Atrial Septal Defect (ASD) is one of the most common acyanotic heart diseases presented in adults, with a higher prevalence among females. Patients often go unrecognised until middle age, unless complications such as arrhythmias arise. The physiological changes during pregnancy cause significant alterations in maternal haemodynamics. Cardiac valvular diseases, when present in obstetric patients, are among the leading causes of maternal mortality worldwide. These conditions pose a significant and unanticipated anaesthetic challenge, as the shunting of blood from left to right may precipitate hypoxia, hypercarbia, arrhythmias and cardiac failure. The presence of any other co-morbidities further complicates management. Hereby, the authors reported the successful management of a 30-year-old primigravida female at eight months of pregnancy, associated with a large ASD (34 mm), severe pulmonary hypertension, and preeclampsia, who underwent an elective Caesarean section (C-section). She presented at the Obstetric Emergency Department with dyspnoea at rest, which progressively deteriorated from the second month of pregnancy onward. She had no other complaints during her pregnancy. Echocardiography revealed a large Ostium Secundum ASD (OS-ASD) measuring 34 mm, almost leading to a single atrium physiology, with an ejection fraction of 45% and grossly dilated right atrium and right ventricle, as well as, severe Pulmonary Artery Hypertension (PAH). She underwent an elective Caesarean section with minimal haemodynamic alterations under fractionated spinal anaesthesia, with prophylactic adrenaline infusion. The effects were found to be beneficial and safe for the Caesarean section in patients with large ASD and preeclampsia.
Cardiac septal defect, Dose fractionation, Obstetric anaesthesia, Pregnancy
Case Report
A 30-year-old primigravida female presented to the Obstetric Emergency Department at eight months of pregnancy, associated with shortness of breath. On general examination, she exhibited dyspnoea at rest {New York Heart Association (NYHA) grade 4} while breathing room air, with an Oxygen Saturation (SpO2) of 87%. She was promptly started on oxygen therapy via a simple facial mask at 6 litres/min in a semi-recumbent position, which raised her SpO2 to 98% and provided some relief to her laboured breathing (respiratory rate: 20 breaths/min).
Auscultation revealed decreased air entry in both lungs, along with moderate crepitations at the bases. Her heart examination showed regular S1 and S2, with a grade 4 pansystolic murmur best heard at the left lower sternal border. Patient appeared pale and had grade 2 clubbing of the fingers on both hands, as well as, bilateral pitting oedema extending to the sacrum, with no cyanosis. Her Blood Pressure (BP) was recorded at 158/104 mmHg, and Heart Rate (HR) was 118 beats/min. The obstetrician diagnosed her with preeclampsia and administered an injection of labetalol 20 mg instantaneously. She was then started on oral labetalol 100 mg twice daily.
The patient had been well prior to her pregnancy and worked as a manual labourer with a Metabolic Equivalent (MET) of >4, without any signs or symptoms until pregnancy. Her respiratory distress began in the second month of pregnancy and gradually worsened as the pregnancy progressed (NYHA 1 to NYHA 4). She had not received any antenatal check-ups until presenting at the Emergency Department.
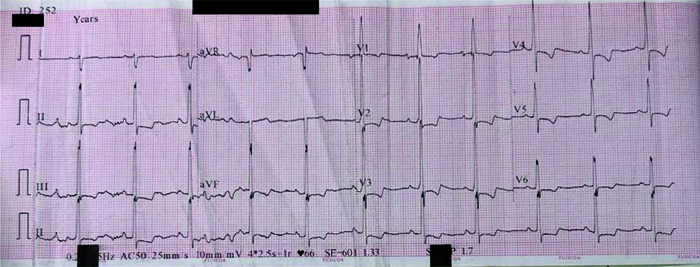
Investigations were within normal limits except for low platelet counts [Table/Fig-1]. An Electrocardiogram (ECG) revealed signs of right ventricular hypertrophy with right axis deviation [Table/Fig-2].
