Orthodontic therapy is frequently sought for Class-II Division 1 malocclusion, which is characterised by a convex facial profile, lip strain, lip trap and proclination of the maxillary anterior teeth [1]. A major goal of orthodontic treatment is to improve facial aesthetics and maintain or enhance the labial contours of the upper and lower lips [2]. It has long been acknowledged that the primary objective of orthodontic therapy is to achieve a harmonious facial appearance. For Class-II patients, maxillary premolar extraction effectively modifies the soft-tissue profile. The extraction of upper premolars is often chosen as an alternative to orthognathic surgery for non growing Class-II patients with significant overjet [3]. The protocol for extraction therapy leads to cephalometric modifications such as an increased nasolabial angle, upper lip retraction, maxillary incisor uprighting and a straighter profile [4]. Therefore, orthodontic therapy may indirectly result in soft-tissue alterations to the facial profile in addition to changing the dentoskeletal framework [1].
Knowledge of the facial skeleton and its overlying soft-tissue is essential for determining facial harmony [5]. Few studies have focused on the impact of alterations in the mandibular development pattern on the facial profile. Blanchette ME et al., found that individuals with vertical growth had longer and thicker soft-tissue drapes than patients with short facial patterns [6]. This outcome was attributed to a compensatory process that created a normal facial profile while concealing the vertical dysplasia. According to Macari AT and Hanna AE adults with hyperdivergent patterns had thinner soft-tissue at gnathion and mention than adults with normal or hypodivergent patterns [7]. Therefore, it is necessary to consider any alterations in the mandibular plane during treatment planning, as they may negatively impact facial profiles following treatment.
Several studies have shown changes in the soft-tissue profile of patients with Class-II malocclusion treated with maxillary premolar extraction, with or without mandibular premolar extraction [8-10]. However, the effects of divergence patterns in Class-II malocclusion patients treated with premolar extraction have not been investigated in detail. Additionally, there is limited orthodontic evidence to support the notion that individuals with Class-II malocclusion who underwent premolar extractions would have post-treatment profiles similar to those of Class-I patients.
The present study was designed to examine the changes in the soft-tissue profile between patients with a skeletal class-I relationship and a balanced facial profile, and patients with corrected Class-II malocclusion who have different mandibular growth patterns. To the best of the authors knowledge, the influence of growth pattern and first premolar extraction on the soft-tissue profile in Class-II division 1 subjects has not been studied in detail in the past. The present study is the first to investigate the soft-tissue parameters in detail.
Materials and Methods
The present cross-sectional cephalometric study was conducted in the Department of Orthodontics, Faculty of Dental Sciences, SGT University, Gurugram, Haryana, India, from June 2021 to December 2022. The study involved the collection of 210 lateral cephalograms from 120 patients who visited the Department of Orthodontics between June 2021 and July 2022. Ethical clearance was obtained from the Ethical Committee (FODS/EC/ORTHO/2021/04).
All adult orthodontic patients with the same ethnic background (North Indian population) had their pre and post-treatment cephalograms selected. The pre and post-treatment lateral cephalograms were divided into four groups. The pretreatment cephalograms of 30 patients with Class-I malocclusion and a balanced facial profile were used for the control group (group-1), who had visited the department for orthodontic treatment. One hundred and eighty pre and post-treatment cephalograms of patients with Class-II malocclusion were used as experimental groups (groups-2-4).
Inclusion criteria: The inclusion criteria for the control group were an ANB angle of 2°±2°, an overjet of 1-2 mm, an FMA angle of 22°-28°, and a balanced facial profile. The inclusion criteria for the experimental group were an ANB angle of 6°±1°, an overjet of 5-9 mm, a full complement of permanent dentition with or without third molars, and a convex soft-tissue profile.
Exclusion criteria: Patients with history of orthognathic surgery, missing permanent first molars and any congenital anomalies were excluded from the study.
Sample size calculation: G*Power Software (version 3.0.10) was used to calculate the sample size. With an effect size of 0.4 [11], a precision level of 5%, a confidence level of 95% and 80% power, the trial produced a total of 84 patients, with 21 in each group.
