In dentistry, there has been a growing demand for aesthetic, natural-appearing restorations with better compatibility and low plaque affinity to promote periodontal health. In prosthodontics, the materials used for fixed dental prostheses have evolved over the years, and their production stages are being rapidly automated with each passing day [1].
In recent years, the demand for natural-looking restorations with enhanced biocompatibility has led to the rise of metal-free alternatives. Despite initial reservations, advancements in material science have propelled the viability of metal-free restorations, particularly for anterior teeth. However, challenges such as low fracture resistance and improper marginal adaptation have hindered their application in posterior restorations [2,3].
Material science has transformed with the advent of CAD/CAM technology in dentistry in the 1980s. These developments have greatly enhanced the manufacturing of indirect restorations with unparalleled strength and performance. One such material is Yttria-stabilised Tetragonal Zirconia Polycrystals (Y-TZP). Zirconia, a crystalline dioxide of zirconium, was dubbed ‘ceramic steel’ by Gravie in 1972, showcasing mechanical properties akin to metal along with excellent aesthetics. Due to its exceptional strength, lengthy fabrication time and tool wear, fully sintered zirconia presents significant challenges to technicians during manufacturing. To overcome this, zirconia is processed in its presintered phase, and the final sintering is done after the fabrication. The clinical applications of zirconia in dentistry include anterior and posterior Fixed Partial Dentures (FPDs) and implant abutments [4]. Zirconia serves as an excellent framework material for crowns and long-span bridges in posterior teeth, offering high toughness, compressive strength, fracture resistance, chemical stability and biocompatibility. However, it lacks tensile strength and etching properties, requiring layering for enhanced aesthetics, although it is prone to fracturing when paired with porcelain under occlusal stresses [3].
High-performance polymers like Polyaryletherketone (PAEK), Polyetheretherketone (PEEK) and Polyetherketoneketone (PEKK) have been introduced in dentistry as alternatives to ceramic restorations. PEEK, introduced in 1978, stands out within the PAEK family for its physiologically inert, water-insoluble properties, making it widely used. Its benefits include radiolucency, low plaque affinity and exceptional chemical resistance [5]. Despite its opaque, greyish appearance, PEEK requires layering with tooth-coloured materials for better aesthetics. Its biomechanical properties, including high fracture strength, rigidity and dimensional stability, make it ideal for various dental restorations like implant prostheses, bars and fixed dental prostheses [3].
Young’s modulus for PEEK in its pure form is around 3.6 GPa, which is similar to that of cortical bone, whereas for zirconia, it is 200 GPa. When reinforced with carbon, Carbon Fibre-reinforced-PEEK (CFR-PEEK), its modulus of elasticity can increase to between 19 GPa and 150 GPa. These characteristics make PEEK an ideal material. Additionally, it has a low density of 1.28-1.32 g/cm3 compared to 6.49 g/cm3 for zirconia, making PEEK useful for fabricating lightweight prostheses [6,7]. PEEK prostheses can be manufactured using vacuum-press techniques with granules or pellets, or they can be milled using CAD/CAM technology, offering flexibility in manufacturing.
The success of the restoration hinges on three main factors: marginal fit, fracture resistance, and aesthetics. Mechanical properties and fracture load are pivotal for the prognosis of restoration under occlusal forces and for the long-term success of the restoration. The tooth-restorative margin contact forms the weakest point in fixed prosthetic treatment. A poor fit could result in the cement dissolving and fluid seeping through, which could induce secondary caries, sensitivity, pulp exposure, plaque deposition and periodontal destruction [2]. PEEK is a relatively new material that is becoming popular in clinical practice and can prove to be a competent coping material like zirconia [3]; however, literature on its use as a coping material is limited.
Therefore, the present study was planned to evaluate and compare the marginal fit and fracture resistance properties of PEEK and zirconia copings. For marginal fit analysis, the null hypothesis stated that there was no significant difference between the materials (PEEK and zirconia copings) and between the sides (palatal and buccal sides). For fracture resistance, the null hypothesis stated that there is no significant difference in the mean fracture resistance between PEEK copings and zirconia copings.