Routine investigations done for the patient.
| Parameters | Patient’s values | Normal range |
|---|
| Haemoglobin (gm%) | 15.7 | 12-14 |
| Platelets (/mm3) | 89,000 (low) | 1.5-4 lakhs |
| Blood urea (mg/dL) | 13 | 5-20 |
| Serum creatinine (mg/dL) | 0.8 | 0.7-1.3 |
| Serum sodium/serum potassium (milliequivalents/litre) | 138/4.2 | 135-145/3.5-5 |
| Prothrombin time (seconds) | 12.2 | 11-13.5 |
| INR (International Normalised Ratio) | 0.7 | <1.1 |
| Urinary protein | 2+ | Negative |
| Alanine aminotransferase (ALT) (unit/litre) | 24 | 10-40 |
| Aspartate aminotransferase (AST) (unit/litre) | 25 | 14-40 |
| Alkaline phosphatase (ALP) (unit/litre) | 87 | 40-125 |
| Total bilirubin (mg/dL) | 0.6 | 0.2-1.2 |
| Total protein (gm/dL) | 2.7 | 3.5-5.5 |
Patients ECG showing right axis deviation, right ventricular hypertrophy and crochetage sign.
A foetal ultrasonography scan revealed good foetal movement and ruled out placenta accreta. A cardiology opinion was sought regarding ECG changes, and an echocardiography was performed. The echocardiography revealed a large Ostium Secundum Atrial Septal Defect (OS-ASD) measuring 34 mm, almost leading to a single atrial physiology. The defect was associated with an ejection fraction of 45%, moderate to severe Tricuspid Regurgitation (TR) (Right Ventricular Systolic Pressure (RVSP)=82 mmHg+right atrial pressure), moderate Pulmonary Regurgitation (PR), a dilated right atrium and ventricle, severe PAH at 84 mmHg, an immensely dilated pulmonary artery with a main pulmonary artery diameter of 44 mm, and paradoxical septal motion. She was started on furosemide (20 mg) twice daily. The obstetricians decided to perform an elective Caesarean section scheduled for the following day. Her blood pressure and heart rate were 138/84 mmHg and 104 beats/min preoperatively. A multidisciplinary team of trained anaesthesiologists, obstetricians, paediatricians and nursing staff were informed to be present on a priority basis in the Operating Room (OR). The procedure was explained to the patient and her husband, and consent was obtained regarding the risks to both the mother and foetus. The plan for anaesthesia favoured a subarachnoid block over general anaesthesia, firstly to minimise the exposure of the foetus to the adverse side-effects of general anaesthetics, and secondly to minimise airway handling, as the patient already had preeclampsia and bilateral pitting oedema, indicating anticipated airway difficulty. The anaesthetic goal was to prevent hypoxia, acidosis, hypercapnia and profound hypotension. Aspiration prophylaxis was administered with ranitidine 50 mg and ondansetron 4 mg intravenously. The patient was shifted to the OR, and standard American Society of Anaesthesiologists (ASA) monitors (non invasive BP, ECG and pulse oximeter) were attached. Two wide-bore (18 G) cannulas were secured, and intravenous Ringer’s lactate was started through one cannula. Right radial arterial catheterisation was performed for continuous arterial monitoring in anticipation of haemodynamic alterations.
