In today’s day and age, composite restorations have become a go-to option for everyday restorations due to their minimally invasive tooth preparation requirements, superior mechanical qualities and stunning aesthetics. Currently, dentin adhesive procedures encounter a challenge known as the “bonding era” problem. This problem is related to the long-term endurance of the hybrid layer, as research has demonstrated that the hybrid layer deteriorates over time [1]. A meta-analysis on the clinical success of posterior composite resin restorations reported a survival rate of 85-90% at the end of 10 years. The reasons for failures include fractures, loss of retention, loss of marginal integrity and unacceptable colour [2]. A suggested reason for these failures could be the degradation of the collagen matrix and hybrid layer over time [3,4]. Hence, the long-term structural durability of the hybrid layer plays a pivotal role and has been the focus of research in adhesion. The morphology, chemical composition and mechanical properties determine the structural durability of the hybrid layer [5].
Some strategies for increasing the durability of the hybrid layer include improving the mechanical properties and preventing hydrolysis of the hybrid layer [6]. A functional monomer, 10-methacryloyloxydecyl-dihydrogen Phosphate (10-MDP), is reported to increase bond strength by forming an insoluble MDP-calcium (MDP-Ca) salt [7]. These MDP-Ca salts are placed on the dentin collagen scaffold to prevent bond deterioration. MDP creates a stable collagen-phosphate complex by hydrogen bonding with the collagen in dentin. In addition, both free MDP and the MDP-Ca salt inhibit MMPs and exogenous proteases [8]. However, some researchers have reported that 2-Hydroxyethyl Methacrylate (HEMA) in 10-MDP-containing bonding agents suppresses nanolayers between 10-MDP and mineralised tissue, compromising the mechanical properties of the hybrid layer [9].
Another method to improve the hybrid layer aims to prevent hydrolysis. The pro MMPs trapped during dentin formation get activated under conditions of lowered pH, such as in carious processes or during acid etching. These MMPs degrade collagen fibres and polymerised hydrophilic resin. Hence, the application of CHX, an MMP and cathepsin inhibitor, has significantly increased bond strength [10].
The CHX is a broad-spectrum MMP inhibitor and cationic antimicrobial agent. The calcium and zinc ions found in MMPs undergo cation chelation, which underlies the inhibitory action. CHX can attach to collagen fibrils of demineralised dentin through electrostatic forces after filling the binding sites of MMP enzymes [11]. An in-vitro study that employed micro-Raman spectroscopy to assess the presence of CHX in the resin/dentin interface after five years of water storage provided clear evidence for this. The study focused on cases where CHX was used as an aqueous dentin pretreatment or included in the etchant [12]. However, CHX pretreatment with bonding agents containing 10-MDP demonstrated partial inhibition of collagenolytic activity. Giacomini MC et al., mentioned the need for further exploration of the negative impact of CHX when used with bonding agents containing 10-MDP in their research [13].
In a natural vegetarian diet, many fruits and vegetables are rich sources of minerals like calcium and phosphate. Vegetables from the gourd family are abundant in fibres, vitamins, essential minerals and antioxidants. Benincasa hispida, commonly known as ash gourd, is well-known for its nutritional and medicinal properties. The edible portion of B. hispida contains vitamin C, thiamine, riboflavin and vitamin E. Minerals such as sodium, potassium, calcium and phosphorus are also present in this vegetable. In traditional Indian medicine, the fresh juice of B. hispida is recommended as a source of good nutrition [14,15]. Ash gourd has been reported to improve bone health [16,17]. Since teeth and bones share hydroxyapatite in common, the dental application of B. hispida was considered. Therefore, in the present study, the authors explored the novel application of a B. hispida solution as a pretreatment for a dentin bonding agent. Moreover, as a natural product, it contains minerals in their purest form, eliminating any artificial components.
Currently, there is no research available on the effect of dentin pretreatment with B. hispida on adhesive bond quality. Thus, the present study aimed to evaluate the effects of different dentin surface pretreatments, such as CHX and Benincasa hispida, on the MSBS of coronal dentin using a universal testing machine with a 10 MDP-based universal adhesive system. Since the optimum concentration of B. hispida as a pretreatment for dentin bonding agents has not been established, the present study was conducted as a pilot study.
