Globally, glyphosate is the most widely used non selective broad-spectrum herbicide. The uncoupling of oxidative phosphorylation and polyoxymethylene amine-mediated cardiotoxicity are thought to contribute to glyphosate toxicity. Hereby, the authors presents a case report of 54-year-old male with an alleged history of consuming glyphosate, who experienced complications 48-72 hours after ingestion. These complications included acute kidney injury, corrosive injury to the oesophageal mucosa, cardiotoxicity, and Acute Respiratory Distress Syndrome (ARDS). These are rare but severe manifestations of oral glyphosate-Polyoxyethyleneamine (POEA) poisoning. The patient survived due to aggressive supportive therapy, which included renal replacement therapy, non invasive ventilation, and heart failure management. Since, there is no antidote for glyphosate poisoning, exposure to glyphosate can be fatal, necessitating vigorous supportive therapy. Published data indicate that the use of additional therapies, such as Intravenous (i.v.) fat emulsion (20% intralipid, 100 mL) and adsorption haemoperfusion cartridge filters, has had limited success.
Case Report
A 54-year-old male, smoker and a chronic alcoholic, working as a farmer, presented to the Emergency Department with an alleged history of consuming 30 to 50 mL of glyphosate mixed with alcohol two days prior. The patient ingested glyphosate unintentionally under the influence of alcohol, according to the history narrated by his relatives who brought him to the hospital.
Two hours after ingestion, the patient developed multiple episodes (10-12) of vomiting, which were not associated with blood, and experienced watery, foul-smelling loose stools. He was first treated at a local hospital with gastric lavage, stabilised with i.v. fluids, i.v. pantoprazole 40 mg twice daily, and ondansetron 4 mg three times a day, and was discharged after a 48-hour stay. However, as vomiting and a burning sensation in the retrosternal area persisted over the next 1 to 2 days, he was referred to a tertiary care centre for further evaluation.
Blood investigations revealed an elevated creatinine level of 6.4 mg/dL with features of ureamia, for which he underwent immediate Haemodialysis (HD). An upper gastrointestinal endoscopy revealed a grade II hiatus hernia with corrosive oesophageal injury. Following three cycles of HD, the patient was discharged against medical advice and presented again to the emergency department at the current hospital.
On examination, the patient was conscious, oriented, and obeying commands. His pulse rate was 86 beats per minute, and his blood pressure was 100/70 mm Hg. His Oxygen Saturation (SpO2) in ambient air was 81%, for which 6 L of O2/min via a Hudson mask was initiated. The pupils were normal in size and reactive to light. Bilateral pitting pedal oedema was present. Auscultation of the chest revealed bilateral basal crepitations, more pronounced in the left infrascapular region.
Arterial blood gas analysis revealed metabolic acidosis with compensatory respiratory alkalosis, with the following values: pH 7.35, pCO2 28 mm Hg, HCO3 15.1 mmol/L, K+ 4.6 mmol/L, Na+ 134 mmol/L, and chloride 101 mmol/L. The comparison of the investigations performed at the previous hospital with the current laboratory investigations, which show mild anaemia, elevated serum creatinine, initial hyperkalaemia, mild transaminitis, and elevated Brain Natriuretic Peptide (BNP) levels has been depicted in [Table/Fig-1].
Showing the investigations performed at previous hospital and current laboratory investigations.
