Congenital Heart Disease (CHD) is one of the most common developmental anomalies seen in children and there is an increased risk of developing oral disease and its systemic effects in children with CHD. The present case report highlights the dental management of a 10-year-old boy with CHD and dextrocardia. The diagnosis for the patient included dextrocardia (where the position of the heart is developmentally changed from the left to the right-side), complete atrioventricular septal defect and double outlet right ventricle with pulmonary stenosis. After consultation, diagnosis and treatment planning and upon obtaining consent from the parents and modifying the child’s behaviour, the dental needs of the child were addressed on a visit-by-visit basis. A quadrant approach was adopted to complete the extractions of all retained carious primary teeth, followed by restorative treatment. Oral prophylaxis was performed, followed by topical fluoride application and the patient was then referred to the Department of Orthodontics for treatment of malalignment. This case report focuses on the guidelines followed for antibiotic prophylaxis against Infective Endocarditis (IE) and highlights the importance of maintaining good oral health for this group of patients. The dental management of children with CHD can be complex, as oral health is often neglected by both parents and patients. Cardiovascular problems can significantly impact both the child and the parent, affecting management and financial implications. The dental considerations require early diagnosis of dental problems and prompt treatment to prevent complications and difficulties in implementing treatment due to systemic repercussions. The present case report aimed to improve dental care for children with severe systemic alterations, as there is a lack of scientific literature regarding the dental management of paediatric patients with CHD.