Study Procedure
The experimental groups were further subclassified into three groups based on the FMA. Group-2 (n=30) was classified as having a horizontal growth pattern (FMA<22°), group-3 (n=30) was classified as having an average growth pattern (FMA=22°-28°), and group-4 (n=30) was classified as having a vertical growth pattern (FMA>28°) [12].
All patients in the experimental groups underwent treatment involving the extraction of all first premolars with an MBT prescription (0.022 slot). Anterior retraction was carried out using loops or elastomeric chains on 0.019×0.025 Stainless Steel (SS) wire. All cases were finished in Class-I occlusion with a 1-2 mm overjet. After the removal of brackets, the patients were given bonded lingual retainers in the lower arch and Hawley retainers in the upper arch. The average treatment time was 20 to 24 months.
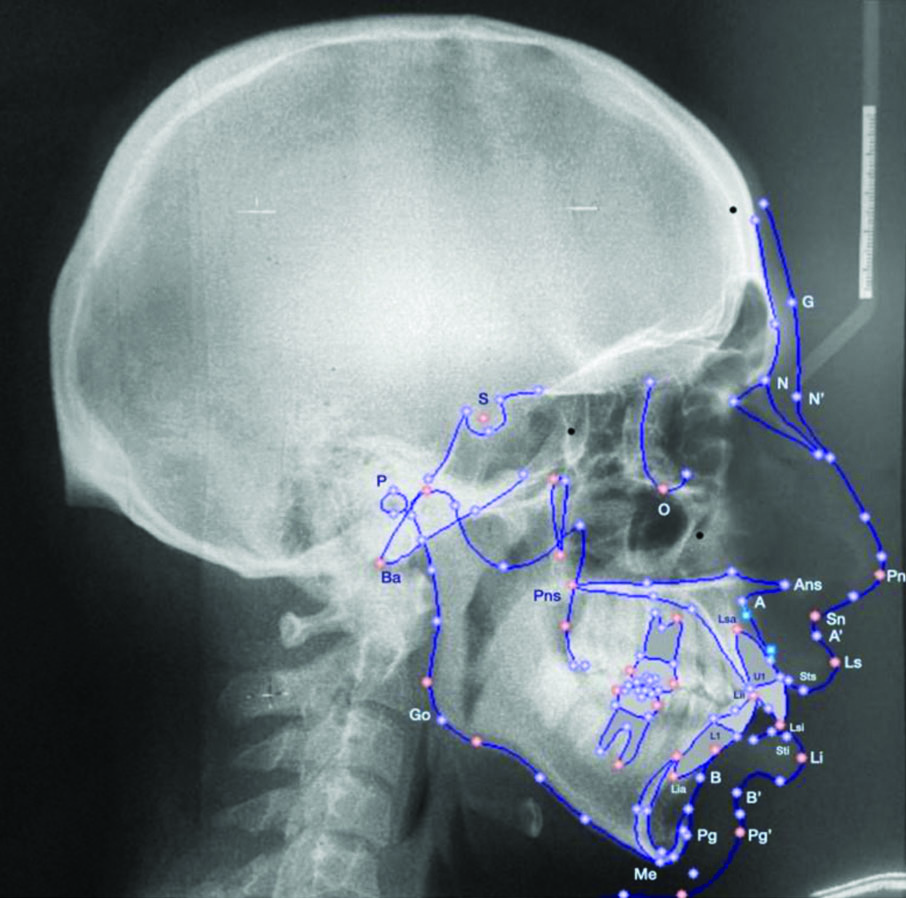
All digital radiographs were analysed using the NemoCeph software (Digital cephalometric system, version 11.0, Nemotec). The skeletal and soft-tissue parameters used in the study are given in [Table/Fig-1] and illustrated in [Table/Fig-2].