| S. No. | Investigations | Done in previous hospital | Done during current admission | Normal cut-off |
|---|
| 1. | Haemoglobin | 9.9 g/dL | 9.8 g/dL | 12-17 g/dL |
| Total white cell counts | 6,900 cells/mm3 | 5850 cells/mm3 | 4,000-11,000 cells/ mm3 |
| Platelets | 1.48 lacs/mm3 | 1.46 lacs/mm3 | 1.5-4.5 lacs/mm3 |
| 2. | Renal function test: |
| Blood Urea Nitrogen (BUN) | 39 mg/dL | 37 mg/dL | 7-18 mg/dL |
| Serum creatinine | 6.5 mg/dL | 6.4 mg/dL | 0.6-1.3 mg/dL |
| 3. | Serum electrolytes: |
| Sodium | 130 mmol/L | 134 mmol/L | 134-144 mmol/L |
| Potassium | 5.8 mmol/L | 4.6 mmol/L | 3.5-5 mmol/L |
| Chloride | - | 101 mmol/L | 96-108 mmol/L |
| Bicarbonate | - | 17 mmol/L | 21-29 mmol/L |
| Calcium | - | 8.9 mg/dL | 8.5-10.1 mg/dL |
| Phosphate | - | 5.8 mg/dL | 2.5-4.9 mg/dL |
| 4. | Serum uric acid | - | 4.3 mg/dL | 2.6-7.2 mg/dL |
| 5. | Cardiac markers: |
| Troponin I | - | 0.03 ng/mL | 0.00-0.02 ng/mL |
| Brain natriuretic peptide | - | >5000 pg/mL | >100 pg/mL |
| CKMB | - | 1.5 ng/mL | 0.0-4.3 ng/mL |
| 6. | Venous lactates | - | 2.6 mmol/L | 0.60-1.40 mmol/L |
| 7. | Liver function test: |
| Total bilirubin | - | 0.53 mg/dL | 0.1-1.2 mg/dL |
| SGOT | - | 53 IU/L | 0-35 IU/L |
| SGPT | - | 27 IU/L | 0-41 IU/L |
*SGOT: Serum glutamic oxaloacetic acid transaminase; SGPT: Serum glutamic pyruvic transaminase; CKMB: Creatine kinase myocardial band
The patient was initially stabilised with intravenous (i.v.) fluids and treated for hyperkalaemia with 10 mL of 10% calcium gluconate i.v. They were nebulised with salbutamol and administered 10 units of regular insulin in 100 mL of 25% dextrose in the emergency room. The patient was later transferred to the intensive care unit for further management.
A chest X-ray showed ill-defined homogeneous opacities noted in the bilateral mid and lower zones, with blunting of the bilateral costophrenic angles and cardiomegaly observed [Table/Fig-2]. The electrocardiogram and Ultrasonography (USG) of the abdomen were normal. However, echocardiography revealed moderate Left Ventricular (LV) systolic dysfunction with grade II diastolic dysfunction, an ejection fraction of 35%, and moderate pulmonary artery hypertension (56 mmHg). Cardiac markers were elevated, with troponin I at 0.03 ng/mL and BNP levels exceeding 5000 pg/mL, suggesting possible cardiotoxicity.
Chest X-ray (CHX) on admission showing homogenous opacities.
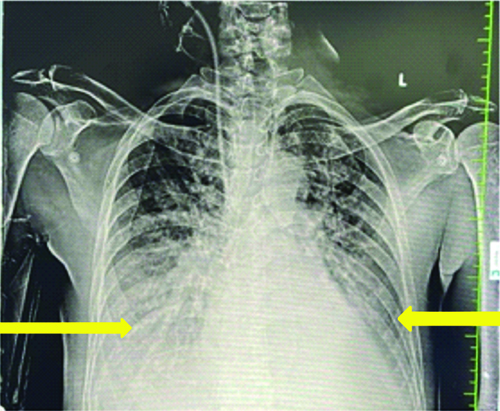
The patient required support from non invasive ventilation due to moderate Acute Respiratory Distress Syndrome (ARDS), with a PaO2/FiO2 ratio of 115 mm Hg. A pantoprazole infusion was administered for 24 hours in light of corrosive esophageal injury. Empirical antibiotics were started, with a renal-adjusted dose of piperacillin-tazobactam {(2.25 gms i.v. three times a day (TDS)}, due to bilateral infiltrates on the chest X-ray and catheter-associated urinary tract infection. This treatment was continued for a total of 14 days.
