Introduction
Diabetic Neuropathy (DN) is a well known difficult to treat microvascular complication of diabetes. Based on Nerve Conduction Velocity (NCV) studies, DN has been classified into various types. Many possible aetiologies have been proposed. C-Reactive Protein (CRP) plays a role in the development of diabetic microvascular complications, while Homocysteine (Hcys) can harm the endothelium by inducing excessive sulfation of connective tissue.
Aim
To study the levels of Hcys and CRP in NCV-proven patients with DN and to associate these levels with the type of DN.
Materials and Methods
This was a cross-sectional study conducted at a semi-urban medical college hospital in Western Maharashtra, India, between February 2022 and May 2024. The study included 70 patients over 18 years of age with NCV-proven DN in Type 2 Diabetes Mellitus (DM), in whom serum Hcys and CRP levels were evaluated. Data collected were analysed using Statistical Package for Social Sciences (SPSS) software version 26.0.
Results
A total of 32 female participants (45.7%) and 38 male participants (54.3%). Among the study participants, 23 (32.9%) had a duration of diabetes of 5-10 years, and 47 (67.1%) had a mixed type of neuropathy. Elevated Hcys levels were observed in 18 (25.7%) participants, while 49 (70%) showed elevated CRP levels. CRP levels were raised in the mixed type of neuropathy, with 35 (71.4%) affected, while elevated Hcys levels were observed among the sensory neuropathies in 6 (33.3%) participants.
Conclusion
No significant association was found between elevated Hcys and CRP levels and the type of neuropathy.
Introduction
Diabetes is a persistent metabolic disorder characterised by increased levels of blood glucose, commonly referred to as blood sugar [1]. DN is a medical condition that occurs when the peripheral and autonomic nerve systems are damaged, leading to a variety of clinical symptoms. It is the most common type of neuropathy. Neuropathy, also known as nerve injury, can manifest with various symptoms that may occur throughout the body or in localised regions. The pathogenesis of this condition is primarily defined by metabolic and inflammatory damage that specifically affects the peripheral nerves responsible for transmitting motor and sensory signals. Diabetic Peripheral Neuropathy (DPN) significantly increases the risk of developing ulcers and amputations in the lower extremities, ultimately leading to disability [2,3].
Risk factors associated with the onset and progression of Diabetic Sensory Polyneuropathy (DSP) include an HbA1c level greater than 7%, male gender, insulin therapy, being ethnically non-Hispanic Black, advanced age, longer duration of DM, dyslipidemias, albuminuria, and a history of Systemic Hypertension (SH) [4].
Progressive DN is characterised by the retraction and degeneration of sensory axons in the peripheral nervous system, while the cell bodies remain relatively intact. The pattern of involvement in DN, known as the “stocking and glove” pattern, indicates that damage primarily affects the longest sensory axons. This means that the loss of distal leg epidermal axons occurs before the loss in more proximal limbs. Due to this characteristic, DN is classified as a length-dependent neuropathy. While DN is not primarily classified as a demyelinating neuropathy, it does affect Schwann cells. In more severe cases of DN, individuals may exhibit signs of demyelination [5].
The C-reactive Protein is a biomarker that indicates inflammation in the body. CRP is a member of the pentraxin family, and the liver is the main organ responsible for synthesising this acute phase reactant. High concentrations of CRP in the blood result from trauma, inflammatory conditions, and acute infections [6]. There is evidence suggesting that CRP plays a role in the development of diabetic microvascular problems, including retinopathy, nephropathy, and neuropathy. High levels of glucose can lead to changes in small blood vessels and an increase in the production of inflammatory substances such as TNF-α, IL-6, and CRP [7].
Homocysteine (Hcys) is a sulfur-containing amino acid generated from methionine, and it is known to be toxic and non proteinogenic. It occupies a junction where several metabolic pathways intersect and is synthesised from methionine through several transmethylation processes [8,9]. Prior research has indicated that Hcys can harm the endothelium by inducing excessive sulfation of connective tissue [8,9].
