 2020 16:1267-73.10.2147/TCRM.S28170933376336 [Google Scholar] [CrossRef] [PubMed]
[22]. Findlay JM, Sadler GP, Bridge H, Mihai R, Post-thyroidectomy tracheomalacia: Minimal risk despite significant tracheal compressionBr J Anaesth 2011 106:903-06.10.1093/bja/aer06221450708 [Google Scholar] [CrossRef] [PubMed]
[23]. Ayandipo O, Adigun T, Afuwape O, Airway complications and outcome after thyroidectomy in Ibadan: A 15 year reviewArch Med 2016 8:410.21767/1989-5216.1000151 [Google Scholar] [CrossRef]