Baseline Arterial Blood Gas (ABG) analysis revealed pH/pO2/pCO2/HCO3/BE/Lac/Na+/K+/Ca+=7.43/104/28/22/−1.1/0.96/134/3.56/0.8. All emergency cardiac medications and defibrillators were prepared in anticipation of adverse cardiac events, and a difficult airway cart was kept on standby. Under aseptic precautions, a fractionated subarachnoid block was administered using a 23G Quincke spinal needle, with an injection of 0.5% heavy bupivacaine (1.6 mL) and an injection of fentanyl (0.2 mL) at the level of the third lumbar intervertebral space. She was also started on an infusion of adrenaline at a rate of 0.1 mcg/kg/min to prevent sudden hypotension induced by spinal anaesthesia. Supplementary oxygen was supplied via nasal prongs at 4 litres/min intraoperatively. A 1.8 kg small-for-gestational-age baby was delivered, with an Appearance, Pulse, Grimace, Activity and Respiration (APGAR) score of 7/10 at 1 minute and 9/10 at 5 minutes. After initial resuscitation, the baby was transferred to the nursery. Oxytocin (15 IU) was injected intramuscularly following the delivery of the baby. The infusion of adrenaline was gradually tapered off. The rest of the surgery was uneventful, and her haemodynamics remained within 10% of preoperative values throughout the one-hour surgery. The total urine output was 200 mL, and the total blood loss was 300 mL. The ABG at the end of the surgery revealed pH/pO2/pCO2/HCO3/BE/Lac/Na+/K+/Ca+=7.34/159/32/20/−5.2/1.29/138/4/0.8. Adequate analgesia was ensured in the postoperative period to prevent sympathetic stimulation. She was shifted to the Intensive Care Unit after 45 minutes of close monitoring in the Post-Anaesthesia Care Unit (PACU), with cardiology and cardiac surgery follow-up. The cardiologist started her on tablet (tab) tadalafil 20 mg, tab ambrisentan 5 mg, and tab spironolactone 25 mg twice daily, with proper antibiotic coverage. Cardiac surgery consultation revealed the defect to be inoperable and fatally irreversible. She was transferred to a cardiac centre for better management of her condition after she was stabilised haemodynamically, with BP 132/76 mmHg, HR 98/min, and SpO2 99% on nasal prongs at 2 litres/min oxygen.
Discussion
Cardiac diseases in pregnancy are leading causes of maternal mortality in the peripartum period, with an incidence of 0.3-3.5%. ASD is the most common acyanotic cardiac anomaly, accounting for 10% of Grown-up Congenital Heart Disease (GUCHD), with a higher prevalence among females. Patients often go unrecognised until middle age when complications such as arrhythmia and paradoxical embolism become more prominent [1]. There are three types of ASD based on anatomical location: ostium secundum (85%), ostium primum (10%) and sinus venosus (5%), with coronary sinus defects being rare. Smaller defects (<3 mm) can close spontaneously within 18 months, while medium-sized defects (3-8 mm) may take longer to close. In contrast, defects larger than 8 mm typically require surgery [2]. Large ASDs cause shunting of blood from left to right. Pregnancy and anaesthetic agents further complicate the steady state between systemic and pulmonary circulation [2].
Here, the authors reported a case of successful management of a primigravida undergoing elective Caesarean section with an enormous ASD of 34 mm, possibly the largest reported to date, further complicated by severe pulmonary hypertension and preeclampsia, under fractionated low-dose spinal anaesthesia. Written informed consent was obtained from the patient before reporting the present case.
The physiological haemodynamic changes in pregnancy include increased stroke volume, cardiac output, heart rate and oxygen consumption [3]. These changes are further accentuated by foetal growth and peak during labour and the puerperium. The left-to-right shunting of blood in ASD places a significant load on the right atrium, right ventricle, pulmonary arteries and lungs. Sympathetic hyperstimulation and increased metabolic demand during labour further exacerbate shunting [4]. All these factors pose an unanticipated challenge to the anaesthesiologist when choosing suitable anaesthesia for the patient. General anaesthesia carries the risk of abrupt and uncontrolled fluctuations in haemodynamics, with the possibility of reversing the intracardiac shunt. It also increases the chances of air embolism during vascular access, heart block, rhythm disturbances (5-10%), heart failure and infective endocarditis [5].