Antibiotic prophylaxis, Dental health services, Heart defects, Infective endocarditis
Case Report
A 10-year-old boy, previously diagnosed by medical professionals with dextrocardia and pulmonary stenosis, came for his first dental visit at the Department of Paediatric and Preventive Dentistry with a chief complaint of misaligned teeth. The medical history was evaluated. The child was delivered at 37 weeks of gestation and there were no unfavourable outcomes related to the pregnancy and delivery. He is the only son of the couple, who have two daughters, in a moderately educated family setting from a non consanguineous marriage. There is no family history of congenital anomalies.
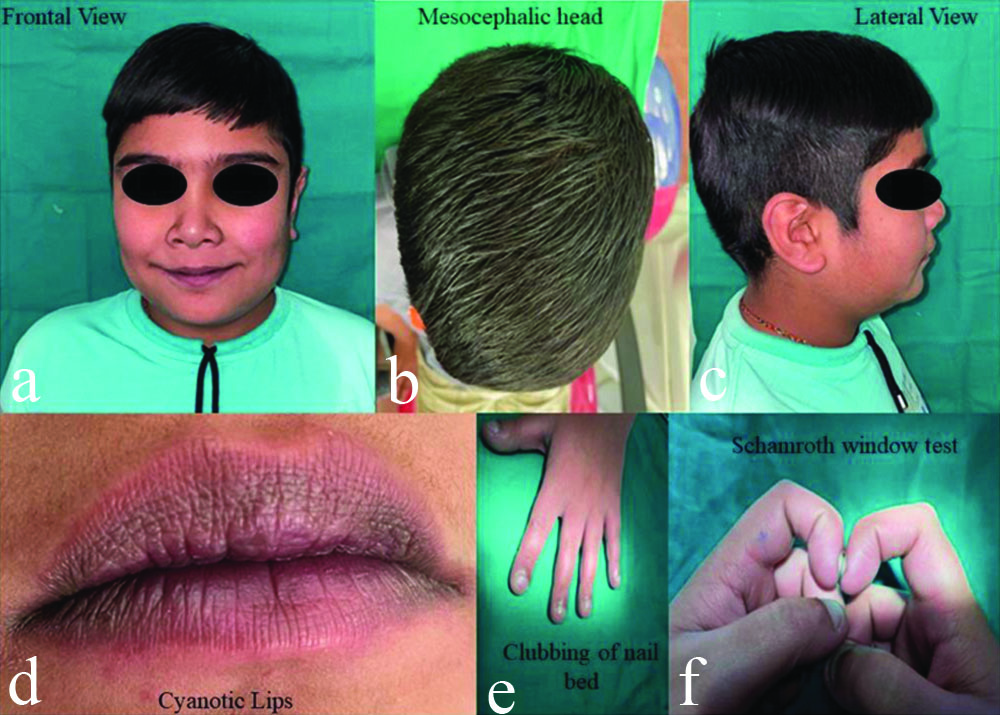
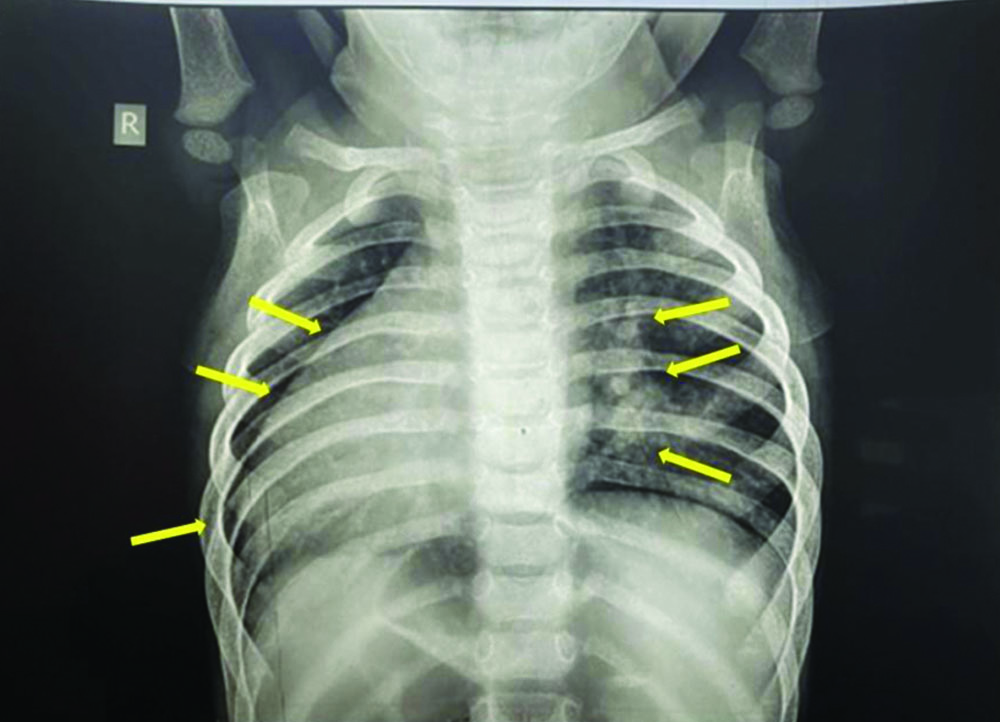
Physical examination revealed that the overall growth and development were delayed, though the child had good intellectual status. He had a mesocephalic head, cyanotic lips and clubbing of the nail beds on his upper and lower limbs, which was confirmed by the Schamroth window test [Table/Fig-1] [1]. The facial profile was convex. A chest X-ray revealed hilar/subhilar patchy consolidations with evidence of cardiomegaly/dextrocardia (situs inversus) [Table/Fig-2]. The patient was not taking any medications for this condition.
Physical examination of a child: a) Frontal view; b) Mesocephalic head; c) Lateral view; d) Cyanotic lips; e) Clubbing of nail bed; f) Schamroth window test [1].
Chest X-ray reveals hilar/subhilar patchy consolidations with evidence of cardiomegaly/dextrocardia (situs inversus).