Materials and Methods
The present in-vitro study was carried out in the Department of Prosthodontics, Maharishi Markandeshwar College of Dental Science and Research, Mullana, Ambala, Haryana, India, in collaboration with Acucal Services, Ambala Cantt, Haryana, and Em Cee Cee Sports Ag. Pvt. Ltd., Jalandhar, Punjab. The study took place over a span of two years, from November 2022 to March 2024. Study was conducted after obtaining clearance from Institutional Ethical Committee (IEC number: 2255).
Inclusion criteria: Maxillary first premolars, which were extracted for orthodontic purposes, with a crown size having a mesiodistal diameter of 7-8 mm and a buccolingual diameter of 9-10 mm were included in the study.
Exclusion criteria: Teeth with caries, any restorations, or any defects were excluded from the study.
Sample size: The sample size was calculated using the software OpenEpi, Version 3; and was calculated to be 20 (10 for the PEEK group and 10 for the zirconia group).
Study Procedure
The maxillary first premolar was mounted in dental plaster and then prepared for all-ceramic restorations. The prepared tooth was scanned using a 3D scanner (Medit T 310 3D Scanner), and the data was stored in Stereolithography (STL) files, which were later used to fabricate resin dies using a 3D printer (Elegoo Saturn 8K Resin 3D Printer) and a resin dye material (Phrozen Aqua 4K 3D Printing Resin). In total, 20 resin dies were created [Table/Fig-1]. These dies were divided into two groups for the fabrication of 10 PEEK copings (Group A) and 10 zirconia copings (Group B) using CAD/CAM technology. After grouping, the samples were numbered from 1 to 10 in each group [Table/Fig-2].
Resin dies fabricated from 3D printer.
PEEK and zirconia copings.

The resin dies were scanned using a 3D extraoral scanner. CAD software (exocad) [Table/Fig-3] was used to design the copings, and photographs were taken to ensure a uniform thickness of 0.5 mm and a virtual cement layer of 50 μm, which was applied 1 mm above the shoulder finish line. The zirconia copings were designed with a uniform thickness of 0.5 mm and a cement space of 50 μm starting 1 mm above the finish line. A 5-axis milling machine (Arum 5X-300 D milling machine) [Table/Fig-4] was used to fabricate both PEEK and zirconia copings.
Designing the coping using the CAD software.

Computer-assisted milling machine.

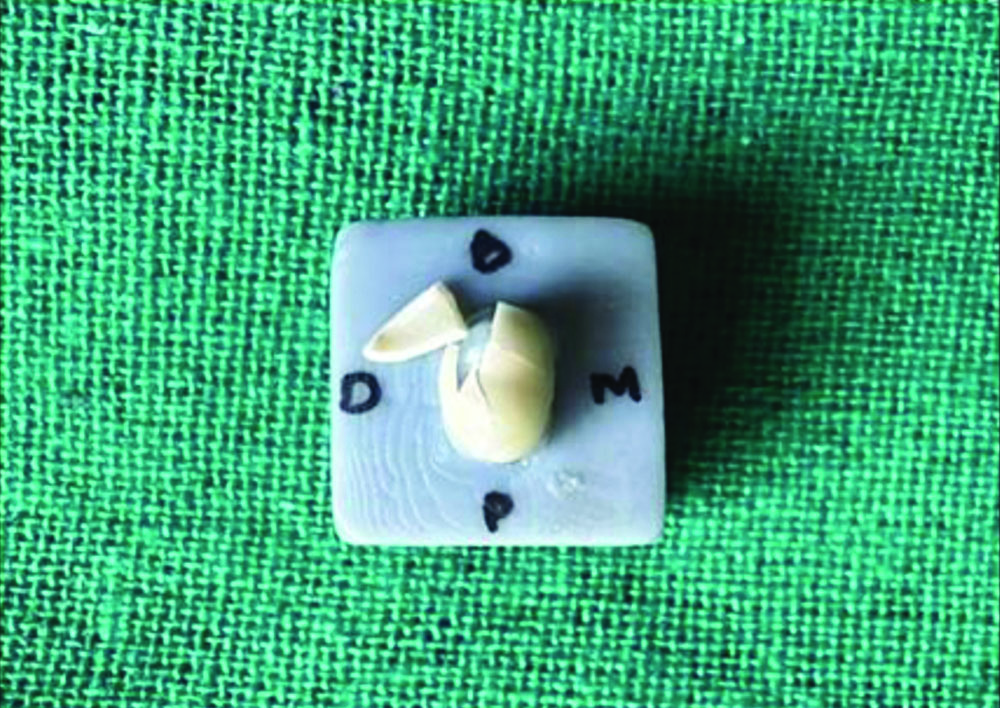
The PEEK and zirconia copings were collected, and reference points were marked on the margins of two aspects: buccal (b) and palatal (p) using a bur attached to a micromotor to ensure uniform depth and size of the marked points [Table/Fig-5]. At each marked reference point, three readings were recorded: for the palatal side, p1, p2 and p3; and for the buccal side, b1, b2 and b3. The fit of the PEEK and zirconia copings was analysed on each resin die, and they were luted onto the prepared surface of the resin die using a self-adhesive translucent resin cement with finger pressure for atleast 10 minutes. The excess cement was removed from the margins.