Thus, DN is a common and debilitating complication of diabetes, leading to significant morbidity. Early identification of biomarkers that correlate with the type and severity of neuropathy can aid in better management and prognosis. Therefore, the present study was undertaken to understand how Homocysteine (Hcys) and CRP levels relate to different types of DN, which could provide valuable insights for personalised treatment strategies and help identify patients at higher risk for more severe forms of neuropathy.
To study Hcys and CRP levels in NCV-proven patients with DN and to associate serum Hcys and CRP levels with the type of DN.
Materials and Methods
This cross-sectional study was conducted at a semi-urban medical college hospital in Western Maharashtra, India, from February 2022 to May 2024. The study targeted known cases of Type 2 Diabetes with NCV-proven neuropathy. Participants were recruited from the general medicine wards, the Diabetes Outpatient Department (OPD), and among those admitted to the wards. The study protocol received approval from the Institutional Ethics Committee (IESC/PGS/260/2022).
Inclusion criteria: Patients aged 18-80 years with Type 2 DM and NCV-proven neuropathy were included.
Exclusion criteria: Patients with Neuropathy due to other causes and patients on vitamin B12 supplements were excluded from the study.
Sample size calculation: Considering the prevalence of DN at 18.84% in the study “Prevalence and Risk Factors for Severity of DN in Type 2 DM” by Rani PK et al., with a 95% confidence interval and an acceptable difference of 9.8%, the calculated sample size was 62 [10]. The software used for this calculation was WinPepi. Therefore, selecting a sample size of 70 aligns with established research norms and ensures comparability with existing literature. Informed written consent was obtained from all patients. Purposive sampling was employed, selecting all consecutive cases of NCV-proven DN that met the inclusion criteria until the desired sample size was achieved.
Study Procedure
Clinical histories were recorded, the duration of diabetes was noted, and clinical examinations were conducted. Blood samples were drawn randomly under aseptic conditions to measure serum Hcys and CRP. The samples were centrifuged to separate serum and plasma. Serum Hcys levels were measured using the chemiluminescence immunoassay method (laboratory normal range: 5.08-15.39 micromol/liter), and serum CRP levels were measured using the nephelometry method (laboratory normal range: up to 5.0 mg/L).
Statistical Analysis
Data were collected using pre-formed data collection and case record forms. Data entry was performed in Microsoft excel and analysed using Statistical Package for Social Sciences (SPSS) software version 26.0. Categorical variables were expressed in terms of frequency and percentage, while continuous variables were expressed in terms of mean and SD. The association between various study parameters was analysed using the Chi-square test or Fisher’s exact test, with p-value ≤0.05 considered significant.
Results
The mean age of study participants was 57.6±10.71 years (range: 18-80 years). Out of 70 participants, the majority were in the age group of 51-60 years (22, 31.4%) and 61-70 years (22, 31.4%). Of the participants, 38 (54.3%) were male and 32 (45.7%) were female, resulting in a male-to-female ratio of 1.2:1. Additionally, 23 (32.9%) patients had diabetes for a duration of 5-10 years. The mean duration of diabetes among participants was 12.0±7.06 years (range: 1-32 years) [Table/Fig-1].
Demographic characteristics of study patients.