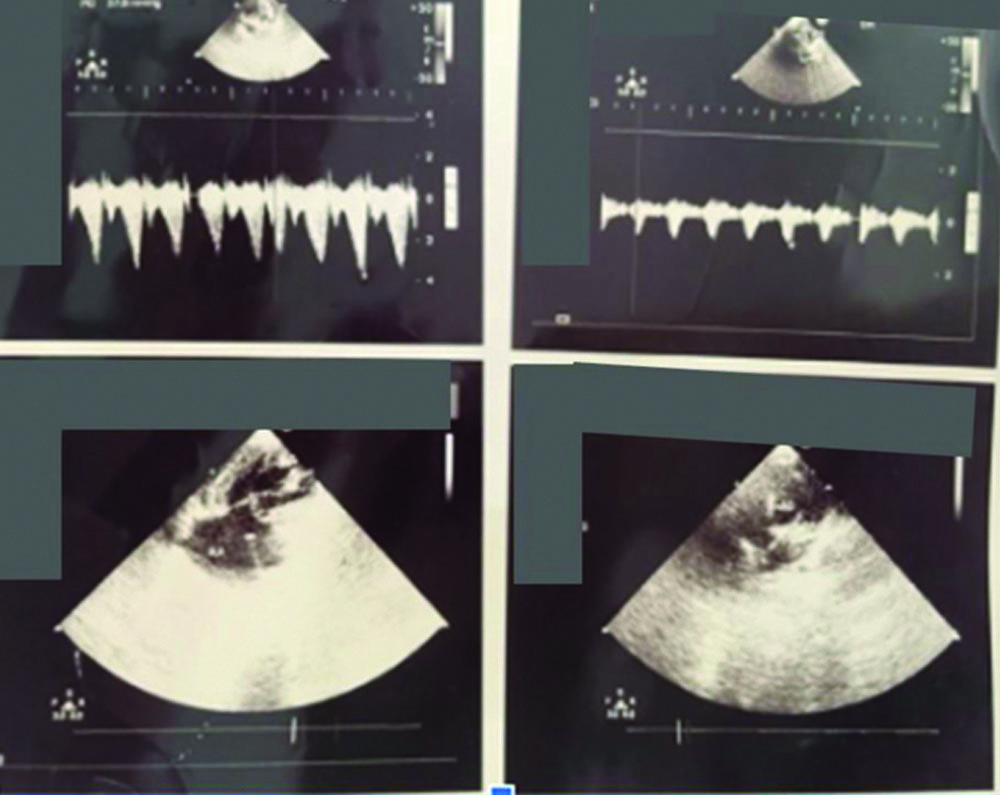
His chest colour Doppler and echocardiogram revealed CHD with dextrocardia, complete atrioventricular septal defect, double outlet right ventricle and pulmonary stenosis, which were diagnosed three months prior to his first dental visit to the Department. There was no evidence of Infective Endocarditis (IE) [Table/Fig-3]. The child’s behaviour was rated as positive according to the Frankl behaviour rating scale.
A 2D colour doppler and echocardiograph.
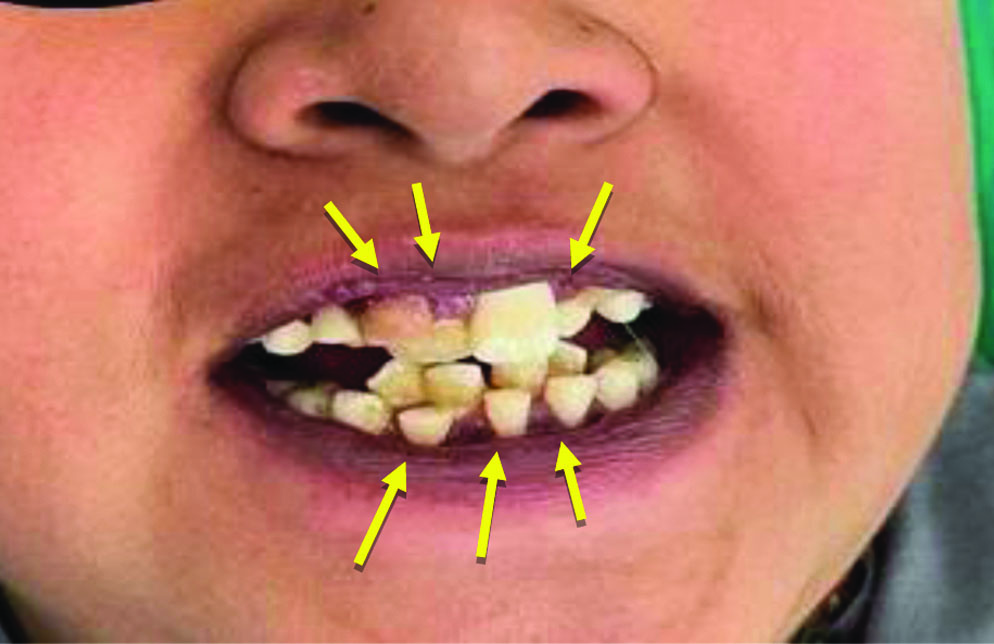
Intraoral soft-tissue examination revealed a red, bumpy tongue with enlarged taste buds, known as “strawberry tongue” [Table/Fig-4]. The child was in the mixed dentition stage with completely erupted teeth 16, 26, 36 and 46. Retained deciduous teeth were present: 51, 52, 62, 71, 72 and 82. Angle’s Class I molar relation was present on both sides. A deep bite was noted. Stains (++) and calculus (+) were present [Table/Fig-5]. The patient used non fluoridated toothpaste and brushed once a day in the morning.