Cephalometric parameters used in the study.
| Skeletal parameters |
| SNA (°) |
| SNB (°) |
| ANB (°) |
| SN-MP (°) |
| FMA (°) |
| Dental parameters |
| U1-NA (°) |
| U1-NA (mm) |
| L1-NB (°) |
| L1-NB (mm) |
| IMPA (°) |
| Soft-tissue parameters |
| Basic upper lip thickness (mm) |
| Upper lip thickness (mm) |
| Upper lip strain (mm) |
| Lower lip thickness (mm) |
| Subnasale to H line (mm) |
| Lower lip to H line (mm) |
| Upper lip to E line (mm) |
| Lower lip to E line (mm) |
| Upper lip length (mm) |
| Lower lip length (mm) |
| Nasolabial angle (°) |
| H angle (°) |
| Soft-tissue contour (mm) |
| Hard tissue contour (mm) |
| Soft-tissue Profile angle (°) |
| Soft-tissue chin thickness (mm) |
| Interlabial gap (mm) |
| Inferior labial sulcus depth (mm) |
| Facial convexity angle (°) |
| Upper lip protrusion (mm) |
SNA: Sella, nasion, A point; SNB: Sella, nasion, B point; ANB: Angle between the A point, nasion and B point; SN-MP: Sella-nasion/mandibular plane angle; FMA: Frankfort horizontal mandibular plane angle
Skeletal and soft-tissue landmarks.
Statistical Analysis
The data were tabulated using an Excel sheet. For statistical analysis, the means and standard deviations of each group’s measurements were calculated using SPSS software version 22.00 for Windows (SPSS Inc., Chicago, USA). A t-test was utilised to determine the differences between the groups, using a significance level of p-value <0.05. An analysis of variance, along with post-hoc Dunnett t-tests, was employed to compare the groups.
Results
The present study included 210 lateral cephalograms of 120 patients (52 males and 68 females) aged 18-28 years. All adult orthodontic patients had the same ethnic background (North Indian population), and their pre- and post-treatment cephalograms were selected.
The skeletal, dental and soft-tissue parameters were tabulated. [Table/Fig-3] shows the intragroup comparison of pre and post-treatment skeletal cephalometric parameters in all experimental groups. In all the experimental groups, there was an increase in the post-treatment Sella-nasion/Mandibular Plane (SN-MP) and FMA angles, but it was statistically significant only in groups-2 and 3 (p-value <0.05) when compared with the pretreatment values. Clinically, insignificant changes were observed in the ANB angle in all the experimental groups.
Intragroup comparison of pre and post-treatment skeletal cephalometric parameters within group-2, 3 and 4.
| Variables | Horizontal growth pattern (Group-2) | Average growth pattern (Group-3) | Vertical growth pattern (Group-4) |
|---|
| Mean | p-value | Mean | p-value | Mean | p-value |
|---|
| SNA (°) | Pre | 83.13±1.83 | 0.350 | 82.94±1.75 | <0.01* | 83.56±1.45 | 0.358 |
| Post | 83.27±1.86 | 83.23±1.76 | 81.06±15.1 |
| SNB (°) | Pre | 77.79±2.06 | 0.201 | 77.55±1.73 | 0.013* | 78.13±1.76 | <0.01* |
| Post | 78.01±1.96 | 77.88±1.73 | 78.54±1.67 |
| ANB (°) | Pre | 5.35±0.50 | 0.578 | 5.36±0.42 | 0.266 | 5.31±0.58 | 0.338 |
| Post | 5.30±0.42 | 5.29±0.52 | 5.22±0.438 |
| SN-MP (°) | Pre | 21.16±1.06 | <0.01* | 25.55±1.64 | 0.023* | 33.68±4.18 | 0.978 |
| Post | 23.46±2.21 | 26.93±2.82 | 33.64±4.67 |
| FMA (°) | Pre | 20.07±1.09 | <0.01* | 24.70±1.42 | 0.021* | 32.61±4.04 | 0.451 |
| Post | 22.43±2.22 | 25.99±2.82 | 32.90±4.88 |
*The p-value <0.05 was considered statistically significant
The intragroup comparison of pre and post-treatment dental cephalometric parameters in all experimental groups is shown in [Table/Fig-4]. In all the experimental groups, there was a significant decrease (p-value <0.01) in post-treatment values of upper incisor to NA (both angular and linear), lower incisor to NB (both angular and linear), and IMPA compared to pretreatment values.