| Parameters | Frequency | Percent |
|---|
| Age group (years) | <40 | 4 | 5.7 |
| 40-50 | 14 | 20 |
| >50-60 | 22 | 31.4 |
| >60-70 | 22 | 31.4 |
| >70 | 8 | 11.4 |
| Gender | Female | 32 | 45.7 |
| Male | 38 | 54.3 |
| Diabetes duration | Upto 5 years | 10 | 14.3 |
| 5-10 years | 23 | 32.9 |
| >10-15 years | 18 | 25.7 |
| >15-20 years | 9 | 12.8 |
| >20 years | 10 | 14.3 |
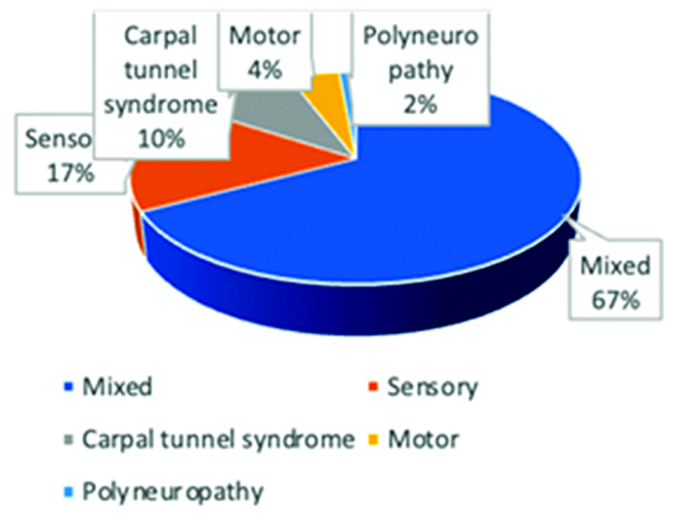
Out of the 70 participants, 47 (67.1%) had mixed neuropathy, 12 (17.1%) had pure sensory neuropathy, 7 (10%) had carpal tunnel syndrome, 3 (4.3%) had pure motor neuropathy, and 1 (1.4%) had polyneuropathy [Table/Fig-2].
Distribution of study participants according to type of neuropathy.
Normal serum Hcys levels were found in 52 (74.3%) participants, while 18 (25.7%) patients had raised serum Hcys levels [Table/Fig-3]. A total of 49 (70%) patients had raised CRP levels [Table/Fig-4].
Homocysteine (Hcys) findings of study participants.
| Homocysteine (Hcys) | Frequency | Percentage |
|---|
| Normal (5.08-15.39 micromol/litre) | 52 | 74.3 |
| Raised (>15.39 micromol/litre) | 18 | 25.7 |
| Total | 70 | 100 |
C-reactive protein findings of study participants.
| CRP | Frequency | Percentage |
|---|
| Normal (upto 5.0 mg/L) | 21 | 30 |
| Raised (>5 mg/l) | 49 | 70 |
| Total | 70 | 100 |
[Table/Fig-5] shows the relationship between the type of DN and Hcys values. Upon analysing the study findings using the Chi-square test, there was no significant association between raised Hcys levels and the type of DN (p-value=0.307). Similarly, there was no significant association between raised serum CRP levels and the type of DN among the study participants (p-value=0.426) [Table/Fig-6].
Relation of type of DN with Homocysteine (Hcys) values.
| Type of DN | Homocysteine (Hcys) | p-value |
|---|
| Normal | Raised |
|---|
| Mixed | 36 (69.2%) | 11 (61.1%) | 0.307 |
| Sensory | 6 (11.5%) | 6 (33.3%) |
| Carpal tunnel syndrome | 6 (11.5%) | 1 (5.6%) |
| Motor | 3 (5.8%) | 0 |
| Polyneuropathy | 1 (1.9%) | 0 |
| Total | 52 (74.3%) | 18 (25.7%) |
*p-value was calculated by using Chi-square test
Relation of type of DN with CRP values.
| Type of DN | C-reactive Protein (CRP) | p-value |
|---|
| Normal | Raised |
|---|
| Mixed | 12 (57.2%) | 35 (71.4%) | 0.426 |
| Sensory | 5 (23.8%) | 7 (14.3%) |
| Carpal tunnel syndrome | 3 (14.3%) | 4 (8.2%) |
| Motor | 1 (4.8%) | 2 (4.1%) |
| Polyneuropathy | 0 | 1 (2.0%) |
| Total | 21 (30.0%) | 49 (70.0%) | |
*p-value was calculated by using Chi-square test
Discussion
The present study aimed to investigate Hcys and CRP levels in NCV-proven patients with DN and to associate serum Hcys and CRP levels with the type of DN. The study found no significant association between raised Hcys and CRP levels and the type of DN. This study revealed that most of the participants, i.e., 47 (67.1%), had mixed neuropathy, 12 (17.1%) had pure sensory neuropathy, 7 (10%) participants had carpal tunnel syndrome, 3 (4.3%) participants had pure motor neuropathy, and 1 (1.4%) participant had polyneuropathy. A study conducted by Papanas N and Ziegler D observed that patients with Distal Sensorimeter Polyneuropathy (DSPN) frequently suffer from Diabetic Autonomic Neuropathy (DAN) [11]. A study conducted by Fahmy E et al., found that 57.69% of patients had distal sensory polyneuropathy, 23.08% had both distal sensory polyneuropathy and lower motor facial palsy, and 19.23% had distal sensory-motor polyneuropathy [12]. The ankle reflex was absent in 18 individuals, accounting for 69.23% of the total, and reduced in eight patients, representing 30.77%. Twelve individuals (46.15%) exhibited a deficit in deep sensation.