Reference points for marginal fit.
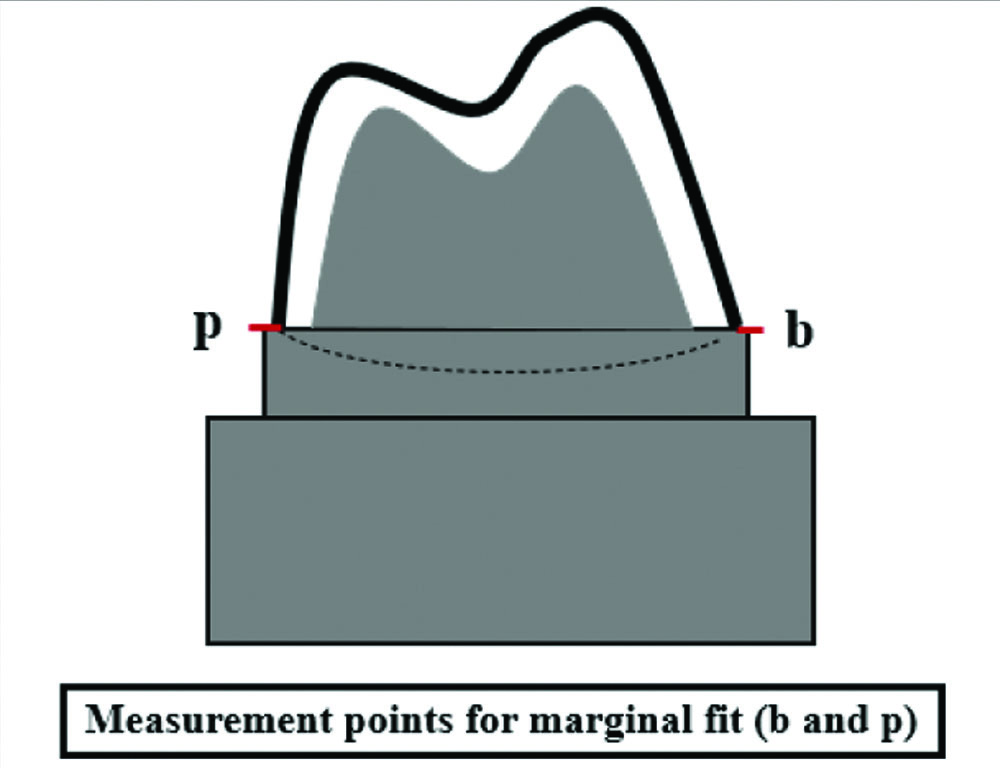
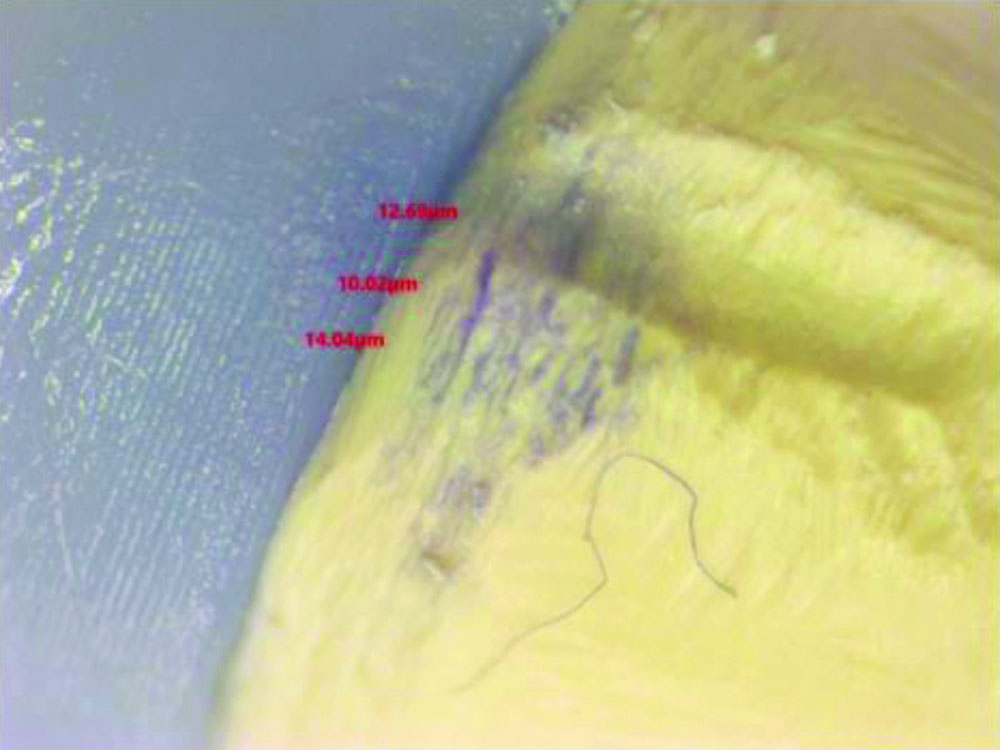
The PEEK and zirconia copings were evaluated under a stereomicroscope at 60x magnification at the marked reference points to check the marginal fit [Table/Fig-6]. The restoration-tooth margin was observed to assess the marginal gap, which was measured as the separation between the prepared tooth’s external marginal line and the extended point on the coping margin [Table/Fig-7].
Stereomicroscope*.
(*Stereo Zoom Microscope Make: ACUCAL- PEEK coping being evaluated under a stereomicroscope at 60x magnification)

Marginal gap at the marked reference point for PEEK coping.
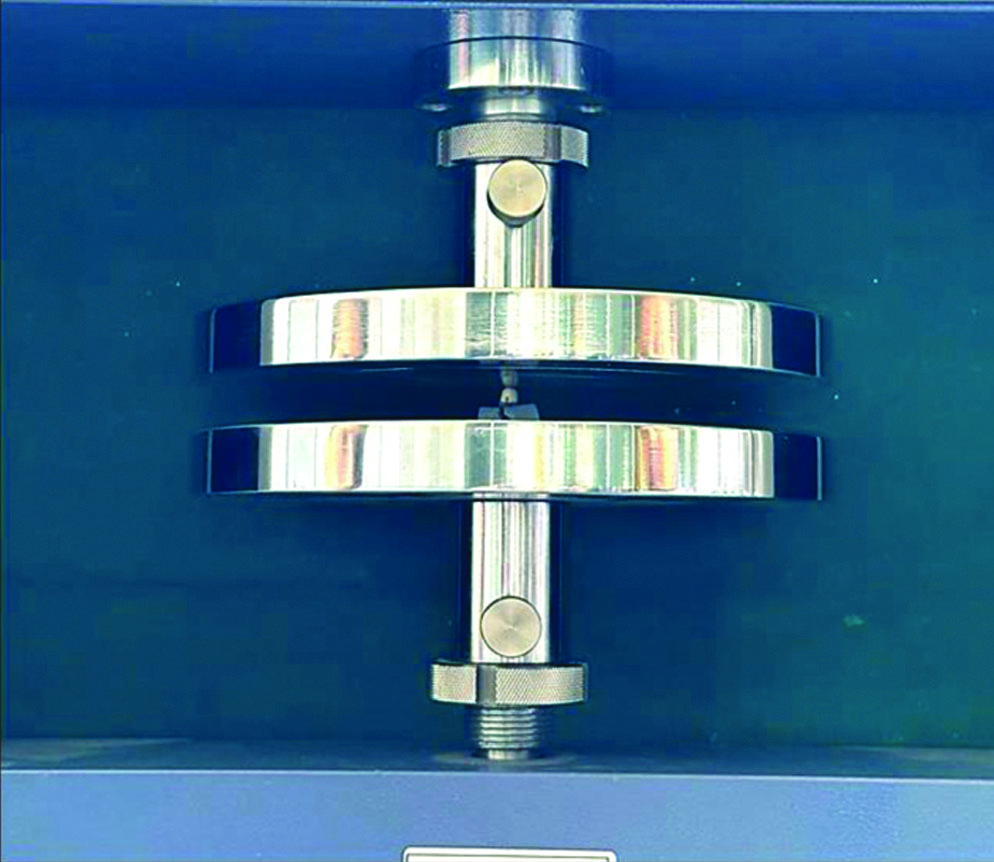
All 20 samples were subjected to thermal cycling to simulate the oral environmental conditions. Each sample underwent 1000 thermal cycles at 5°C and 55°C in a water bath, with a dwell time of 15 seconds and a transfer time between the baths of 15 seconds, similar to the studies by Sarfaraz H et al., [8]. After thermal cycling, all the samples were assessed for fracture resistance using a Universal Testing Machine (UTM) (Presto Computerised Tensile Testing Machine and UTM) [Table/Fig-8]. Therefore, the maximum vertical dislodging force was recorded at a crosshead speed of 1 mm/min. The test samples were placed in the lower compartment of the machine, with the central fossa directly aligned with the centre of the upper compartment to ensure a uniform distribution of stresses. The failure load or fracture resistance value was determined by recording the value that corresponded to the specimen’s first break. The force was recorded in Newtons, and it was noted that the load decreased by 30% from the maximum load [Table/Fig-9].