Once the patient was completely evaluated, a diagnosis of glyphosate poisoning with Multiorgan Dysfunction (MOD) was made, characterised by pulmonary, cardiac, upper gastrointestinal, and renal toxicity. Due to deranged renal parameters, continuous veno-venous hemodiafiltration was initiated. The patient underwent a total of three cycles of haemodialysis. Blood cultures grew gram negative bacilli, Acinetobacter, which was sensitive to piperacillin-tazobactam; therefore, intravenous treatment with piperacillin-tazobactam was continued for 14 days in light of bacteraemia. Regular monitoring of renal parameters indicated a declining trend throughout the hospitalisation [Table/Fig-3].
Shows renal function tests over the period of hospitalisation.
| Cycle of Haemodialysis (HD) | BUN(mg/dL) | Serum creatinine(mg/dL) |
|---|
| 1st cycle: |
| Pre-HD | 40 | 7.3 |
| Post-HD | 26 | 5.2 |
| 2nd cycle: |
| Pre-HD | 36 | 6.0 |
| Post-HD | 24 | 3.9 |
| 3rd cycle: |
| Pre-HD | 32 | 4.6 |
| Post-HD | 21 | 2.4 |
| At discharge | 8 | 0.8 |
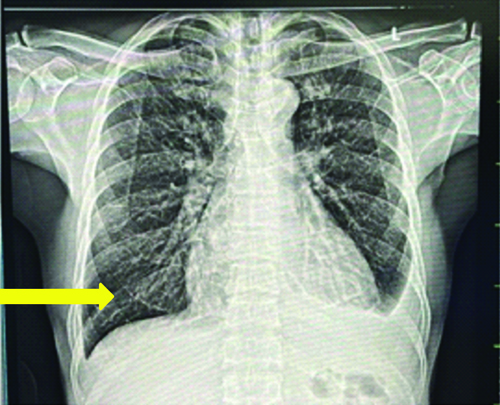
As the patient’s clinical condition improved, they were weaned off non invasive ventilation and dialysis, and successfully discharged on day 19 following hospitalisation with stable haemodynamics. Upon discharge, renal parameters had normalised (s.creatinine: 0.8 mg/dL), lung shadows had resolved, and the patient was maintaining an SpO2 of 99% in ambient air.
On follow-up after two weeks, the patient remained stable without any symptoms. Repeat echocardiography showed mild LV systolic dysfunction {Ejection Fraction (EF)-45%} and normal pulmonary artery pressure. A repeat chest X-ray showed complete resolution of opacities compared to the initial CXR at admission, with only minimal left costophrenic angle blunting [Table/Fig-4].
Chest X-ray showing complete resolution of opacities.
Discussion
The chemical substance observed in glyphosate is N-(phosphonomethyl)-glycine (C3H8NO5P), which is commercially available as Roundup®. Other adjuvant substances include POEA, which are derived from amine di-ethoxylates and aimed to increase the absorption of glyphosate by plants, thereby improving its effectiveness as a herbicide [1]. Glyphosate is believed to be less toxic to humans than to other organisms due to variations in chemical pathways and/or metabolism between species; however, this may not always be the case [2]. The toxic dose in humans is not well established.
The toxicity of this pesticide can present with a wide range of clinical symptoms, from asymptomatic to fatal. For glyphosate poisoning, intensive supportive therapy is the cornerstone of treatment since, there is no known antidote [3]. The reported mortality rate ranges from 4 to 11.2% [4-7]. Despite early detection and vigorous treatment, the triad of metabolic acidosis, hyperkalemia, and pulmonary oedema has been shown to have a fatal prognosis and can be associated with mortality [5]. The mainstay of care for glyphosate toxicity is supportive care. Following exposure, it is vital to perform skin decontamination with soap and water.
