Almost 85% of women experience some form of perineal trauma during vaginal birth, with the incidence of anal sphincter injury ranging from 0.5% to 7% [1]. Perineal tears can lead to significant postpartum complications, both short-term and long-term, including psychological effects. Short-term complications may include pain, discomfort, increased blood loss, haematoma and infections. Long-term complications can involve chronic infections, urinary, faecal and flatus incontinence, sexual dysfunction and pelvic organ prolapse [2]. Risk factors for perineal tears include Asian ethnicity, nulliparity, occiput-posterior position, shoulder dystocia, prolonged second stage of labour, instrumental delivery and higher birth weight [3]. A short perineal length of less than 35 mm has been associated with an increased risk of perineal tears [4].
Materials and Methods
A prospective cohort study was conducted in the Department of Obstetrics and Gynaecology at GTB Hospital, New Delhi, India, from January 2021 to April 2022. Ethical clearance was obtained from the Institutional Ethical Committee for human research (IECHR/2020/PG/47/42) and informed consent was obtained from the subjects.
After an extensive search, the authors found one study that was indirectly related, which provided a guiding number for the sample size [11].
Inclusion and Exclusion criteria: Primigravida patients with singleton pregnancies at ≥37 weeks in early labour were included in the study, while those with a history of pelvic floor trauma/surgery, instrumental delivery and malpresentation were excluded. Group 1 patients were defined as females sustaining ≥2nd degree perineal tears (including episiotomy, n=80), while group 2 patients were females with an intact perineum or sustaining up to 1st-degree perineal tears post-vaginal delivery (n=80).
Study Procedure
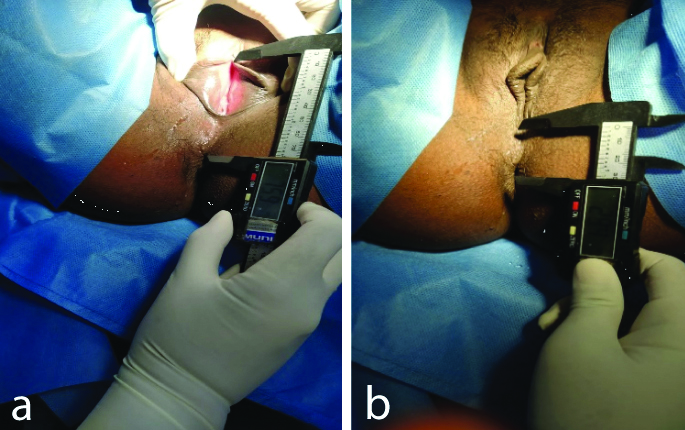
Anthropometric data such as AGDac (anus to clitoris) and AGDaf (anus to fourchette), along with labour parameters like foetal position, duration of the second stage, induction of labour and birth weight, were noted. AGD measurements were taken using digital vernier callipers by the same observer between contractions, with patients in the lithotomy position and thighs at an angle of 45 degrees to the examination table [Table/Fig-2]. Each measurement was taken three times and the average for each AGD was calculated. The recruitment strategy has been summarised in the flowchart [Table/Fig-3].
Anogenital Distance (AGD) and vernier caliper. a) Anus to clitoris (AGDac); b) Anus to fourchette (AGDaf).
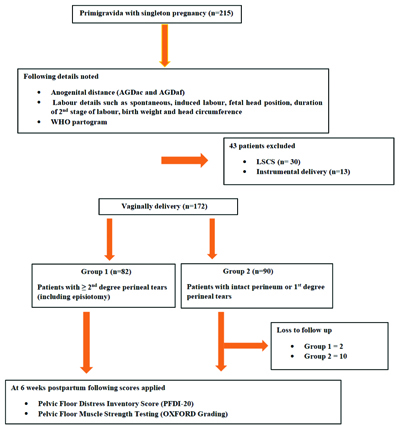
Follow-up of the subjects was conducted at 6 weeks postpartum in the postnatal clinic, where the PFDI and pelvic floor muscle strength testing were performed to assess pelvic floor function. Of the 20 questions in the PFDI-20 form, each question had "yes" or "no" as potential answers. A "no" response corresponded to a score of "0." If the patient answered "yes," the response was based on an ordinal range from "1" to "4" in terms of bother and severity of symptoms [13].