Universal testing machine.
Statistical Analysis
A two-way ANOVA was used to assess whether there are significant differences in marginal fit based on material and side between PEEK and zirconia copings. To compare the fracture resistance of PEEK and zirconia copings, an independent t-test was applied to assess whether there is a statistically significant difference in the mean fracture resistance between the two materials. The p-value <0.05 was considered statistically significant.
Results
The mean±Standard Deviation (SD) for marginal fit was calculated aspect-wise for both the PEEK and zirconia groups based on the three readings obtained for all samples at the palatal and buccal aspects. These mean readings were then used for comparative analysis [Table/Fig-10]. For both the palatal and buccal aspects, the test results showed higher mean values for the PEEK copings (palatal side: 23.941±7.73 μm and buccal side: 22.338±7.89 μm) compared to the zirconia copings (palatal side: 18.469±6.55 μm and buccal side: 17.116±6.34 μm). This implies less discrepancy at the margins for the zirconia group, indicating that the zirconia copings have better marginal adaptation than the PEEK copings.
Marginal fit value comparison of PEEK and zirconia copings.
| Tooth aspect | Marginal fit |
|---|
| PEEK copings (n=10) | Zirconia copings (n=10) |
|---|
| Palatal side* (n=30) | 23.941±7.73 | 18.469±6.55 |
| Buccal side* (n=30) | 22.338±7.89 | 17.116±6.34 |
| p-value | 0.0000753* |
*At each marked reference point, three readings were recorded. The markings on the palatal side- p1, p2 and p3; and on the buccal side- b1, b2 and b3 were recorded; *The p-value <0.05 was considered statistically significant
The results of the two-way ANOVA indicate a significant difference in marginal fit between the two materials used in the study (PEEK and zirconia). The p-value associated with the ‘material’ factor is highly significant (p-value=7.53e-05), suggesting that the choice of material has a substantial impact on the marginal fit value. However, the factor ‘side’ (palatal or buccal) does not show a significant effect on marginal fit, as indicated by a non significant p-value (p-value=0.259). This implies that, on average, across both materials, the location of the fit measurement (palatal or buccal) does not significantly influence marginal fit. Thus, the difference in marginal fit is primarily attributed to the choice of material, with no significant influence from the side of measurement.
For the analysis of fracture resistance, higher mean values are shown by the PEEK group compared to the zirconia group. This indicates that the PEEK copings exhibit greater fracture resistance than the zirconia copings [Table/Fig-11]. A two-sample t-test was conducted to compare the means of fracture resistance between the PEEK and zirconia copings. The analysis yielded a p-value of 0.04884, which is less than the common significance level of 0.05.