The authors choice was regional anaesthesia, keeping in mind that it is always preferable to general anaesthesia for both the mother and foetus [6]. From the aspect of preeclampsia, regional anaesthesia not only decreases maternal morbidity and mortality but also increases uteroplacental flow and improves neonatal outcomes [7]. One added benefit of the authors decision was the avoidance of an anticipated difficult airway. Perioperative changes in Systemic Vascular Resistance (SVR) can impact patients with ASD [1]. The authors chose to perform low-dose spinal anaesthesia, as it would lead to less hypotension. Procedure was started with an adrenaline infusion to firstly counteract abrupt hypotension caused by spinal anaesthesia; and secondly decrease the risk of acute heart failure. The authors administered the spinal anaesthesia in a fractionated dosage. The initial two-thirds of the drug was given, and the syringe was kept attached, followed by one-third of the drug after 45 seconds to prevent sudden hypotension and ensure better haemodynamic stability. This approach was motivated by findings from Badheka JP et al., which indicated that a fractionated dose in obstetric patients undergoing elective Caesarean sections resulted in better haemodynamic stability compared to a bolus dose of spinal anaesthesia [8]. Another study by Derakhshan P et al., found that a fractionated dose administered 45 seconds apart not only caused less frequent haemodynamic changes but was also associated with a longer duration and better blockade compared to the bolus method of spinal anaesthesia [9]. According to the literature, oxygen is a potent and selective vasodilator of the pulmonary vasculature with minimal systemic side-effects [10]. Comparisons of multiple studies have shown a reduction of 5-15% in mean pulmonary artery pressure with acute oxygen administration [10-14]. Therefore, the authors provided patient with supplemental oxygen at 4 litres per minute via nasal cannula throughout the surgery, which is beneficial in cases of severe PAH. The nasal cannula is the simplest oxygen delivery device, capable of delivering 1-6 litres per minute of oxygen with a variable FiO2 of 24-40% [15]. Intraoperatively, special care was taken to maintain haemodynamics as close to preoperative values as possible to prevent the worsening of shunt reversal. Perioperatively, the authors ensured adequate preload, good contractility of the heart, near-normal heart rate and SVR, and adequate analgesia to achieve favourable outcomes.
Conclusion(s)
Cardiac diseases in pregnancy further complicate the already altered physiology of obstetric patients. A good preoperative assessment, adequate intraoperative preparation and effective analgesia, during both the intraoperative and postoperative periods are essential. Additionally, fair anticipation and emergency preparedness are necessary to manage these challenging conditions. From the present case, the authors can conclude that low-dose fractionated spinal anaesthesia can be beneficial for Caesarean sections in patients with massive ASD with significant shunting and severe PAH, particularly in those with uncomplicated preeclampsia receiving prophylactic adrenaline infusion.
Author Declaration:
Financial or Other Competing Interests: None
Was informed consent obtained from the subjects involved in the study? Yes
For any images presented appropriate consent has been obtained from the subjects. Yes
Plagiarism Checking Methods: [Jain H et al.]