Intragroup comparison of pre and post-treatment dental cephalometric parameters within groups-2, 3 and 4.
| Variables | Horizontal growth pattern (Group-2) | Average growth pattern (Group-3) | Vertical growth pattern (Group-4) |
|---|
| Mean | p-value | Mean | p-value | Mean | p-value |
|---|
| U1-NA (°) | Pre | 36.69±4.97 | <0.01* | 37.82±1.91 | <0.01* | 38.87±2.8 | <0.01* |
| Post | 21.64±1.83 | 21.71±2.42 | 22.89±2.12 |
| U1-NA (mm) | Pre | 10.71±1.78 | <0.01* | 10.91±1.57 | <0.01* | 11.91±1.63 | <0.01* |
| Post | 3.96±1.14 | 3.68±1.06 | 3.88±1.33 |
| L1-NB (°) | Pre | 34.98±6.07 | <0.01* | 37.52±3.14 | <0.01* | 37.43±3.1 | <0.01* |
| Post | 21.94±4.11 | 22.74±1.58 | 22.71±1.99 |
| L1-NB (mm) | Pre | 9.97±4.19 | <0.01* | 9.62±1.39 | <0.01* | 10.12±1.57 | <0.01* |
| Post | 4.66±3.36 | 3.59±0.94 | 3.81±0.98 |
| IMPA (°) | Pre | 106.26±18.98 | <0.01* | 108.84±4.33 | <0.01* | 107.72±2.68 | <0.01* |
| Post | 93.90±16.59 | 91.98±2.47 | 92.09±2.51 |
The comparison of pre and post-treatment soft-tissue cephalometric parameters within all experimental groups is tabulated in [Table/Fig-5]. In group-2, among the soft-tissue parameters, there was a significant increase (p-value <0.01) in post-treatment upper lip thickness, nasolabial angle and inferior labial sulcus depth. Additionally, there was a significant decrease (p-value <0.01) in post-treatment upper lip strain, lower lip to H line, upper lip to E line, interlabial gap, facial convexity angle and upper lip protrusion.
Intragroup comparison of pre and post-treatment soft-tissue cephalometric parameters within groups-2, 3 and 4.
| Variables | Horizontal growth pattern (Group-2) | Average growth pattern (Group-3) | Vertical growth pattern (Group-4) |
|---|
| Mean | p-value | Mean | p-value | Mean | p-value |
|---|
| Basic upper lip thickness (mm) | Pre | 17.72±16.92 | 0.547 | 14.51±1.85 | 0.023* | 15.54±2.04 | 0.909 |
| Post | 17.41±14.86 | 15.24±1.53 | 15.53±1.82 |
| Upper lip thickness (mm) | Pre | 10.058±1.59 | <0.01* | 9.98±1.66 | <0.01* | 10.72±1.44 | <0.01* |
| Post | 13.01±1.74 | 13.67±1.7 | 13.97±1.94 |
| Upper lip strain (mm) | Pre | 4.89±1.66 | <0.01* | 4.74±1.92 | <0.01* | 5.46±2.98 | <0.01* |
| Post | 2.10±2.09 | 1.61±0.81 | 1.55±0.64 |
| Lower lip thickness (mm) | Pre | 13.64±2.44 | 0.142 | 13.69±2.08 | 0.020 | 13.76±2.43 | 1.00 |
| Post | 12.99±2.91 | 14.48±2.49 | 13.76±2.54 |
| Subnasale to H line (mm) | Pre | 7.34±3.04 | 0.065 | 8.24±2.73 | <0.01* | 7.42±2.68 | 0.455 |
| Post | 6.09±3.83 | 6.75±2.23 | 6.97±2.26 |
| Lower lip to H line (mm) | Pre | 1.80±1.55 | <0.01* | 2.17±1.43 | <0.01* | 2.31±1.65 | <0.01* |