Fracture resistance comparison of PEEK and zirconia copings.
| Variables | Fracture resistance |
|---|
| PEEK copings (n=10) | Zirconia copings (n=10) |
|---|
| Mean | 523.11 | 395.4 |
| Standard deviation | 117.2780594 | 150.9328033 |
| p-value | 0.04884* |
Discussion
In the era of digitalisation in prosthodontics, it has become possible to manufacture newer materials with good strength and performance. Using CAD/CAM technology, it has become easier to produce precise restorations that demonstrate both longevity and durability [9].
According to Rodriguez V et al., marginal adaptation, fracture resistance and aesthetics are the three key elements that influence the success of restorations, even with advancements in CAD/CAM technology [10]. McLean JW and Von Fraunhofer JA (1971) stated that for crown prostheses, the clinically acceptable marginal gap is approximately 120 μm, ensuring the longevity of the prostheses [11]. However, El-Dessouky RA et al., reported that marginal discrepancies ranging between 17 μm and 161 μm have been found for all-ceramic restorations fabricated using different techniques [12]. Therefore, the strength of the finished restoration and the marginal fit are significantly impacted by the various materials and manufacturing processes used in crown systems.
The present study was conducted to evaluate and compare the marginal fit and fracture resistance of PEEK and zirconia copings fabricated using CAD/CAM technology. Additionally, standardised resin master dies were used. This material was preferred because of its high tensile modulus, low brittleness, great hardness and stiffness, and good clarity, which provided visibility to evaluate the marginal gap using digital microscopes.
Previous authors have studied the marginal gap at various reference points. Groten M et al., (2000) suggested using 50 reference points for measuring the marginal fit, while Gassino G et al., (2004) suggested using 18 reference points [13,14]. However, different studies have reported the number of measurements to range between 4, 8 and 12, which is closer to the number of reference points marked in the present study.
In the present study, the mean marginal gap for PEEK copings was significantly higher than that for zirconia copings. For the PEEK copings, a marginal discrepancy of 23.941±7.73 μm was reported on the palatal side and 22.338±7.89 μm on the buccal side. These values were consistent with the observations by Attia MA and Shokry TE, and Abdullah AO et al., for PEEK CAD/CAM copings [3,15]. The mean marginal gap observed for zirconia copings in this study was 18.469±6.55 μm for the palatal side and 17.116±6.34 μm for the buccal side, which were similar to the results observed by Emam M and Metwally MF (2023), who also reported a similar range of marginal discrepancy for partially sintered zirconia [16].
The results of the marginal fit were congruent with the study conducted by Emad M et al., which highlighted a higher marginal discrepancy in PEEK crowns compared to zirconia crowns. The present study was also conducted using a stereomicroscope [17]. Additionally, favourable results were reported by Makky MR et al., who stated a significantly lower marginal gap for the zirconia group than for the PEEK CAD and PEEK pressed groups [18]. Baran MC et al., evaluated the adaptation of three-unit Fixed Dental Prosthesis (FDPs) processed using zirconia, PEEK, PEKK and fibre-reinforced polymer composite, using silicon replica technique under a stereomicroscope at 40x [19]. Their results concluded that the best adaptation was shown by the zirconia FDP.
In the present study, PEEK copings demonstrated a higher marginal discrepancy compared to zirconia copings. This could be due to the semicrystalline nature of PEEK, which has a structure made of filler particles embedded in the resin matrix, resulting in a higher marginal gap during manufacturing. In contrast, zirconia is polycrystalline. The present study did not align with the findings of Bae SY et al., who compared the marginal and internal fit of PEKK and zirconia copings, stating that PEKK copings showed a better fit than zirconia copings [20]. Similarly, Park JY et al., used the replica technique to compare the marginal fit of PEEK, zirconia and lithium disilicate crowns, concluding that the marginal discrepancy for all crowns was clinically acceptable [21]. Amalorpavam V et al., also concluded that zirconia copings exhibited less marginal and internal adaptation compared to PEEK copings, with the difference being statistically significant, as observed under a scanning electron microscope [22].
After the analysis of the marginal fit, all the samples underwent artificial ageing. According to Güngör MB and Nemli SK, all samples must undergo dynamic loading and thermal cycling to simulate the changes observed in the oral environment [23]. In the present study, all the copings were subjected to thermal cycling for 1000 cycles at temperatures of 5°C and 55°C in a water bath, with a dwell time of 15 seconds and a transfer time of 15 seconds. The copings were then assessed for fracture resistance in a universal testing machine, where the maximum dislodging force was recorded at a cross-head speed of 1 mm/minute.