In the present study, the mean duration of diabetes among participants was 12.0±7.06 years (range: 1-32 years). A study conducted by Rujaswini T et al., revealed that the mean duration of diabetes was 3.18±1.6 years in participants without neuropathy and 5.71±1.8 years in participants with neuropathy [13]. A study conducted by Lin XY et al., observed that the mean duration of diabetes in patients with DN was 8.82±4.75 years [14]. Another study conducted by Doupis J et al., reported that the mean duration of diabetes among study participants was 20±13 years [15].
This study revealed raised serum Hcys levels in only 18 (25.7%) participants. Hcys plays a role in the progression of DN in individuals with type 2 diabetes, and high levels of Hcys are likely linked to DN [16]. A study conducted by Rujaswini T et al., revealed that the mean serum Hcys level without DN was 6.8±2.9, while the serum Hcys level with DN was 21.6±0.29, with a p-value of 0.0017 [13]. The association between serum Hcys and DN was found to be statistically significant (p-value=0.001). A study conducted by Ambrosch A et al., showed that the frequency of hyperhomocysteinemia was significantly greater in patients with DN compared to those without neuropathy [17]. This suggests that Hcys is independently associated with the prevalence of DN in a group of type 2 diabetic patients. Cohen JA et al., found a significant correlation between total Hcys (tHcy) and DAN [18]. However, there was no correlation between tHcy and Diabetic Sensorimotor Peripheral Neuropathy (DSPN). Their conclusion suggests that hyperhomocysteinemia may be a risk factor for DAN, but not for diabetic Sensorimotor Polyneuropathy (DSPN). This may be associated with unequal damage to small nerve fibers.
A case-control study conducted by Fahmy E et al., examined 42 participants, including 26 diabetic individuals and 16 healthy individuals [12]. The study found that diabetic patients had significantly higher plasma levels of Hcys compared to the control group (p-value=0.001). Furthermore, elevated serum Hcys levels were found to be associated with the presence of DN in type 2 diabetic patients. A study conducted by Guo H et al., showed that patients with DN exhibited higher levels of serum Hcys compared to those without DN [16]. Additionally, there was a strong correlation between hyperhomocysteinemia and an elevated risk of DPN in individuals diagnosed with type 2 diabetes. Hcys serves as a biomarker for DN and shows potential for use in preventing or treating this condition.
In this study, 70% of the patients had raised CRP levels; however, no significant association was found between the type of neuropathy and raised CRP levels. A study conducted by Banait T et al., revealed a significant correlation between elevated blood CRP levels and an increased risk of developing type 2 DM and neurodegenerative disorders [19]. A study conducted by Kang ES et al., found that there were no differences between the mean serum high-sensitivity CRP (hsCRP) levels of those with and without neuropathy (p-value >0.05) [20]. Najafi L et al., observed a significant difference in serum hsCRP levels between patients with nephropathy and those without nephropathy (p-value=0.003) [21]. Hassaan A et al., found that CRP levels were non-significantly higher in diabetic patients with microvascular complications compared to those without complications (p-value=0.35) [22]. Aslam M and Chandrasekhara P discovered a significant positive correlation between hsCRP levels and microvascular complications (p-value <0.0001) [23].