| Post | 0.82±1.29 | 1.24±1.17 | 0.90±0.93 |
| Upper lip to E line (mm) | Pre | 2.32±1.49 | <0.01* | 2.41±1.98 | <0.01* | 2.89±1.9 | <0.01* |
| Post | 1.54±1.20 | 1.26±1.41 | 1.38±1.25 |
| Lower lip to E line (mm) | Pre | 2.35±2.03 | 0.259 | 3.44±3.37 | <0.01* | 3.44±2.85 | <0.01* |
| Post | 1.60±3.75 | 1.58±1.88 | 0.99±1.02 |
| Upper lip length (mm) | Pre | 17.18±2.45 | 0.082 | 18.87±2.95 | 0.347 | 18.60±2.77 | 0.858 |
| Post | 18.70±5.76 | 18.47±3.93 | 18.54±3.28 |
| Lower lip length (mm) | Pre | 40.43±3.68 | 0.107 | 41.83±2.56 | 0.352 | 43.70±2.84 | 0.370 |
| Post | 43.92±12.75 | 41.33±4.17 | 44.14±2.56 |
| Nasolabial angle (°) | Pre | 95.95±8.20 | 0.001** | 92.27±16.89 | <0.01* | 94.43±5.27 | <0.01* |
| Post | 107.85±19.10 | 106.72±20.17 | 111.44±4.68 |
| H angle (°) | Pre | 20.70±2.95 | 0.080 | 25.32±7.24 | <0.01* | 21.97±2.69 | <0.01* |
| Post | 17.52±1.29 | 19.10±4.05 | 16.92±2.65 |
| Soft-tissue contour (mm) | Pre | 61.58±5.37 | 0.126 | 62.72±9.73 | 0.015 | 68.12±6.32 | 0.211 |
| Post | 62.15±5.29 | 63.45±9.6 | 68.87±6.7 |
| Hard tissue contour (mm) | Pre | 63.10±5.70 | 0.187 | 64.29±10.97 | 0.293 | 69.20±6.76 | 0.090 |
| Post | 67.55±19.73 | 64.79±9.98 | 70.24±6.54 |
| Soft-tissue profile angle (°) | Pre | 157.87±6.50 | 0.434 | 148.90±38.52 | 0.554 | 156.93±5.41 | 0.189 |
| Post | 162.04±29.31 | 151.96±49.53 | 164.09±29.79 |
| Soft-tissue chin thickness (mm) | Pre | 10.44±2.21 | 0.102 | 9.74±2.07 | 0.687 | 10.63±2.78 | 0.689 |
| Post | 9.82±3.20 | 9.56±3.25 | 10.78±3.16 |
| Interlabial gap (mm) | Pre | 5.163±2.61 | <0.01* | 6.45±3.21 | <0.01* | 6.16±3.13 | <0.01* |
| Post | 2.05±1.28 | 2.14±1.248 | 2.29±1.07 |
| Inferior labial sulcus depth(mm) | Pre | -6.12±1.13 | <0.01* | -5.34±1.83 | <0.01* | -6.14±1.03 | <0.01* |
| Post | -3.91±2.32 | -4.19±1.7 | -4.74±0.99 |
| Facial convexity angle (°) | Pre | 20.94±2.92 | <0.01* | 20.31±4.39 | <0.01* | 22.74±3.56 | <0.01* |
| Post | 15.27±2.76 | 14.46±3.31 | 16.04±2.80 |
| Upper lip protrusion (mm) | Pre | 5.67±2.03 | <0.01* | 6.88±2.01 | <0.01* | 6.35±2.0 | <0.01* |
| Post | 3.12±2.51 | 4.64±1.55 | 4.34±1.42 |
In group-3, among the soft-tissue parameters, there was a significant increase (p-value <0.01) in post-treatment upper lip thickness, nasolabial angle and inferior labial sulcus depth. Furthermore, there was a significant decrease (p-value <0.01) in post-treatment upper lip strain, subnasale to H line, lower lip to H line, upper lip to E line, lower lip to E line, H angle, interlabial gap, facial convexity angle and upper lip protrusion.