Preoperative intraoral picture showing retained deciduous teeth.
The orthopantomogram of the patient showed retained deciduous teeth numbered 51, 52, 62, 71, 72 and 82. The gonial angle, condylar heads and skeletal pattern of growth all appeared normal. [Table/Fig-6]. After assessing all these findings, the parents were advised to obtain a medical fitness certificate from the physician and to consult regarding the strawberry tongue. The paediatrician prescribed multivitamins for the strawberry tongue. The treatment plan was explained to the parents and after obtaining written consent, treatment was started with antibiotic prophylaxis using three tablets of Amoxicillin 500 mg one hour before the dental appointment, as the patient weighed 30 kg.
Orthopantomogram of the patient.

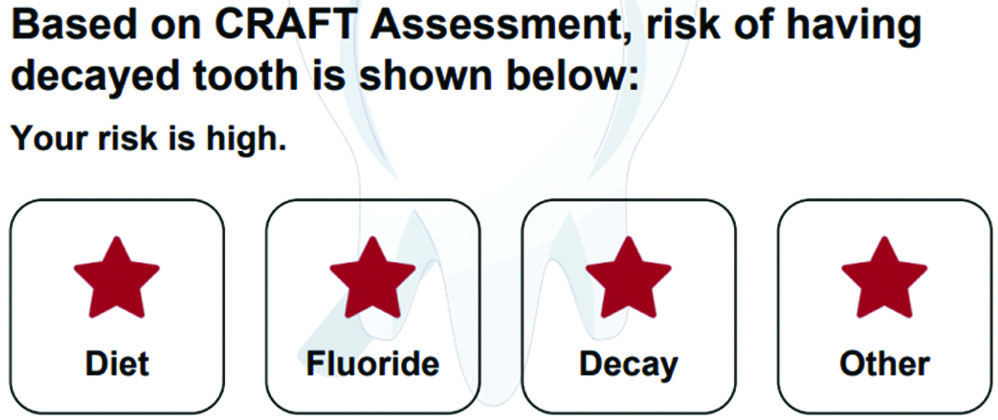
A caries risk assessment of the patient was calculated using the Caries Risk Assessment for Treatment (CRAFT) tool, which concluded that the patient had a high caries index [Table/Fig-7] [2].
Interpretation of caries risk assessment using CRAFT [2].