Materials and Methods
The present in-vitro pilot study was conducted at the Department of Conservative Dentistry and Endodontics, Vishnu Dental College, Bhimavaram, Andhra Pradesh, India, from May 2023 to November 2023. The Institutional Ethical Committee (IRB No: IECVDC/23/PG01/CE/IVT/5) approved the research protocol. The present research was executed in accordance with the Checklist for Reporting In-vitro Studies (CRIS) guidelines (equator.org). A convenience sample of 42 participants was selected.
Inclusion and Exclusion criteria: Forty-two human mandibular first molar teeth, freshly extracted due to poor periodontal health or for complete denture treatment, were selected for the present study. Teeth with carious and non carious lesions, crown or root fractures occurring during extraction and developmental anomalies were excluded.
Study Procedure
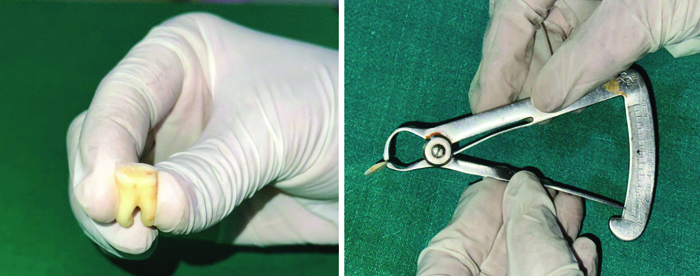
After ultrasonic scaling, the teeth were stored in a 0.5% thymol solution at 37°C. All the occlusal enamel was ground off using a diamond disc under water coolant and evaluated for the absence of enamel under a stereomicroscope (Olympus, Model SZX2-ILLT, Olympus Corporation, Shinjuku-ku, Tokyo, Japan) at magnifications of x12.5 and x20. A dentin slice approximately 1.0 mm thick was cut perpendicular to the long axis of each tooth from the upper middle coronal region using a low-speed diamond disk (Marathon M4 Micromotor) under water coolant [Table/Fig-1] [18]. The occlusal surfaces of the slices were ground with up to 600-grit silicon carbide paper to expose a flat dentin surface. The dentin slices were divided into three main groups (fourteen each): Group-I - no pretreatment, Group-II - CHX pretreatment and Group-III - B. hispida pretreatment, according to the surface pretreatments performed, using a randomisation technique (www.randomizer.org) [19].
A 1.0 mm thick dentin slice from upper middle coronal portion [18].
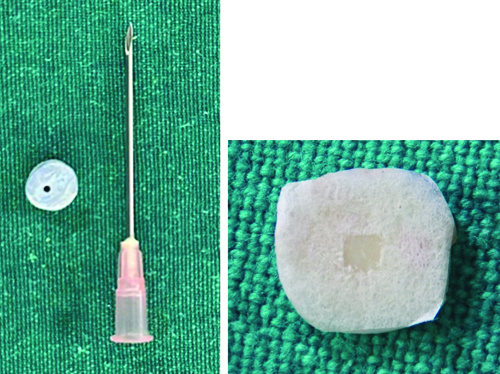
A putty impression of an 18-gauge needle with an outer diameter of 1.27 mm was made [20]. This was used as a matrix to prepare composite restorations with dimensions of 1.2 mm in diameter and 1 mm in height [Table/Fig-2] [21]. Surgical micropore adhesive tape was applied to the dentin disc, exposing only the bonding surface [Table/Fig-2] [22].
Putty impression and micropore taped specimen [22].
Preparation of B. Hispida juice: In June, the vegetable was purchased from the local market in Bhimavaram, Andhra Pradesh, India. It was washed thoroughly and peeled to obtain only the internal portion from which the juice was intended to be extracted. The equipment (grater) used to grate the pulp was dried in sunlight for a whole day to sterilise it. The juice was extracted from the grated pulp of the vegetable by squeezing it in a sterile cloth into a sterile container. It was used immediately for the surface pretreatment.
The dentin slices in all three groups were etched with 37% phosphoric acid (3M Scotchbond Multipurpose Etchant) for 15 seconds, followed by rinsing for 15 seconds. The excess moisture was removed with absorbent paper.
The dentin slices in Group-I did not receive any surface pretreatment, while Group-II and III underwent a passive application of 2% CHX solution (HexaChlor, Safe Endo Dental India Pvt. Ltd.,) and a passive application of freshly prepared B. hispida juice, respectively, for 30 seconds [Table/Fig-3]. The excess solution was removed using absorbent paper.