In group-4, among the soft-tissue parameters, there was a significant increase (p-value <0.01) in post-treatment upper lip thickness, nasolabial angle and inferior labial sulcus depth. There was also a significant decrease (p-value <0.01) in post-treatment upper lip strain, lower lip to H line, upper lip to E line, lower lip to E line, H angle, interlabial gap, facial convexity angle and upper lip protrusion.
An intergroup comparison of the post-treatment changes in the skeletal, dental, and soft-tissue cephalometric parameters is presented in [Table/Fig-6]. A significant change (p-value <0.001) in the post-treatment ANB angle was observed in group-2, followed by groups-3 and 4, when compared with group-1 [Table/Fig-7]. The post-treatment SN-MP and FMA angles of groups-2 and 4 showed a significant difference (p-value <0.001) when compared with group-1. The post lower lip to H line parameter of groups-2 and 4 was significantly different (p-value <0.01) when compared with group-1. The lower lip to the E line did not show any significant difference among the groups. The soft-tissue profile angle showed a significant change in group-3 when compared with group-1 (p-value=0.012).
Intergroup comparison of post-treatment changes in the skeletal, dental and soft-tissue cephalometric parameters.
| Variable | Group-2 | Group-3 | Group-4 | Group-1 | p-value | Post-hoc test |
|---|
| Skeletal parameters |
| SNA (°) | 83.27±1.86 | 83.23±1.76 | 81.06±1.10 | 82.571±1.17 | 0.39 | - |
| SNB (°) | 78.01±1.96 | 77.88±1.73 | 78.57±1.67 | 81.223±1.25 | 0.32 | - |
| ANB (°) | 5.30±0.42 | 5.29±0.52 | 5.22±0.43 | 1.347±0.27 | <0.01* | 2, 3, 4>1 |
| SN-MP (°) | 23.46±2.21 | 26.93±2.82 | 33.67±4.67 | 26.590±1.74 | 0.032* | 4>1 |
| FMA (°) | 22.43±2.22 | 25.99±2.82 | 32.90±4.88 | 25.468±1.83 | 0.026* | 4>1 |
| Dental parameters |
| U1-NA (°) | 21.64±1.83 | 21.71±2.42 | 22.89±2.12 | 23.974±1.67 | 0.47 | - |
| U1-NA (mm) | 3.96±1.14 | 3.68±1.06 | 3.88±1.33 | 4.077±0.84 | 0.40 | - |
| L1-NB (°) | 21.94±4.11 | 22.74±1.58 | 22.71±1.99 | 23.810±2.07 | 0.38 | - |
| L1-NB (mm) | 4.66±3.36 | 3.59±0.94 | 3.81±0.98 | 3.630±0.96 | 0.13 | - |
| IMPA (°) | 89.90±6.59 | 91.98±2.47 | 92.09±2.51 | 92.160±3.15 | 0.54 | - |
| Soft-tissue parameters |
| Basic upper lip thickness (mm) | 17.41±4.86 | 15.24±1.53 | 15.53±1.84 | 14.613±1.46 | 0.09 | - |
| Upper lip thickness (mm) | 13.02±1.74 | 13.67±1.70 | 13.98±1.94 | 12.915±1.55 | 0.33 | - |
| Upper lip strain (mm) | 2.10±2.09 | 1.61±0.81 | 1.55±0.64 | 1.749±0.58 | 0.15 | - |
| Lower lip thickness (mm) | 12.99±2.91 | 14.48±2.49 | 13.76±2.54 | 13.150±2.63 | 0.27 | - |
| Subnasale to H line (mm) | 6.09±3.83 | 6.75±2.23 | 6.97±2.26 | 6.165±2.49 | 0.39 | - |
| Lower lip to H line (mm) | 0.82±1.29 | 1.24±1.17 | 0.90±0.93 | 1.737±1.11 | 0.036* | 1>3, 4 |
