Homosexuality can be described as the behaviour of a person whose sexual desire is predominantly directed towards members of the same sex or who primarily engages in sexual activity with persons of the same sex [1]. MSM fall under this broader category of homosexuality. The changing societal attitudes towards sexuality and increasing acceptance have led to a noticeable rise in the number of MSM who come out and express their sexual orientation [2]. Social media and dating apps play a significant role in facilitating discreet connections among MSM [3].
MSM populations are at a higher risk of transmitting STIs and HIV infections compared to heterosexual individuals, as they often engage in high-risk sexual practices [4-6]. It is crucial to study the prevalence of STIs in this high-risk group. Limited data are currently available regarding STI prevalence among MSM in India, as noted in studies by Setia MS et al., Aggarwal P et al., and Pravitha BP et al., [5,7,8]. Understanding the prevalence of STIs in this high-risk group is essential for rapid diagnosis and effective control of infections, thereby reducing transmission [7].
The purpose of this study was to analyse the prevalence of STIs among the MSM group, which may help in understanding the factors contributing to the rise of STIs and in developing effective control measures to prevent further transmission. Ultimately, this can lead to a decrease in the overall prevalence of STIs in the community.
Materials and Methods
This was a record-based cross-sectional study conducted on men who either walked in directly or were brought in by voluntary organisations and identified themselves as homosexuals at the Venereology OPD of a tertiary care centre in Chennai, Tamil Nadu, India. This study was conducted in January 2024, and the records from January 2023 to December 2023 were reviewed, covering a 12-month period. Ethical approval was obtained from the institutional ethics committee (ECR/131/Inst/TN/2013/RR-22).
Inclusion criteria: Men above 18 years old who have sex with men and attend the Venereology OPD, whether as direct walk-ins or brought in by voluntary organisations for screening or with genital lesions, were included in the study.
Exclusion criteria: Men under 18-year-old and heterosexuals were excluded from the study.
Sample size: Sample size was calculated based on a similar study by Aggarwal P et al., India [7].
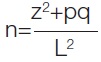
Z=1.96 (statistical significant constant for 95% CI)
P=7%, q=100-p=93, L=absolute error=5%
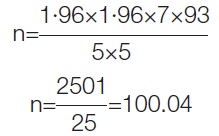
Therefore, by using the above formula and 10% non-response rate, the calculated sample size was 110.
Study Procedure
The male patients who sought care at the skin and venereal diseases OPD and reported being involved in sexual relationships with other males were retrospectively enrolled in this study. The following data were collected: demographic information regarding sexual orientation, age, marital status, educational status, present occupation, and details of their contacts. Subsequently, detailed information regarding sexual practices was obtained. This was followed by documenting the clinical history and examination findings.
All patients were screened for syphilis, HIV, and Hepatitis B. Screening for syphilis was conducted using the Rapid Plasma Reagin (RPR) test, and those who tested reactive for RPR were confirmed with the Treponema pallidum Hemagglutination Assay (TPHA) using a card test. Additional laboratory investigations were performed in accordance with the patients’ symptoms. For patients presenting with genital ulcers and discharge, smears were taken for dark field microscopy, Tzanck smear, Gram stain, and Giemsa stain. All patients were referred to the Integrated Counselling and Testing Centre (ICTC) for voluntary counselling and testing for HIV.
Statistical Analysis
The data were presented as frequencies and percentages. All analyses were conducted using SPSS software 21.0.
Results
In this study, over one year, a total of 110 patients who self-reported to the venereology OPD and identified themselves as MSM were enrolled. The prevalence of STIs in this study was found to be 42 (38.18%). Analysing the socio-demographic data, as depicted in [Table/Fig-1], the most common age group ranged from 18 to 29 years. Out of the 110 patients, 34 (30.91%) were uneducated, while the remaining were educated, which included 32 (29.09%) graduates and 4 (3.64%) postgraduates. Additionally, 23 (20.91%) MSMs were Commercial Sex Workers (CSWs), and 21 (19.09%) MSM patients were married, thereby posing an increased risk of transmission of infection to their female partners.