Previous studies by Hassaan A et al., and Aslam M suggested that Hcys may damage the endothelium through excessive sulfation of connective tissues [22,23], while vascular risk factors have been linked to DN. Therefore, Hassaan A et al., and Aslam M and Chandrasekhara P hypothesised that the status of Hcys is associated with the risk and progression of neuropathy in type 2 diabetes [22,23]. In addition to increased levels of Hcys, high levels of CRP have also been found to be associated with diabetic polyneuropathy and some neuropathic deficits. The treatment of DN has always been challenging and has never been completely successful. Various aetiologies have been proposed. In this study, comparing Hcys levels and CRP levels among the various types of DN revealed that mixed types of diabetic neuropathies had higher serum CRP levels, indicating inflammation possibly due to end glycation products, while sensory DN showed higher serum Hcys levels. Thus, B12 supplementation may yield better results in this context.
Limitation(s)
The cross-sectional nature of this study design limits the inference of a causal relationship between the correlates and DPN. Therefore, the present findings need to be confirmed in prospective studies with larger sample sizes.
Conclusion(s)
A total of 25.7% of the participants showed raised Hcys levels, and 70% showed raised CRP levels. No significant association was found between raised Hcys and CRP levels and the type of neuropathy. However, mixed-type DN had elevated CRP levels, indicating a possible inflammatory process. These findings highlight the need for further research with larger sample sizes to validate these associations and enhance treatment approaches.
*p-value was calculated by using Chi-square test
*p-value was calculated by using Chi-square test
[1]. Kasper D, Fauci A, Hauser S, Longo D, Jameson J, Loscalzo J, Harrison’s principles of internal medicine 2015 19 ediNew York, NY, USAMcgraw-Hill [Google Scholar]
[2]. Pearson ER, McCrimon RJ, Diabetes mellitusIn: Davidson’s Principles and Practice of Medicine E-Book 2022 23rd ediLondon, EnglandElsevier Health Sciences [Google Scholar]
[3]. Chandalia HB, Tripathy BB, RSSDI Textbook of Diabetes Mellitus 2020 4th edJP Medical Ltd:121:163-250. [Google Scholar]
[4]. Chawla R, Chawla S, Diabetic Neuropathy. In: Joshi S, editorRSSDI Textbook of Diabetes Mellitus 2020 4th edJP Medical Ltd:121:163-250. [Google Scholar]
[5]. Kahn RC, Weir GC, King GL, Jacobson AM, Moses AL, Smith RJ, Joslin’s Diabetes Mellitus 2007 4th edLippincott Williams & Wilkins [Google Scholar]
[6]. Sloan G, Shillo P, Selvarajah D, Wu J, Wilkinson ID, Tracey I, A new look at painful diabetic neuropathyDiabetes Res Clin Pract 2018 144:177-91.Epub 2018 Sep 710.1016/j.diabres.2018.08.02030201394 [Google Scholar] [CrossRef] [PubMed]
[7]. Black S, Kushner I, Samols D, C-reactive ProteinJ Biol Chem 2004 279(47):48487-90.Epub 2004 Aug 2610.1074/jbc.R40002520015337754 [Google Scholar] [CrossRef] [PubMed]
[8]. Gasecka A, Siwik D, Gajewska M, Jaguszewski MJ, Mazurek T, Filipiak KJ, Early biomarkers of neurodegenerative and neurovascular disorders in diabetesJ Clin Med 2020 9(9):280710.3390/jcm909280732872672 [Google Scholar] [CrossRef] [PubMed]
[9]. Starkebaum G, Harlan JM, Endothelial cell injury due to copper-catalyzed hydrogen peroxide generation from homocysteineJ Clin Invest 1986 77(4):1370-76.10.1172/JCI1124423514679 [Google Scholar] [CrossRef] [PubMed]