Two days later, the child’s second visit was scheduled, during which 2 mL of local anaesthesia without adrenaline (Lox 2%, Neon Laboratories Ltd., India) was administered, with 1 ml each delivered using buccal and palatal infiltration techniques. The retained primary teeth numbered 51, 52 and 62 were extracted. The procedure was uneventful and hemostasis was achieved using a gauze piece (pompom) and digital pressure. The patient was advised to continue the previously prescribed antibiotics and a tablet of paracetamol 250 mg was prescribed to be taken only if pain occurred.
The third visit was scheduled five days later. During this visit, the extraction of the lower retained primary teeth numbered 71, 72 and 82 was performed using the same technique [Table/Fig-8]. The fourth visit was scheduled 10 days later, during which oral prophylaxis was conducted, followed by the application of topical fluoride using acidulated phosphate fluoride (Pascal APF Fluoride gel, Pascal International Inc.) [Table/Fig-9].
Intraoral picture after extraction of deciduous teeth.

Post-treatment images after oral prophylaxis and fluoride application.

The child was advised to have a follow-up every three months until the complete eruption of the permanent teeth. Diet counselling for both the parent and child was provided, with instructions to reduce the consumption of sugar-containing foods and to increase the intake of fruits and vegetables. Furthermore, the child was advised to brush twice a day with fluoridated toothpaste and to rinse daily with a fluoridated mouthwash. The patient was also referred to the Department of Orthodontics for correction of the deep bite and convex profile.
Discussion
The CHD is defined by Mitchell SC et al., (1971) as a gross structural abnormality of the heart or intrathoracic great vessels that is actually or potentially of functional significance [3]. CHD and morphological changes of the heart are considered to be among the most common anomalies in newborn infants, with an incidence of eight out of 1,000 live births worldwide [4]. Dextrocardia refers to the positioning of the heart on the right-side of the thoracic cavity. It is a congenital anomaly that occurs during embryogenesis and results in anatomical left-right asymmetry [5].
Children with CHD have been found to have similar or poorer oral health compared to children without cardiac defects [6-9]. With the increased survival of patients with CHD, there comes an increased burden of complexity in managing these children’s oral health and disease. However, IE remains a major and serious complication in the dental management of patients with CHD. The presence of transient bacteraemia is considered one of the major risk factors in the pathogenesis of IE [10-15]. CHD itself seems to impact dentition, as enamel-forming cells are very sensitive to changes in metabolic conditions. Clinically, this is presented as thinner or softer teeth, making them more susceptible to dental caries [16]. One of the major reasons for the neglect of oral health appears to be the focus on the child’s heart disease, which remains central to the parents’ and child’s daily lives [17,18]. The management of such patients requires a balance between medical and dental faculties, based on the guidelines of the American Heart Association (AHA) [19].
Additionally, positional anomalies and crowding in the permanent dentition have been shown to be more prevalent in children with CHD [9]. It is essential that prior to prescribing drugs for dental purposes, appropriate consultation is made with the child’s physician [20]. Therefore, before proceeding with dental management, a medical fitness certificate should be obtained from the child’s cardiologist.
The child’s caries risk assessment was calculated using the mobile-based app CRAFT (Caries Risk Assessment For Treatment) and categorised the patient as high-risk [2]. According to the American Academy of Paediatric Dentistry (AAPD) revised guidelines for 2020-21, patients with CHD must be prescribed antibiotic prophylaxis to prevent the increased risk of developing IE [21]. Three tablets of Amoxicillin (500 mg) were prescribed to be taken one hour before the dental appointment as antibiotic prophylaxis.
Children with CHD experience difficulties in managing the usual stress associated with dental therapy. Reducing stress and anxiety is the primary goal in the successful dental management of these patients. Local anaesthetics play a major role in controlling pain in patients with CHD. The literature indicates that there is no absolute contraindication to the use of local anaesthetics containing vasoconstrictors [22]. However, adrenaline-containing local anaesthetics can affect the cardiovascular system [23]. An increase in cardiac output and stroke volume may occur if the concentration of adrenaline in the blood rises [24]. Therefore, to prevent this, the extractions of retained deciduous teeth were performed using local anaesthesia without vasoconstrictors.