Beuer F et al., stated that for fixed prostheses, fracture strength is determined by several parameters, including cementation, loading circumstances, and the elastic modulus of the supporting die [24]. Scherrer SS and De Rijk WG stated that when the Young’s modulus of the supporting die is greater, it may result in larger fracture strength [25]. Different authors have tested fracture resistance using stainless-steel dies, epoxy resin, or acrylic dies with varying mechanical properties. However, the dies used in this study were digitally obtained and fabricated using 3D printing technology, with a tensile modulus of 1037 MPa. Cementation and loading factors were consistent for all samples used in the study.
The maximum bite force for the maxillary premolar area ranges between 222 and 445 N, with a mean force of 322.5 N. In this study, an average load-bearing capacity of 300 N was used to represent adequate fracture resistance against normal occlusal forces. The results indicated that the fracture resistance of PEEK copings was significantly higher than that of zirconia copings (p-value=0.048, p-value <0.005). The mean values reported were 523.11±117.27 N for PEEK copings, with the highest fracture load recorded at 725.1 N. In contrast, the mean fracture load recorded for zirconia copings was 395.4±150.93 N, with the highest load observed at 570 N.
The results of the current study were congruent with those of Hossam M et al., who compared the load-bearing capacity of PEEK {Bio-high Performance Polymer (BioHPP)} and zirconia three-unit framework prostheses using a universal testing machine [26]. The PEEK group showed higher fracture resistance than the zirconia group. In that study, epoxy dies were used, and no artificial ageing was performed.
Rodriguez V et al., studied the fracture resistance of FPD frameworks processed using metal, zirconia and PEEK CAD/CAM milled materials. Their results indicated the highest fracture resistance for metal prostheses, followed by PEEK and zirconia prostheses [10]. Emam M and Metwally MF reported no significant difference in the fracture resistance of molar crowns manufactured using PEEK (CAD), pressed PEEK and zirconia groups [16]. A similar study by El Sokkary A et al., also observed no significant difference in the fracture resistance of zirconia and PEEK veneered groups [27].
In contrast, a study by Tartuk BK et al., examined the load-bearing capacity of CAD/CAM crowns made from zirconia, PEEK and hybrid ceramic crowns [28]. A statistically insignificant difference was observed between the PEEK (2214±236 N) and the ceramic group (2325±264 N); however, the zirconia group exhibited the highest values (3292±192 N). Additionally, a zirconia die was used in that study. Stawarczyk B et al., examined the load-bearing capacity of PEEK three-unit FDPs manufactured using CAD/CAM and pressed granules, stating that PEEK CAD/CAM showed a higher fracture resistance than the pressed group [29]. A comparative evaluation of similar studies has been presented in [Table/Fig-12,13] [1,10,16,18,20,22,29].
Comparison with similar studies for marginal fit [16,18,20,22].
| S. No. | Author name and year | Place of study | Number of samples | Factors studied | Conclusions |
|---|
| 1 | Emam M and Metwally MF (2023) [16] | Cairo, Egypt | N=18(six specimens in three groups-Zirconia, PEEK milled and PEEK pressed crowns) | Marginal fit | Zirconia framework crowns have a smaller vertical marginal gap than milled and pressed PEEK crowns. |
| 2 | Makky MR et al., (2020) [18] | Cairo, Egypt | N=21 Copings were divided according to the type of material and method of manufacturing into three main groups: seven specimens each, zirconia (Zr), PEEK CAD (PC) and PEEK press (Pp) groups | Marginal and internal fit | Marginal and internal fit for the three groups were within the acceptance range, while zirconia copings showed superior marginal fit than PEEK groups. |
| 3 | Amalorpavam V et al., (2021) [22] | Kavalkinaru, Tirunelveli, India | N=30(PEEK copings-15, Zirconia copings-15) | Marginal fit and internal adaptation | The study concluded that the PEEK copings exhibited enhanced marginal fit and internal adaptation compared to Zirconia copings. |
| 4 | Bae SY et al., (2016) [20] | Seoul, South Korea | N=20(10 PEEK copings and 10 Zirconia copings) | Marginal and internal fit | The study concluded that PEEK copings presented a much better marginal and internal fit than the zirconia copings. |
| 5 | Present study | Mullana, Ambala (India) | N=20(PEEK copings-10, Zirconia copings-10) | Marginal fit | For marginal fit, Zirconia copings showed better marginal fit than PEEK copings. |
Comparison with similar studies for fracture resistance [1,10,16,29].