For pelvic floor muscle strength testing, the examination was carried out after the patient emptied their bladder in a dorsal lithotomy position with knees semi-flexed. Patients were requested to contract the muscles of the pelvic floor and their responses were graded from 0 to 5 according to a validated Oxford scale [14].
Statistical Analysis
Statistical analysis was performed using Statistical Package for Social Sciences (SPSS) version 22.0. The receiver operating characteristic curve was plotted to calculate the optimum cut-off values for AGD (AGDac and AGDaf). All continuous and categorical parameters were compared using an unpaired t-test and Chi-square test, respectively. Logistic regression analysis was conducted to identify the risk factors for the likelihood of perineal tears. A p-value of less than 0.05 was considered significant.
Results
Demographic characteristics such as age, socioeconomic status, religion, education and Basic Metabolic Index (BMI) (kg/m2) were comparable in group 1 and group 2 [Table/Fig-4]. The mean AGDac was shorter in group 1 compared to group 2, which was statistically significant (p-value of 0.029). Group 1 had a significantly shorter AGDaf compared to group 2 (p<0.001) [Table/Fig-5]. Second-degree perineal tears, including episiotomies, were the most common perineal outcomes, accounting for 86.25%, followed by Obstetric Anal Sphincter Injuries (OASIS) at 8.75% and cervical or paraurethral tears at 3.75% [Table/Fig-6].
Comparison of demographic profile in group 1 and 2.
| Parameters | Group 1 (n=80) | Group 2 (n=80) | p-value |
|---|
| Age (years) | 23.9±3.40 | 23.81±3.19 | 0.867* |
| Socioeconomic status | Upper middle | 0 | 2 (2.5%) | 0.311 |
| Lower middle | 59 (73.75%) | 57 (71.25%) |
| Upper lower | 16 (20%) | 19 (23.75%) |
| Lower | 5 (6.25%) | 2 (2.5%) |
| Religion | Hindu | 57 (71.25%) | 53 (66.25%) | 0.495# |
| Muslim | 23 (28.75%) | 27 (33.75%) |
| Education | Illiterate | 6 (7.5%) | 2 (2.5%) | 0.105# |
| Till 12th | 61 (76.25%) | 73 (91.25%) |
| Graduate | 13 (16.25%) | 4 (5%) |
| Postgraduate | 0 | 1 (1.25%) |
| BMI (pre-pregnancy, kg/m2) | 22.99 (1.40) | 23.12 (0.75) | 0.485* |
*: Age and BMI compared by unpaired t-test was; #: Chi-square test was used to socioeconomic status, religion and education
Anthropometric measurements in group 1 and 2.
| Parameters | Group 1 (mean±CI) | Group 2 (mean±CI) | p-value |
|---|
| Mean AGDac (mm) | 75.99±3.43 | 77.05±2.62 | 0.029 |
| Mean AGDaf (mm) | 33.50±1.65 | 34.52±1.25 | <0.001 |
Unpaired t-test was used
Types of perineal tears sustained during vaginal delivery in group 1.
| Type of tear | n (%) |
|---|
| Second-degree perineal tear | Spontaneous | 0 |
| Episiotomy | 69 (86.25%) |
| Episiotomy with cervical tear | 1 (1.25%) |
| Third or fourth-degree perineal tear {Obstetric Anal Sphincter Injuries (OASIS)} | | 7 (8.75%) |
| Other tears (cervical or paraurethral tears) | | 3 (3.75%) |
The left occiput anterior foetal head position and baby birth weight were significantly associated with the occurrence of second-degree or higher perineal tears (p=0.016 and p=0.002) [Table/Fig-7]. Cut-off values obtained from the receiver operating curve [Table/Fig-8] for AGDac and AGDaf were 77.05 mm and 33.75 mm for predicting the occurrence of second-degree or higher perineal tears. However, AGDaf had better sensitivity (75%) and specificity (55%) for predicting these tears compared to AGDac [Table/Fig-9]. The cut-off values obtained from the receiver operating curve [Table/Fig-10] for AGDac and AGDaf were 77.15 mm and 33.25 mm for predicting OASIS. AGDac exhibited better specificity (51%), while AGDaf demonstrated better sensitivity (71.4%) for predicting OASIS [Table/Fig-11].