Two pretreatment materials.

All dentin slices were then treated with an active application of a layer of Dentin Bonding Agent containing 10-MDP (DBA) (Adper Single Bond Universal, 3M ESPE) [23] for 20 seconds, followed by solvent evaporation for five seconds using a 3-way syringe. The Dentin Bonding Agent was light-cured with LED equipment (Woodpecker Ltd., intensity 1000 mW/cm2) for 20 seconds. Composite resin (3M ESPE Filtek Z250 XT Nano Hybrid Universal Restorative) was placed onto the dentin discs using a putty impression as a matrix and photopolymerised with LED equipment (Woodpecker Ltd., intensity 1000 mW/cm2) for 20 seconds [Table/Fig-4].
Specimen after restoration and mounted specimen in UTM.
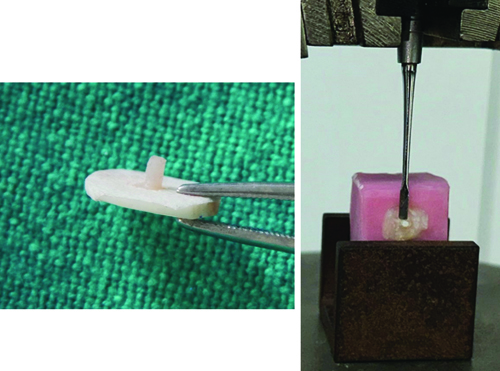
The samples were then embedded in resin blocks and stored in distilled water. Subsequently, the samples were subjected to a MSBS test using a Universal Testing Machine (AE-UTM-LC2 Advanced Equipment, Thane, India). A flat, sharp chisel with dimensions of 6 mm in length and 3 mm in width was placed as close as possible to the resin-dentin interface [Table/Fig-4]. The resin-dentin interfaces of the specimens and the chisel were aligned as straight as possible to ensure shear orientation. A shear force was applied to the specimen at a crosshead speed of 0.5 mm/min until failure occurred. The loads at failure were recorded using the formula [18,21].
Debonding force (N)/Bonding area (mm2): The failed samples were examined to assess the failure patterns under a stereomicroscope at 20x magnification. This examination aimed to determine whether the debonding occurred at the resin-dentin interface, within the adhesive, or within the dentin. The failures were classified as follows: a) adhesive failure between dentin and resin; b) cohesive failure in the resin; c) cohesive failure in the dentin; and d) mixed failure [24].
Statistical Analysis
A one-way ANOVA test (for group-wise comparison) and a Tukey’s HSD test (for pair-wise comparison) were used to analyse the data. The Chi-square test was employed to determine the association between the three groups in the failure mode analysis. The results were considered statistically significant when p≤0.05.
Results
The group-wise comparison of mean and standard deviation of MSBS values is shown in [Table/Fig-5]. As illustrated, the pretreatment of dentin bonding agents with B. hispida resulted in the highest mean MSBS value, followed by the CHX and no pretreatment (control) groups. One-way ANOVA indicated statistically significant differences in bond strength values among the groups (p<0.001).
Group-wise comparison of MSBS bond strength.
| Group | n | Mean (MPa) | Std. Deviation | Sth. Error | 95% CI | Min | Max | p-value |
|---|
| Lower bound | Upper bound |
|---|
| Control (I) | 14 | 6.9724 | 3.15837 | 0.84411 | 5.1488 | 8.7959 | 1.91 | 12.52 | <0.001* |
| CHX (II) | 14 | 14.3848 | 4.23492 | 1.13183 | 11.9396 | 16.8300 | 6.52 | 20.97 |
| B. hispida (III) | 14 | 24.2732 | 5.41329 | 1.44676 | 21.1477 | 27.3988 | 17.67 | 33.35 |
*Statistically significant difference- p<0.05; †One-way ANOVA
Consequently, the Tukey’s HSD test was applied for pair-wise comparisons. The results demonstrated statistically significant differences in the mean bond strength values between the Control and CHX groups, the Control and B. hispida groups, as well as the CHX and B. hispida groups (p <0.001) [Table/Fig-6].