| Upper lip to E line (mm) | 1.54±1.20 | 1.27±1.41 | 1.38±1.25 | 1.418±1.13 | 0.62 | - |
| Lower lip to E line (mm) | 1.60±3.75 | 1.58±1.88 | 0.99±1.02 | 0.825±1.03 | 0.013* | 2, 3, 4>1 |
| Upper lip length (mm) | 18.70±5.76 | 18.47±3.93 | 18.54±2.28 | 18.868±3.27 | 0.71 | - |
| Lowe lip length (mm) | 43.92±3.75 | 41.33±4.17 | 44.14±2.56 | 42.944±2.74 | 0.68 | - |
| Nasolabial angle (°) | 107.85±8.10 | 106.72±6.17 | 111.44±4.68 | 109.911±2.97 | 0.29 | - |
| H angle (°) | 17.52±3.29 | 19.10±4.05 | 16.92±2.65 | 15.063±1.86 | 0.45 | - |
| Soft-tissue contour (mm) | 62.15±5.29 | 63.46±9.6 | 68.87±6.70 | 65.238±2.07 | 0.29 | - |
| Hard tissue contour (mm) | 67.55±7.73 | 64.79±7.98 | 70.24±6.54 | 65.296±2.85 | 0.10 | - |
| Soft-tissue profile angle (°) | 162.05±2.31 | 151.97±4.43 | 164.09±2.9 | 170.084±2.74 | 0.032* | 1 >2 |
| Soft-tissue chin thickness (mm) | 9.82±3.20 | 9.56±3.25 | 10.78±2.30 | 10.631±3.86 | 0.43 | - |
| Interlabial gap (mm) | 2.05±1.28 | 2.14±1.24 | 2.30±1.27 | 2.160±0.67 | 0.70 | - |
| Inferior labial sulcus depth | -3.91±0.50 | -4.20±0.65 | -4.74±0.80 | -3.403±1.50 | 0.61 | - |
| Facial convexity angle | 15.27±2.78 | 14.46±2.25 | 16.04±2.54 | 14.531±2.65 | 0.74 | - |
| Upper lip protrusion | 3.12±0.80 | 4.64±1.5 | 4.34±1.75 | 3.900±0.98 | 0.35 | - |
After Post-hoc test application for the significant parameters (Dunnett test for comparison with control group).
| Variables | p-values | Significant findings |
|---|
| Group-1 vs Group-2 | Group-1 vs Group-3 | Group-1 vs Group-4 |
|---|
| Skeletal parameters | |
| ANB (°) | <0.001* | <0.001* | <0.001* | 2>1, 3>1, 4>1 |
| SN-MP (°) | <0.001* | 0.950 | <0.001* | 1>2, 4>1 |
| FMA (°) | <0.001* | 0.861 | <0.001* | 1>2, 4>1 |
| Soft-tissue parameters | |
| Lower lip to H line (mm) | <0.001* | 0.183 | 0.009* | 1>2, 1>4 |
| Lower lip to E line (mm) | 0.313 | 0.417 | 0.240 | - |
| Soft-tissue profile angle (°) | 0.243 | 0.012* | 0.972 | 1>3 |
Discussion
The present study was conducted to assess soft-tissue profile changes in Class-II Division 1 patients treated with the extraction of all first premolars, considering varied growth patterns.
In this study, all experimental groups demonstrated an increase in the post-treatment SN-MP and FMA angles; however, this increase was significant only in group-2 when compared to pretreatment values. The increase in post-treatment SN-MP and FMA angles may be attributed to the extrusive nature of orthodontic treatment and the subsequent clockwise rotation of the mandible, which leads to an opening of the bite [13]. During orthodontic therapy, Creekmore TD also observed a vertical eruption of the molars, which contributed to bite opening and was beneficial for patients with deep bites [13].