Socio-demographic data of MSM patients.
| Socio-demographic data | n (%) |
|---|
| Age group (years) |
| 18-29 | 61 (55.45) |
| 30-39 | 32 (29.09) |
| 40-49 | 16 (14.55) |
| >50 | 1 (0.91) |
| Education |
| Uneducated | 34 (30.91) |
| Till primary school | 31 (28.18) |
| Till higher secondary | 9 (8.18) |
| Graduate | 32 (29.09) |
| Postgraduate | 4 (3.64) |
| Marital status |
| Married | 21 (19.09) |
| Unmarried | 89 (80.91) |
| Occupation |
| Student | 6 (5.45) |
| Daily wages | 25 (22.73) |
| Self employed | 17 (15.45) |
| Professional | 30 (27.27) |
| Unemployed | 9 (8.18) |
| CSW | 23 (20.91) |
Among the 110 patients, 74 (67.27%) were brought in by voluntary organisations for screening, while the other 36 (32.73%) patients were direct walk-ins. The most common genital complaint was a genital ulcer, seen in 13 (11.82%) patients, followed by a maculopapular rash on the palms and soles in 7 (6.36%) and urethral discharge in 6 (5.45%) [Table/Fig-2]. Four (3.64%) patients who were asymptomatic at the time of presentation were found to have a sexually transmitted disease upon further laboratory investigation.
Symptoms for presentation to venereology OPD.
| Symptoms | n (%) |
|---|
| Genital ulcer | 13 (11.82) |
| Urethral discharge | 6 (5.45) |
| Growth in genitalia | 4 (3.64) |
| Maculopapular rash | 7 (6.36) |
| Itchy papules over genitalia | 3 (2.73) |
| Asymptomatic (screening) | 77 (70.00) |
[Table/Fig-3] illustrates the sexual practices among MSM patients. Sixty-seven (60.91%) men identified as strictly homosexual, while 43 (39.09%) identified as bisexual, although they predominantly preferred male partners. Fifty-seven (51.82%) men were ano-insertive in practice, and 58 (52.72%) reported having unprotected intercourse. Eighty-six (78.18%) men had contact with unknown partners.
Sexual practices in MSM patients.
| n (%) |
|---|
| Sexual orientation |
| Strictly homosexual | 67 (60.91) |
| Bisexual | 43 (39.09) |
| Details of contact |
| Known partners | 24 (21.82) |
| Unknown partners | 86 (78.18) |
| Sexual practice |
| Insertive | 57 (51.82) |
| Receptive | 40 (36.36) |
| Both | 13 (11.82) |
| Usage of condoms |
| Protected | 17 (15.45) |
| Unprotected | 58 (52.72) |
| Irregular use | 35 (31.82) |
| Presenting to STD OPD |
| Direct walk-in | 36 (32.73) |
| Through voluntary organisation | 74 (67.27) |
[Table/Fig-4] depicts the most common STDs in the MSM group. The most prevalent STD was found to be syphilis, seen in 15 (13.63%) patients, followed by HIV in 10 (9.09%) patients (among whom six had only HIV and four had a co-infection of HIV and syphilis). The next most common infections were genital herpes in 7 (6.36%), gonorrhea in 6 (5.45%), genital warts in 3 (2.73%), hepatitis B in 3 (2.73%), and genital scabies in 2 (1.81%). All others who came for screening were found to be free of STDs.
| S. No. | Disease | n (%) |
|---|
| 1. | Syphilis | 15 (13.63) |
| Primary | 5 (4.54) |
| Secondary | 4 (3.63) |
| Latent | 6 (5.45) |
| 2. | HIV | 6 (9.09) |
| Newly diagnosed | 3 (2.72) |
| Already on ART | 7 (6.36) |
| HIV with secondary syphilis | 3 (2.72) |
| HIV with latent syphilis | 1 (0.90) |
| 3. | Genital Herpes | 7 (6.36) |
| 4. | Gonorrhea | 6 (5.45) |
| 5. | Genital wart | 3 (2.73) |
| 6. | Hepatitis B | 3 (2.73) |
| 7. | Genital scabies | 2 (1.81) |
Discussion
In this study, the prevalence of STIs among MSM was found to be 38.18%. A recent study on the MSM population in Kerala by Pravitha BP et al., (2015-2020) also noted a prevalence of STIs among MSM at 46.30% [8]. Studying prevalence is crucial for public health efforts aimed at preventing the transmission of STIs and HIV.