Pair-wise comparison of MSBS bond strength.
| Pair 1 | Pair 2 | Mean difference | Std. error | p-value | 95% Confidence interval |
|---|
| Lower bound | Upper bound |
|---|
| Control | CHX | -7.41243* | 1.65059 | <0.001* | -11.4338 | -3.3911 |
| Control | B. hispida | -17.30086* | 1.65059 | <0.001* | -21.3222 | -13.2795 |
| CHX | B. hispida | -9.88843* | 1.65059 | <0.001* | -13.9098 | -5.8671 |
*Statistically significant difference- p<0.05; †Tukey’s HSD test
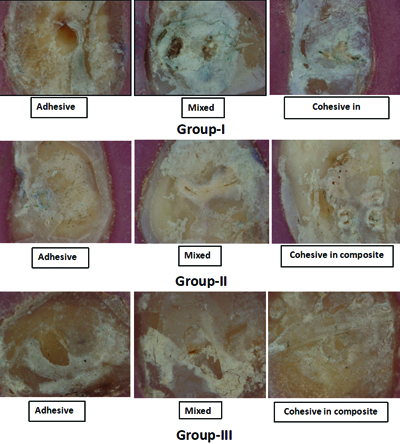
Among the three groups, adhesive failures were more prevalent in Group-I, with 8 cases (57.1%), while the least adhesive failures were observed in Group-III, with only 1 case (7.1%). Cohesive failures were more common in Group-III, totaling 7 cases (50.0%) and were least frequent in Group-I, with three cases (7.1%). Mixed-type failures were more frequent in Group-III, with 6 cases (42.9%) and least frequent in Group-II, with 1 case (21.4%). There was a significant difference in failure modes among the three groups, with a p-value of 0.029 [Table/Fig-7,8].
Stereomicroscope images representing the mode of failure at x20.
Comparison of mode of failure between the groups.
| Failure modes | Groups | Chi-square value | p-value |
|---|
| I (No-pretreatment) | II (CHX-pretreatment) | III (B. hispida pretreatment) |
|---|
| Adhesive | 8 (57.1%) | 7 (50.0%) | 1 (7.1%) | 10.800† | 0.029* |
| Cohesive in composite | 3 (21.4%) | 6 (42.9%) | 7 (50.0%) |
| Mixed | 3 (21.4%) | 1 (7.1%) | 6 (42.9%) |
*Statistically significant difference- p-<0.05; †Chi-square test
Discussion
The results of the present study demonstrated a statistically significant difference in MSBS values among the three groups. Pretreatment with B. hispida resulted in significantly higher MSBS compared to both the pretreatment with CHX and the no pretreatment group.
Three methods for improving dentin bond strength are reported in the literature and were tested in the present study. The first method involved using a functional monomer, such as 10-MDP (Adper Single Bond Universal, 3M ESPE), which enhances chemical and micro-mechanical adhesion by binding with hydroxyapatite in dentin and enamel, forming MDP-Ca salts in the specimens of Group-I. The second method involved the pretreatment of etched dentin with MMP inhibitors, such as CHX, in the specimens of Group-II. The third method consisted of pre-treating etched dentin with B. hispida juice to promote the mineralisation of the hybrid layer, as seen in the specimens of Group-III.
In the present study, Group-I samples were treated with a bonding agent containing 10-MDP, following a conventional protocol without dentin pretreatment. The mean bond strength achieved was 6.9724 MPa, with a standard deviation of 3.158. A similar study achieved a MSBS of 15.60 MPa using self-etch adhesive systems containing HEMA and 10-MDP monomers, but it was conducted with bovine dentin [25]. Another study involving 10-MDP bonding agents (Clearfil SE Bond and Clearfil Tri-S Bond) in self-etch mode reported MSBS bond strength values of 36.9 MPa and 28.5 MPa achieved immediately and after 24 hours, respectively. However, that study also used bovine teeth, which may account for the variation in bond strength [26]. Both studies used dentin from incisors as a bonding substrate, whereas in the present study, dentin from molars was utilised with the etch-and-rinse technique. The formation of water-insoluble MDP-Ca salts enhances bond adhesion, durability and strength, with “nano-layering” of MDP-Ca salts proposed as the mechanism. However, the lengthy carboxyl chain of 10-MDP leads to poor monomer polymerisation and a low elastic modulus at the interface. The presence of HEMA suppresses the formation of nanolayers between 10-MDP and mineralised tissue, resulting in lower mechanical integrity during hybridisation [25].