Children with CHD are at an increased risk of oral diseases, which may further jeopardise their overall general health. As a preventive measure, oral prophylaxis followed by topical fluoride application was performed for the child.
Conclusion(s)
Children with CHD should have good access to dental care, as it is vital for their overall health. This access allows them to attain and maintain good oral health throughout their lives, limiting the need for complicated dental treatments and reducing their risk of IE. However, dental professionals encounter certain challenges when treating patients with CHD, such as high dental needs, complex medical histories, dental-related anxiety and a low level of awareness regarding the importance of oral health. Consequently, the priority given to oral care may be insufficient. The dental team plays a crucial role in regularly following up with patients who have CHD, providing enhanced prevention, proper diagnosis and effective management of their oral health.
[1]. Matsuura N, Schamroth signCMAJ 2019 191(45):E1251PMCID: PMC686115410.1503/cmaj.19051531712360 [Google Scholar] [CrossRef] [PubMed]
[2]. Thakur JH, Subhadra HN, Jawdekar A, Evaluation of CRAFT as a tool for caries risk assessment in 3- to 6-year-old children and its validation against Alban’s test: A pilot studyInt J Clin Paediatr Dent 2019 12(6):538-42.PMCID: PMC722938010.5005/jp-journals-10005-169832440071 [Google Scholar] [CrossRef] [PubMed]
[3]. Mitchell SC, Korones SB, Berendes HW, Congenital heart disease in 56,109 births. Incidence and natural historyCirculation 1971 43(3):323-32.10.1161/01.cir.43.3.3235102136 [Google Scholar] [CrossRef] [PubMed]
[4]. Bernier PL, Stefanescu A, Samoukovic G, Tchervenkov CI, The challenge of congenital heart disease worldwide: Epidemiologic and demographic factsSemin Thorac Cardiovasc Surg Paediatr Card Surg Annu 2010 13(1):26-34.10.1053/j.pcsu.2010.02.00520307858 [Google Scholar] [CrossRef] [PubMed]
[5]. Naaraayan A, Nimkar A, Acharya P, Pomerantz D, Jesmajian S, Dextrocardia: When right is wrong!J Atr Fibrillation 2020 13(2):2222PMCID: PMC869130710.4022/jafib.222234950286 [Google Scholar] [CrossRef] [PubMed]
[6]. Hallett KB, Radford DJ, Seow WK, Oral health of children with congenital cardiac diseases: A controlled studyPaediatr Dent 1992 14(4):224-30.1303520 [Google Scholar] [PubMed]
[7]. Stecksén-Blicks C, Rydberg A, Nyman L, Asplund S, Svanberg C, Dental caries experience in children with congenital heart disease: A case-control studyInt J Paediatr Dent 2004 14(2):94-100.10.1111/j.1365-263x.2004.00531.x15005697 [Google Scholar] [CrossRef] [PubMed]
[8]. Balmer R, Bu’Lock FA, The experiences with oral health and dental prevention of children with congenital heart diseaseCardiol Young 2003 13(5):439-43.10.1017/s104795110300092114694938 [Google Scholar] [CrossRef] [PubMed]
[9]. Tasioula V, Balmer R, Parsons J, Dental health and treatment in a group of children with congenital heart diseasePaediatr Dent 2008 30(4):323-28.18767512 [Google Scholar] [PubMed]
[10]. Warnes CA, Liberthson R, Danielson GK, Dore A, Harris L, Hoffman JI, Task force 1: The changing profile of congenital heart disease in adult lifeJ Am Coll Cardiol 2001 37(5):1170-75.10.1016/s0735-1097(01)01272-411300418 [Google Scholar] [CrossRef] [PubMed]