High rates of partner turnover, high-risk sexual practices, and inconsistent condom use contribute to the increased transmission of STIs and HIV among these men. Additional factors, such as stigma associated with this population, discrimination, and barriers to accessing healthcare, further increase the risk [7]. MSM are at greater health risk than heterosexual men not only because of promiscuity but also due to the nature of sexual practices among men. Anal intercourse is relatively common among MSM, and the rectum differs significantly from the vagina. The vagina has stratified squamous epithelium with secretions that help with lubrication during sexual intercourse, allowing it to endure friction without damage and resist the immunological actions caused by semen and sperm [9]. In contrast, the rectum and anal canal consist of delicate muscles that cannot withstand the friction associated with penile penetration, leading to trauma, damage to the anal sphincter, anal tears, and fecal incontinence [10]. All of these factors expose both participants to blood and organisms in feces, resulting in infection, inflammation, and enhanced susceptibility to STIs. The fragility of the anus and rectum, along with the immunosuppressive effect of ejaculate, makes anogenital intercourse a particularly efficient means of HIV transmission [11].
In this study, the most common age group of MSM was 18 to 29 years, which was comparable to the findings of Aggarwal P et al., where the common age group ranged from 20 to 29 years [7], and Setia MS et al., where the common age group ranged from 18.5 to 28.7 years [5]. Similarly, in Pravitha BP et al., study a majority of patients were in the age group of 20 to 30 years (47.3%) [8].
In this study, 29.09% of MSM were graduates, and 3.64% were post-graduates. In Aggarwal P et al., 17.31% and 3.85% were graduates and postgraduates, respectively [7]. In this study, 15.45% were self-employed, and 27.27% were professionals. Similar findings were noted in Pravitha BP et al., study, where most patients (82.4%) among MSM were semiprofessional workers [8]. Unlike the studies conducted by Setia MS et al., Aggarwal P et al., and Pravitha BP et al., this study noted that 20.90% of MSM were CSWs [5,7,8].
In this study, 19.09% of MSM patients were married. This findingwas similar to that of Aggarwal P et al., where 34.62% were married [7], and Setia MS et al., which noted that 22% of MSM were married [5]. Pravitha BP et al., study found that 41.9% of MSM were married [8]. These MSM, who are married to women, often feel obligated to have intercourse with their wives to fulfil societal expectations of having children, thereby increasing the risk of STI transmission to females. In this study, strict MSM accounted for more (60.91%) than bisexual MSM, which was contrary to the findings of Aggarwal P et al., where bisexual individuals comprised a greater percentage (63.46%) than strict homosexuals [7]. These bisexual individuals serve as a bridge population for STI transmission [3]. Therefore, it is crucial to trace, treat, and follow-up with married and bisexual MSM due to their significant role in the spread of STIs.
Additionally, 67.27% of MSM were brought in by voluntary organisations for screening, while 3.63% of MSM who were initially asymptomatic later received an STI diagnosis. This underscores the importance of screening. Voluntary organisations also play a vital role in tracing MSM individuals, creating awareness among them regarding STI risks, motivating them for regular screenings, and counseling them on the proper use of condoms. Through regular screening, STIs can be diagnosed at an early stage, allowing for appropriate treatment to be initiated and thereby preventing complications.
In previous studies by Setia MS et al., and Brahmam GN et al., genital herpes was found to be the most common STI among MSM [5,12]. In the study, conducted by Aggarwal P et al., genital warts were the most common STI, occurring in 23.08% of cases, followed by HIV in 23.08% and syphilis in 21.15% [7]. Viral STIs were found to be more common in these studies. In contrast, the study by Pravitha BP et al., found that syphilis was the most common STI, present in 64.9% of cases, followed by genital warts in 36.5% and HIV in 14.9% [8]. Similarly, in this study, syphilis was the most common STI, found in 13.63% of MSM, followed by HIV in 9.09%. This changing trend from viral STIs to bacterial STIs has been observed after the year 2015 and continues to the present [8,13,14].