Comparison of labour parameters in group 1 and 2.
| Labour parameters | Group 1 (n=80) | Group 2 (n=80) | p-value | Odds ratio (95% CI) |
|---|
| Spontaneous labour | 41 (51.25%) | 37 (46.25%) | 0.527 | 0.669 (0.345-1.300) |
| Induction of labour | 39 (48.75%) | 43 (53.75%) |
| Foetal position | Left occiput posterior | 1 (1.25%) | 0 | 0.016 | - |
| Left occiput transverse | 17 (21.25%) | 4 (5%) | 0.0 (0) |
| Right occiput posterior | 2 (2.5%) | 1 (1.25%) | 0.189 (0.059-0.608) |
| Right occiput anterior | 10 (12.5%) | 18 (22.5%) | 0.470 (0.041-5.407) |
| Left occiput anterior | 50 (62.5%) | 57 (71.25%) | 1.695 (0.707-4.062) |
| Duration of second stage (min) | 24.56 (7.64) | 22.69 (7.37) | 0.116 | 0.967 (0.927-1.009) |
| Baby birth weight (kg) | 2.70 (0.38) | 2.50 (0.43) | 0.002 | 0.286 (0.125-0.652) |
| Head circumference (cm) | 33.43 (1.34) | 33.64 (1.51) | 0.351 | 1.111 (0.892-1.383) |
Logistic regression was used
Receiver operating characteristics curve for AGDac and AGDaf in predicting ≥Grade-2 perineal tears.
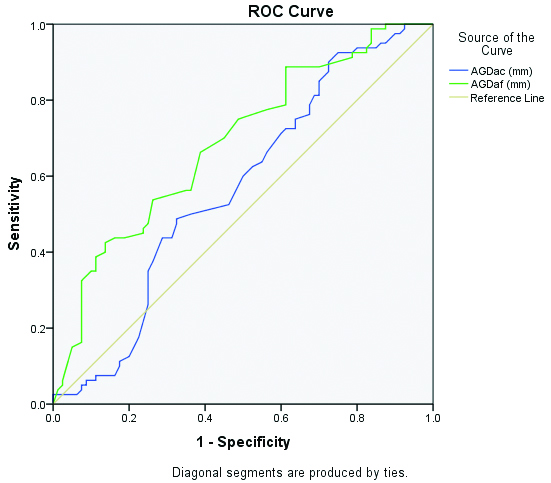
Receiver operating characteristic curve for AGDac and AGDaf in predicting ≥Grade-2 perineal tears.
| Parameters | Cut off | AUC | Sensitivity | Specificity | PPV | NPV |
|---|
| AGDac (mm) | 77.05 | 0.569 | 60.0% | 50.0% | 54.5% | 55.5% |
| AGDaf (mm) | 33.75 | 0.688 | 75.0% | 55.0% | 62.5% | 68.7% |
Receiver operating characteristic curve for AGDac and AGDaf in predicting (OASIS, Third and Fourth degree perineal tears).
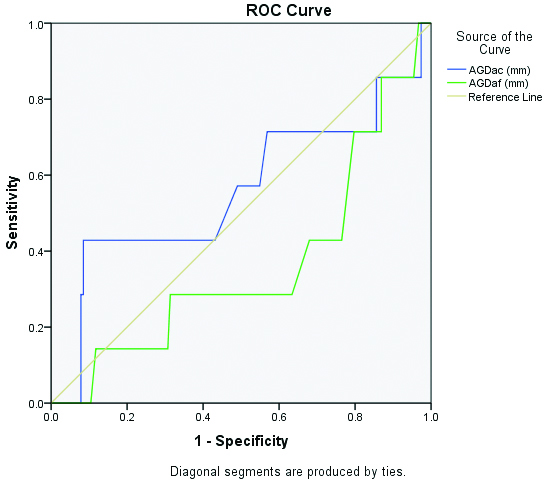
Receiver operating characteristic curve for AGDac and AGDaf in predicting Obstetric Anal Sphincter Injury Syndrome (OASIS, Third or Fourth degree perineal tears).
| Parameters | Cut off | AUC | Sensitivity | Specificity | PPV | NPV |
|---|
| AGDac (mm) | 77.15 | 0.558 | 57.1% | 51.0% | 5.29% | 96.13% |
| AGDaf (mm) | 33.25 | 0.361 | 71.4% | 20.3% | 4.11% | 93.68% |
At six weeks, patients in group 1 reported more bowel symptoms and symptoms pertaining to prolapse compared to group 2, while urinary symptoms were comparable in both groups, with no statistically significant difference found using the PFDI-20 [Table/Fig-12]. Pelvic floor muscle strength, assessed by Oxford grading, was found to be comparable in both groups.