[11]. Knirsch W, Haas NA, Uhlemann F, Dietz K, Lange PE, Clinical course and complications of infective endocarditis in patients growing up with congenital heart diseaseInt J Cardiol 2005 101(2):285-91.10.1016/j.ijcard.2004.03.03515882677 [Google Scholar] [CrossRef] [PubMed]
[12]. Droz D, Koch L, Lenain A, Michalski H, Bacterial endocarditis: Results of a survey in a children’s hospital in FranceBr Dent J 1997 183(3):101-05.10.1038/sj.bdj.48094329282451 [Google Scholar] [CrossRef] [PubMed]
[13]. Martin JM, Neches WH, Wald ER, Infective endocarditis: 35 years of experience at a children’s hospitalClin Infect Dis 1997 24(4):669-75.10.1093/clind/24.4.6699145742 [Google Scholar] [CrossRef] [PubMed]
[14]. Li W, Somerville J, Infective endocarditis in the grown-up congenital heart (GUCH) populationEur Heart J 1998 19(1):166-73.10.1053/euhj.1997.08219503191 [Google Scholar] [CrossRef] [PubMed]
[15]. Saiman L, Prince A, Gersony WM, Paediatric infective endocarditis in the modern eraJ Paediatr 1993 122(6):847-53.10.1016/s0022-3476(09)90006-38501558 [Google Scholar] [CrossRef] [PubMed]
[16]. Berger EN, Attitudes and preventive dental health behaviour in children with congenital cardiac diseaseAust Dent J 1978 23(1):87-90.10.1111/j.1834-7819.1978.tb02878.x274933 [Google Scholar] [CrossRef] [PubMed]
[17]. Koerdt S, Hartz J, Hollatz S, Heiland M, Neckel N, Ewert P, Prevalence of dental caries in children with congenital heart diseaseBMC Paediatr 2022 22(1):711PMCID: PMC974350510.1186/s12887-022-03769-236510161 [Google Scholar] [CrossRef] [PubMed]
[18]. Schulz-Weidner N, Logeswaran T, Schlenz MA, Krämer N, Bulski JC, Parental awareness of oral health and nutritional behaviour in children with congenital heart diseases compared to healthy childrenInt J Environ Res Public Health 2020 17(19):7057PMCID: PMC757959710.3390/ijerph1719705732992501 [Google Scholar] [CrossRef] [PubMed]
[19]. Stout KK, Daniels CJ, Aboulhosn JA, Bozkurt B, Broberg CS, Colman JM, 2018 AHA/ACC guideline for the management of adults with congenital heart disease: A report of the American College of Cardiology/American Heart Association Task Force on clinical practice guidelinesJ Am Coll Cardiol 2019 73(12):e81-e192. [Google Scholar]
[20]. FitzGerald K, Fleming P, Franklin O, Dental health and management for children with congenital heart diseasePrim Dent Care 2010 17(1):21-25.10.1308/13557611079030769020067687 [Google Scholar] [CrossRef] [PubMed]
[21]. American Academy of Paediatric DentistryAntibiotic prophylaxis for dental patients at risk for infectionThe Reference Manual of Paediatric Dentistry 2019 Chicago, Ill.American Academy of Paediatric Dentistry:416-21. [Google Scholar]
[22]. Jastak JT, Yagiela JA, Donaldson D, Local Anesthesia of the Oral Cavity 1995 2 EdSaunders [Google Scholar]
[23]. Niwa H, Sugimura M, Satoh Y, Tanimoto A, Cardiovascular response to epinephrine-containing local anaesthesia in patients with cardiovascular diseaseOral Surg Oral Med Oral Pathol Oral Radiol Endod 2001 92(6):610-16.10.1067/moe.2001.11890311740477 [Google Scholar] [CrossRef] [PubMed]
[24]. Kjellberg SR, Rudhe U, Sjostrand T, The effect of adrenaline on the contraction of the human heart under normal circulatory conditionsActa Physiol Scand 1952 24(4):333-49.10.1111/j.1748-1716.1952.tb00849.x14952315 [Google Scholar] [CrossRef] [PubMed]