Plagiarism X-checker: Jun 10, 2024
Manual Googling: Jul 29, 2024
iThenticate Software: Sep 03, 2024 (9%)
[1]. Madaan V, Gupta R, Anaesthetic management of a case of large ASD with severe pulmonary hypertension—case presentationAin Shams J Anaesthesiol 2022 14(1):3210.1186/s42077-022-00232-3 [Google Scholar] [CrossRef]
[2]. Baboker P, Demissie H, Anesthetic management of patient with large atrial septal defect for caesarean delivery in resource limited SettingClinical Case Reports and Studies 2023 4(1):01-03.10.59657/2837-2565.brs.23.092 [Google Scholar] [CrossRef]
[3]. Kumar B, Soni S, Jafra A, Anesthetic management of double atrial septal defect with moderate pulmonary hypertension emergency caesarean sectionJ Anesth Clin Res 2019 10(2):100087610.4172/2155-6148.1000876 [Google Scholar] [CrossRef]
[4]. Periambudi AA, Zainal R, Lestari MI, Spinal anesthesia in patient with congestive heart failure due to congenital atrial septal defect, and pulmonary hypertension undergoing cesarean section procedure: A case reportJACR 2021 1(2):95-102.10.37275/jacr.v1i2.141 [Google Scholar] [CrossRef]
[5]. Howard-Quijano K, Smith M, Schwarzenberger JC, Perioperative care of adults with congenital heart disease for non-cardiac surgeryCurr Anesthesiol Rep 2013 3(3):144-50.10.1007/s40140-013-0023-8 [Google Scholar] [CrossRef]
[6]. Iddrisu M, Khan ZH, Anesthesia for cesarean delivery: General or regional anesthesia—A systematic reviewAin-Shams J Anaesthesiol 2021 13(1):01-07.10.1186/s42077-020-00121-7 [Google Scholar] [CrossRef]
[7]. Ankichetty SP, Chin KJ, Chan VW, Sahajanandan R, Tan H, Grewal A, Regional anesthesia in patients with pregnancy induced hypertensionJ Anaesthesiol Clin Pharmacol 2013 29(4):435-44.10.4103/0970-9185.11910824249977 [Google Scholar] [CrossRef] [PubMed]
[8]. Badheka JP, Oza VP, Vyas A, Baria D, Nehra P, Babu T, Comparison of fractionated dose versus bolus dose injection in spinal anaesthesia for patients undergoing elective caesarean section: A randomised, double-blind studyIndian J Anaesth 2017 61(1):55-60.10.4103/0019-5049.19839028216705 [Google Scholar] [CrossRef] [PubMed]
[9]. Derakhshan P, Faiz SHR, Rahimzadeh P, Salehi R, Khaef G, A comparison of the effect of fractionated and bolus dose injection on spinal anesthesia for lower limb surgery: A randomized clinical trialAnesth Pain Med 2020 10(5):e10222810.5812/aapm.102228 [Google Scholar] [CrossRef]
[10]. Green S, Stuart D, Oxygen and pulmonary arterial hypertension: Effects, mechanisms, and therapeutic benefitsEur J Prev Cardiol 2020 28(1):127-36.10.1093/eurjpc/zwaa00133623970 [Google Scholar] [CrossRef] [PubMed]
[11]. Roberts DH, Lepore JJ, Maroo A, Semigran MJ, Ginns LC, Oxygen therapy improves cardiac index and pulmonary vascular resistance in patients with pulmonary hypertensionChest 2001 120(5):1547-55.10.1378/chest.120.5.154711713133 [Google Scholar] [CrossRef] [PubMed]
[12]. Groth A, Saxer S, Bader PR, Lichtblau M, Furian M, Schneider SR, Acute hemodynamic changes by breathing hypoxic and hyperoxic gas mixtures in pulmonary arterial and chronic thromboembolic pulmonary hypertensionInt J Cardiol 2018 270:262-67.10.1016/j.ijcard.2018.05.12729891241 [Google Scholar] [CrossRef] [PubMed]
[13]. Green S, Stuart D, Effects of oxygen therapy in a young normoxaemic patient with pulmonary arterial hypertension and congenital heart diseasePulm Circ 2019 9(2):01-03.10.1177/204589401984561030942130 [Google Scholar] [CrossRef] [PubMed]
[14]. Green S, Stuart D, Oxygen therapy for pulmonary arterial hypertension: We need to rethink and investigateRespirology 2020 25(5):470-71.10.1111/resp.1379732147908 [Google Scholar] [CrossRef] [PubMed]
[15]. Hardavella G, Karampinis I, Frille A, Sreter K, Rousalova I, Oxygen devices and delivery systemsBreathe 2019 15(3):e108-16.10.1183/20734735.0204-201931777573 [Google Scholar] [CrossRef] [PubMed]