| S. No. | Author name and year | Place of study | Number of samples | Factors studied | Conclusion |
|---|
| 1 | Emam M and Metwally MF (2023) [16] | Cairo, Egypt | N=18(six specimens in three groups- Zirconia, PEEK milled and PEEK pressed crowns) | Fracture resistance | Crowns fabricated from zirconia, PEEK CAD, or PEEK Press frameworks and veneered with composite resin have comparable fracture resistance. |
| 2 | Rodriguez V et al., (2021) [10] | Madrid, Spain | N=30 (three-unit posterior FPD randomly divided into 3 groups- milled metal, Zirconia and PEEK) | Fracture load and fracture pattern | The study concluded that for assessing the fracture load the milled metal frameworks showed superior values followed by PEEK and zirconia, also PEEK might be considered a promising alternative for posterior FDP. |
| 3 | Gupta AK et al., (2021) [1] | New Delhi, India | N=40PEEK copings were divided into four groups, based on different surface treatments and veneering with composite and lithium disilicate on PEEK copings each group having 10 copings | Load bearing capacity, Failure mode | The highest load-bearing capacity was noted for chemically etched Lithium Disilicate with 98% sulfuric acid veneered on PEEK copings, followed by groups 3, 1, and 2. |
| 4 | Stawarczyk B et al., (2015) [29] | Zurich, Switzerland | N=45PEEK frameworks are divided into three groups as per the fabrication technique- using CAD/CAM technology, pressed PEEK pellets, and granules | Fracture resistance | The maximum load bearing was seen in the PEEK frameworks fabricated using CAD/CAM technology, followed by frameworks fabricated by pressed PEEK pellets and granules; also, the frameworks manufactured using CAD/CAM and pressed pellets fractured at the pontic region. |
| 5 | Present study | Mullana, Ambala (India) | N=20(PEEK copings-10, Zirconia copings-10) | Fracture resistance | PEEK copings demonstrated better load bearing capacity than Zirconia copings. |
In the present study, PEEK copings exhibited significantly higher fracture resistance than zirconia copings. Therefore, it can be presumed that PEEK material exhibits better mechanical properties than zirconia. This may be due to the semicrystalline nature of PEEK, which possesses significant ductility, allowing it to withstand plastic deformation under load application. Consequently, the null hypothesis was rejected, indicating that there is sufficient evidence to conclude a significant difference in the means of fracture resistance between PEEK and zirconia copings.
Limitation(s)
This is an in-vitro study; therefore, patient-based studies are needed to evaluate mechanical properties and patient satisfaction. Resin dies were used in the present study. A natural tooth could have been used as a supporting die to better match the modulus of elasticity of a natural tooth or bone. Cementation was performed using finger pressure, and no mechanical loading was performed during the cementation process. The marginal fit was evaluated using a stereomicroscope, but the replica method, which is also commonly used to evaluate marginal adaptation, was not employed.
Conclusion(s)
Within the limitations of the present study, it can be concluded that the marginal fit of both PEEK and zirconia copings was within the clinically acceptable range, with marginal gaps observed between 23 μm and 110.1 μm. Zirconia copings demonstrated a significantly superior marginal fit compared to PEEK copings. The fracture strength is determined by several parameters, including cementation, loading conditions, and the elastic modulus of the supporting die. PEEK copings demonstrated a higher fracture resistance than zirconia copings due to the polycrystalline nature of PEEK. The results obtained in the current study are promising under laboratory conditions; however, it is necessary to investigate the properties of PEEK and zirconia copings in clinical or oral conditions. PEEK is emerging as a promising material due to its exceptional properties, and its use in both removable and fixed prostheses can be highly recommended. More studies should be encouraged to compare the load-bearing capacity, as well as, the fit of PEEK and zirconia.
*At each marked reference point, three readings were recorded. The markings on the palatal side- p1, p2 and p3; and on the buccal side- b1, b2 and b3 were recorded; *The p-value <0.05 was considered statistically significant