In this study, HIV co-infection with syphilis was found in 3.63% of patients. Similar findings were noted in other Indian studies, such as the study by Pravitha BP et al., [8], where HIV co-infection with syphilis was reported in 8.1% of patients and in the study by Aggarwal P et al., where the HIV-syphilis co-infection was reported in 5.77% of patients [7]. This HIV co-infection with syphilis could enhance HIV replication by increasing the activation of the immune system and causing cytokine alterations. This co-infection negatively impacts immune recovery and the effectiveness of antiretroviral therapy [15,16]. A comparison of data with similar studies has been presented in [Table/Fig-5] [4,5,7,8,17-22].
Comparison of data with similar studies on Sexually Transmitted Infections (STI) in MSM [4,5,7,8,17-22].
| S. No. | Name and year of study | Place of study | No. of subjects | Prevalence of STI (in %) | Most common STI |
|---|
| 1. | Pravitha BP et al., [8] (2015-2020) | Kerala | 74 | 46.30 | Syphilis |
| 2. | Aggarwal P et al., [7] (2013-2014) | New Delhi | 52 | 7.05 | Genital wart |
| 3. | Setia MS et al., [5] (2006) | Mumbai | 150 | 58.26 | Genital Herpes |
| 4. | Garg T et al., [4] (2004-2010) | Delhi | 75 | 10.15 | Syphilis |
| 5. | Go VF et al., [17] (2004) | Chennai | 46 | 5.90 | HIV |
| 6. | Mwaniki SW [18] (2021) | Kenya | 248 | 31.99 | Chlamydia |
| 7. | Ye ZH et al., [19] (2020) | China | 177 | 23.70 | Human Papilloma virus |
| 8. | Hart TA et al., [20] (2017-2019) | Canada | 2449 | 56.80 | HIV |
| Montreal | 1179 | 45.10 | Syphilis |
| Toronto | 517 | 57.59 | HIV |
| Vancouver | 753 | 49.09 | HIV |
| 9. | Hakim AJ et al., [21] (2016-2017) | Papua New Guinea Port Moresby | 400 | 27.00 | Chlamydia |
| Lae | 352 | 32.30 | Chlamydia |
| Mt Hagen | 111 | 27.60 | Chlamydia |
| 10. | Fournet N [22] (2006-2012) | Netherland | 2183 | 20.60 | Chlamydia |
| 11. | Present study Jan-Dec 2023 | Chennai | 110 | 38.18 | Syphilis |
In this study, it was noted that a significant number of individuals (78.18%) had contact with unknown male partners, making contact tracing very difficult and resulting in the spread of STIs to other MSM. To address this issue, social media platforms can be utilised to create awareness among MSM [23].
Some suggested strategies to decrease the prevalence of STIs in this high-risk group include increasing awareness about the signs and symptoms of STIs before entering dating apps. This knowledge helps individuals recognise early symptoms and seek treatment promptly, thereby reducing the likelihood of transmission to partners. While using dating apps, it is essential to emphasise the importance of using protection (condoms) during sexual activity. Lastly, better coordination between physicians and voluntary organisations for field-level tracing of MSM groups and their contacts will ensure that MSM individuals undergo regular screening, early diagnosis, and treatment, ultimately decreasing the prevalence of STIs.
Limitation(s)
As this is a record-based study, retrieving detailed histories was challenging. More information regarding the contacts could not be obtained. Additionally, no comparison was made between STIs among MSM and STIs among heterosexual men.
Conclusion(s)
The MSM is a high-risk group due to the high prevalence of STIs among them. In this study, the prevalence of STIs was found to be 38.18%, with syphilis being the most common STI, affecting 13.63% of the subjects. As the prevalence of syphilis and HIV among this vulnerable group continues to rise, it is crucial to create awareness about STI risks and encourage regular screening to facilitate early diagnosis and prompt treatment. Since a significant portion of the MSM population is young and educated, combining traditional outreach and educational approaches with digital interventions will be a powerful strategy for maximising healthcare initiatives within the MSM community.