Comparison of clinical tests in group 1 and 2 at six weeks postpartum.
| Clinical test | Group 1 (n=80) | Group 2 (n=80) | p-value |
|---|
| Pelvic Floor Distress Inventory (PFDI 20) | Pelvic Organ Prolapse Distress Inventory 6 (POPDI 6) | 1.13 (0.56) | 0.81 (0.58) | 0.001 |
| Colorectal Anal Distress Inventory 8 (CRAD 8) | 0.74 (0.69) | 0.51 (0.55) | 0.024 |
| Urinary Distress Inventory 6 (UDI 6) | 0.44 (0.50) | 0.45 (0.50) | 0.875 |
| Pelvic floor muscle strength testing (Oxford grading) | 3.16 (0.40) | 3.19 (0.39) | 0.692 |
Unpaired t-test was used
Discussion
The mean AGDac was lower in group 1 and higher in group 2 (75.99±3.43 mm vs. 77.05±2.62 mm, p=0.029). The mean AGDaf was also lower in group 1 and higher in group 2 (33.50±1.65 mm vs. 34.52±1.25 mm, p<0.001). Moya-Jiménez LC et al., conducted an observational prospective cohort study to compare perineal measurements {gh+pb, as per the Pelvic Organ Prolapse Quantification system (POP-Q)} and AGD to determine which perineal measurement can predict the likelihood of episiotomy. The gh+pb measurement was 77 mm in the episiotomy group and 81.9 mm in the no-episiotomy group, while its counterpart AGDac was 93.1±9.4 mm in the episiotomy group and 97.8±10.2 mm in the no-episiotomy group [11].
In the study conducted by Moya-Jiménez LC et al., the AGDaf was 35.9±6.9 mm and 34.9±7.4 mm in the episiotomy and no-episiotomy groups, respectively. They found that shorter lengths of gh+pb and AGDac were risk factors for episiotomy, which were comparable to the current study’s results.
Additionally, AGDac was found to be a more specific predictor of OASIS, while AGDaf was identified as a better predictor of ≥2nd-degree perineal tears and episiotomy [11]. These results were consistent with the current study.
A study conducted by Lane TL et al., assessed the relationship between perineal body length and perineal lacerations [4]. The mean perineal body length was 37±0.5 mm and the study concluded that a perineal body length of ≤35 mm was predictive of 3rd or 4th-degree lacerations. Geller EJ et al., conducted a study to determine whether a shortened perineal body is a risk factor for ultrasound-detected anal sphincter tears at first delivery and concluded that a perineal body length of <3 cm was associated with a significantly higher rate of tears [15].
The mean birth weight in group 1 was 2.7 kg and 2.5 kg in group 2 (p=0.002), which was statistically significant, suggesting it is significantly associated with the occurrence of second-degree or higher perineal tears. The study conducted by Marschalek ML et al., also found that birth weight was significantly associated with a high likelihood of perineal tears, similar to the results of the present study [3]. AGD is an emerging and lesser-explored area in obstetrics and Gynaecology. More studies should be conducted to fully understand its implications. Further studies are needed to validate these findings on a larger scale.
Limitation(s)
Only primiparous women were included, so the results cannot be generalised to multiparous women. Additionally, since this was a single-centre study, the findings cannot be generalised to the entire population.
Conclusion(s)
The shorter Anus to Fourchette Distance (AGDaf) has been found to have good sensitivity for predicting second-degree or higher perineal tears. In predicting Obstetric Anal Sphincter injury specifically, AGDaf demonstrated better sensitivity than the Anus to Clitoris Distance (AGDac); however, its specificity was lower than that of AGDac. Measuring AGD with vernier callipers in obstetric patients is simple and can be performed easily. If AGD is found to be short, along with the presence of risk factors for perineal tears, the obstetrician conducting the delivery can take more precautions. This can help reduce the occurrence of obstetric anal sphincter injuries and their long-term consequences.
Declaration: The present article is published as Abstract 181- Role of Maternal Anogenital Distance Measurement in Prediction of Perineal Tears during Vaginal Delivery, Continence, Volume 7, Supplement 1, 2023, 100899, ISSN 2772-9737. htt://doi.org/10.1016/j.cont.2023.100899.
*: Age and BMI compared by unpaired t-test was; #: Chi-square test was used to socioeconomic status, religion and education
Unpaired t-test was used
Logistic regression was used
Unpaired t-test was used