Clinically insignificant changes were noted in the SNA, SNB and ANB angles across all experimental groups. In all experimental groups (groups-2, 3 and 4), there was a significant decrease in post-treatment upper incisor to NA (both angular and linear), lower incisor to NB (both angular and linear), and IMPA compared to pretreatment values. These post-treatment parameters in the experimental groups were also comparable to those in group-1. Ali US et al., Anderson BD, and Maetevorakul S and Viteporn S also found that premolar extractions in the maxillary and mandibular arches of patients with Class-II Division 1 malocclusion resulted in more upright maxillary and mandibular incisors compared to non extraction cases [14-16].
There was a significant increase in post-treatment upper lip thickness compared to pretreatment values in all experimental groups. Talass MF et al., and Issacson JR et al., reported increases in upper lip thickness due to the retraction of the maxillary incisors [17,18]. Similarly, there was a significant decrease in post-treatment upper lip strain when compared with pretreatment values in all experimental groups. The current study revealed a strong association between the quantity of upper lip fall and the relief from lip strain caused by upper incisor retraction. More relief from lip strain also resulted in less severe upper lip taper and a closer upper lip-to-upper incisor retraction relationship. Similar findings were reported in studies conducted by Johnston DJ et al., Schudy FF and Murugesan A et al., [19-21].
In all experimental groups, there was a significant decrease in post-treatment lower lip to H line and upper lip to E line measurements compared with pretreatment findings. These post-treatment soft-tissue parameters were also comparable to those in group-1. This finding suggests that maxillary incisor retraction in the experimental groups produced a lip fall, thereby decreasing the upper lip to E line values and resulting in a comparable upper lip soft-tissue profile as seen in Class-I individuals, irrespective of their growth pattern. These findings are in accordance with the studies conducted by Mishra D et al., Ekstam M et al., and Fang ML et al., [22-24].
There was a significant increase (109±2 degrees) in the post-treatment nasolabial angle in all experimental groups when compared with pretreatment values (93±2 degrees). Mishra D et al. reported a similar increase in the nasolabial angle (107±2 degrees) [22]. This larger response in the nasolabial angle was probably related to the retraction of the upper lip during orthodontic treatment [22]. Similarly, there was a decrease in post-treatment H angle in all experimental groups, and it was comparable to individuals with a Class-I profile. Similar results were found in a study conducted by Basciftci FA and Usumez S in which they compared extraction and non extraction groups [25].
These findings suggest that first premolar extraction in skeletal Class-II patients achieved a soft-tissue profile comparable to that of group-1, irrespective of their growth pattern. In the present study, there was a significant decrease in the post-treatment interlabial gap, as well as, upper and lower lip protrusion in all experimental groups. The decrease in these parameters might be due to the retrusion of the upper and lower lips subsequent to the retraction of the maxillary and mandibular anterior teeth, which leads to a decrease in the interlabial gap. Similar findings were noted by Janson G et al., Albertini P et al., and Kochar GD et al., [26-28]. These studies observed that the extraction of premolars led to a significant reduction in the interlabial gap throughout the long-term treatment period.
Similarly, there was a significant difference in the post-treatment facial convexity angle among all experimental groups. Comparable results were observed in a study conducted by Chua AL et al., in which they compared the effects of extraction and non extraction cases on anterior facial height [29].
Limitation(s)
The present study did not investigate the gender-linked influence on the soft-tissue profile. Future longitudinal studies with large, gender-specific sample sizes are suggested to evaluate changes in the soft-tissue profile more effectively. Another limitation of the current study is that it was a two-dimensional study; therefore, the authors recommend conducting a three-dimensional study in the future.
Conclusion(s)
The present study was conducted to assess changes in the soft-tissue profile of Class-II division 1 patients treated with the extraction of all first premolars, considering different growth patterns, using lateral cephalograms. Angular and linear measurements in Class-II division 1 subjects were affected by the extraction of all first premolars during orthodontic treatment. Changes in dental parameters and alterations in the soft-tissue profile of Class-II Division 1 malocclusion subjects after retraction of the incisors were comparable to those in a skeletal Class-I group, regardless of their growth pattern. It is concluded that in mild to moderate cases of skeletal Class-II, an acceptable soft-tissue profile can be achieved with the extraction of premolars, irrespective of growth pattern.
*The p-value <0.05 was considered statistically significant