Mahendrakar K et al., reported a case of a patient who presented within an hour of consuming the poison and was treated with supportive measures, such as vasopressors, ventilation, and renal support, along with an intravenous fat emulsion (20% intralipid, 100 mL) [6]. More recent haemoperfusion cartridges, HA130, HA230, and HA330, are typically employed in conjunction with dialysis techniques and were developed in the field of extracorporeal adsorption blood purification techniques [7]. Additional research has been conducted to estimate the safety and efficacy characteristics of molecules in the 10-60 kDa range [8]. In a case report by Chakraborty S et al., H230 cartridges were used to manage acute tubular necrosis caused by glyphosate poisoning, and they observed that the patient improved within 72 hours [7]. The ingested volume of glyphosate has a significant association with adverse outcomes and prognosis [5]. Fluid loss and hypovolemia result in hypotension, which must be corrected with intravenous fluids and blood products. In present case report, the authors observed a failing myocardium, which precluded the use of excess intravenous fluid to treat hypotension.
Kim YH et al., in their retrospective study of 232 patients with glyphosate poisoning, found that serum lactate levels (>4.7 mmol/L), a prolonged QTc interval (>495 ms), and hyperkalaemia (>5.5 mmol/L) were independent predictors of mortality at 30 days [2]. Measurement of serum lactate on admission can be used as point-of-care testing for predicting mortality among patients with glyphosate poisoning. Serum levels of glyphosate greater than 734 μ/mL are associated with fatality [4].
Conclusion(s)
The present case report aimed to raise awareness about the relatively rare and potentially fatal poisoning caused by the widely available herbicide glyphosate. Glyphosate exposure may lead to renal failure, congestive heart failure, and intractable pulmonary oedema, which can result in mortality if, left untreated. Since, the herbicide lacks a specific antidote, early aggressive treatment can significantly reduce mortality.
*SGOT: Serum glutamic oxaloacetic acid transaminase; SGPT: Serum glutamic pyruvic transaminase; CKMB: Creatine kinase myocardial band
[1]. Carvalho FP, Glyphosate, the herbicide that become a nightmare and the precautionary principleInternational Journal of Environmental Studies 2020 77(6):1012-23.10.1080/00207233.2020.1773682 [Google Scholar] [CrossRef]
[2]. Kim YH, Lee JH, Cho KW, Lee DW, Kang MJ, Lee KY, Prognostic factors in emergency department patients with glyphosate-surfactant intoxication: Point-of-care lactate testingBasic Clin Pharmacol Toxicol 2016 119(6):604-10.10.1111/bcpt.1262427224736 [Google Scholar] [CrossRef] [PubMed]
[3]. Kunapareddy T, Kalisetty S, Glyphosate poisoning-A case reportJ Postgrad Med 2021 67:36-38.10.4103/jpgm.JPGM_766_2033533750 [Google Scholar] [CrossRef] [PubMed]
[4]. Roberts DM, Buckley NA, Mohamed F, A prospective observational study of the clinical toxicology of glyphosate-containing herbicides in adults with acute self-poisoningClin Toxicol (Phila) 2010 48(2):129-36.10.3109/1556365090347649120136481 [Google Scholar] [CrossRef] [PubMed]
[5]. Stella J, Ryan M, Glyphosate herbicide formulation: A potentially lethal ingestionEmerg Med Australas 2004 16:235-39.10.1111/j.1742-6723.2004.00593.x15228468 [Google Scholar] [CrossRef] [PubMed]
[6]. Mahendrakar K, Venkategowda PM, Rao SM, Mutkule DP, Glyphosate surfactant herbicide poisoning and managementIndian J Crit Care Med 2014 18:328-30.10.4103/0972-5229.13250824914265 [Google Scholar] [CrossRef] [PubMed]
[7]. Chakraborty S, Dey P, Singh P, Bhardwaj SS, Sen D, Bose A, A case report on glyphosate poisoningAsian Journal of Pharmaceutical and Clinical Research 2022 15(12):03-05.10.22159/ajpcr.2022.v15i12.46819 [Google Scholar] [CrossRef]
[8]. Ankawi G, Fan W, Montin DP, Lorenzin A, Neri M, Caprara C, A new series of sorbent devices for multiple clinical purposes: Current evidence and future directionsBlood Purif 2019 47:94-100.10.1159/00049352330253409 [Google Scholar] [CrossRef] [PubMed]