[10]. Rani PK, Raman R, Rachapalli SR, Pal SS, Kulothungan V, Sharma T, Prevalence and risk factors for severity of diabetic neuropathy in type 2 diabetes mellitusIndian J Med Sci 2010 64(2):51-57.10.4103/0019-5359.9440022466493 [Google Scholar] [CrossRef] [PubMed]
[11]. Papanas N, Ziegler D, Risk factors and comorbidities in diabetic neuropathy: An update 2015Rev Diabet Stud 2015 12(1-2):48-62.10.1900/RDS.2015.12.4826676661 [Google Scholar] [CrossRef] [PubMed]
[12]. Fahmy E, Amer H, Rabah AM, El-Fayoumy N, Mokhtar H, Estimation of serum homocysteine level in patients with type 2 diabetic neuropathyEgypt J Neurol Psychiat Neurosurg 2010 47(1):59-66. [Google Scholar]
[13]. Rujaswini T, Praveen D, Chowdary PR, Aanandhi MV, Shanmugasundaram P, A review on association of serum homocysteine in diabetic neuropathyDrug Invention Today 2018 10(2):154-56. [Google Scholar]
[14]. Lin XY, Sun T, Yu RX, Tang YL, Li HY, Correlation between elevated serum homocysteine level and the development of diabetic peripheral neuropathy: A comparative study and meta-analysisInt J Clin Exp Med 2016 9(2):2857-64. [Google Scholar]
[15]. Doupis J, Lyons TE, Wu S, Gnardellis C, Dinh T, Veves A, Microvascular reactivity and inflammatory cytokines in painful and painless peripheral diabetic neuropathyJ Clin Endocrinol Metab 2009 94(6):2157-63.10.1210/jc.2008-238519276232 [Google Scholar] [CrossRef] [PubMed]
[16]. Guo H, Chen X, Zhang H, Zhang X, Serum homocysteine levels and diabetic neuropathy in patients with type 2 diabetes mellitus: A systematic review and meta-analysisInt J Clin Exp Med 2016 9(10):19588-94. [Google Scholar]
[17]. Ambrosch A, Dierkes J, Lobmann R, Kühne W, König W, Luley C, Relation between homocysteinaemia and diabetic neuropathy in patients with Type 2 diabetes mellitusDiabet Med 2001 18(3):185-92.10.1046/j.1464-5491.2001.00445.x11318838 [Google Scholar] [CrossRef] [PubMed]
[18]. Cohen JA, Jeffers BW, Stabler S, Schrier RW, Estascio R, Increasing homocysteine levels and diabetic autonomic neuropathyAuton Neurosci 2001 87(2-3):268-73.10.1016/S1566-0702(00)00262-911476288 [Google Scholar] [CrossRef] [PubMed]
[19]. Banait T, Wanjari A, Danade V, Banait S, Jain J, Role of High-sensitivity c-reactive protein (Hs-CRP) in non-communicable diseases: A reviewCureus 2022 14(10):e3022510.7759/cureus.30225 [Google Scholar] [CrossRef]
[20]. Kang ES, Kim HJ, Ahn CW, Park CW, Cha BS, Lim SK, Relationship of serum high sensitivity C-reactive protein to metabolic syndrome and microvascular complications in type 2 diabetesDiabetes Res Clin Pract 2005 69(2):151-59.10.1016/j.diabres.2004.11.01416005364 [Google Scholar] [CrossRef] [PubMed]
[21]. Najafi L, Malek M, Valojerdi AE, Khamseh ME, Acute phase proteins and diabetes microvascular complicationsInternational Journal of Diabetes in Developing Countries 2016 36:10-17.Available for: https://www.academia.edu/80807674/Acute_phase_proteins_and_diabetes_microvascular_complications10.1007/s13410-015-0389-x [Google Scholar] [CrossRef]
[22]. Hassaan A, El-Ghany A, Mohamed I, Eldars W, Othman TA, Correlation between highly sensitive C reactive protein and development of microvascular complications of type 2 diabetes mellitusEgyptian Journal of Medical Microbiology 2022 31(1):69-73.10.21608/ejmm.2022.211968 [Google Scholar] [CrossRef]
[23]. Aslam M, Chandrasekhara P, Correlation of fibrinogen and HsCRP with microvascular complications of type 2 diabetes mellitusIJHSR 2016 6(5):25-32. [Google Scholar]