Analysis of the fracture pattern yielded a majority of adhesive fractures (57.1%), followed by fewer mixed fractures (21.4%) and cohesive composite fractures (21.4%) in Group-I. This finding supports the lowest MSBS bond strength achieved in the present experiment.
Many topical treatments on dentin have been researched, aimed at altering the physical and chemical properties to enhance resin-dentin bonding. Such treatments transform a previously hydrophilic, crystalline and relatively impermeable acid-labile surface into a more hydrophobic, organic, highly permeable and acid-resistant surface. Inhibition of collagenolytic activity using CHX is an important strategy to increase resistance to enzymatic degradation [27].
In Group-II, the mean MSBS achieved was 14.38 MPa, which was significantly higher than that of Group-I, with a p-value of less than 0.001. Analysis of the fracture pattern showed fewer adhesive fractures (50.0%), mixed fractures (7.1%) and cohesive composite fractures (42.9%) in Group-II compared to Group-I. This supports the higher MSBS values achieved in Group-II compared to Group-I in the experiment.
The association between CHX and adhesive systems in the bonding procedure could be a promising strategy to increase the durability of restorations due to the anti-gelatinolytic activity of CHX applied prior to the adhesive systems. According to previous literature, acid-etched dentin treated with CHX prevents MMP activity and decreases collagen solubility [13]. Consequently, the MSBS values of the CHX group were significantly better than those of the control Group-In the present study [28]. Similar findings have been reported in several studies conducted by Carrilho MR et al., Zhang YB et al., Leitune VC et al., and Dionysopoulos D [Table/Fig-9] [29-32].
Comparative studies from the literature [29-32].
| S. No | Author’s name and year | Place of study | Number of subjects | Pretreatment agent | Results | Conclusion |
|---|
| 1. | Carrilho MR et al., 2007 [29] | Brazil | 7 | 2% Chlorhexidine (CHX) | Microtensile Bond strengthCHX group-30 MPaNo pretreatment group-20 MPa9.3% adhesive bond failures in CHX group29.5% bond failures in no pretreatment group | CHX pretreatment improved bond strength |
| 2. | Zhang YB et al., 2010 [30] | Brazil | 40 | 2% Chlorhexidine (CHX) | Microtensile Bond strengthCHX group-23.19 MPaNo pretreatment group-19.10 MPa | CHX pretreatment improved bond strength |
| 3. | Leitune VC, Portella FF et al., 2011. [31] | Brazil | 40 | 2% Chlorhexidine (CHX) | Microshear Bond strength (MSBS)CHX group-24.48 MPaNo pretreatment group-19.93 MPa | CHX pretreatment improved bond strength |
| 4. | Dionysopoulos D et al., 2016 [32] | Greece | Systematic review, 102 studies | 2% Chlorhexidine (CHX) | CHX exhibited better bond strength than the control experimental groupsFurther investigations are required | CHX pretreatment improved bond strength |
| 5. | Present study | India | 42 | 2% Chlorhexidine (CHX)B. hispida | B. hispida exhibited better bond strength than the control and experimental groups | B. hispida pretreatment improved bond strength |
The CHX has been reported to ultimately diffuse out of the polymerised resin network, as it cannot co-polymerise with methacrylate resin monomers. Furthermore, its electrostatic bonding characteristics compromise the long-term anti-MMP effectiveness of CHX, as water acts as a desorption medium [13].
According to Gao X et al., topical mineralisation with calcium/phosphorus (Ca/P) ion release after bonding procedures might not improve adhesive bond strength. The spatiotemporal mismatch of mineralising agents and the hybrid layer prevents mineral deposition in the collagen fibril network. Therefore, dentin collagen mineralisation during hybridisation could be a promising technique for intrafibrillar mineralisation [33]. With all of this in mind, the use of B. hispida was considered, as it has the potential to be a source of minerals in their purest and most natural form.
The mean MSBS of Group-III (24.27 MPa) is significantly higher than that of Group-I and II, with a p-value <0.001*. This increase in bond strength may be attributed to B. hispida being a rich source of minerals, including sodium, potassium, calcium, iron and phosphorus, as well as antioxidants and polysaccharides found in fruit extract. It also contains vitamins such as vitamins C and E, riboflavin and niacin [15].
Analysis of the fracture pattern revealed lower adhesive fractures (7.1%), mixed fractures (42.9%) and cohesive composite fractures (50.0%) in Group-III compared to Group-II. This supports the higher MSBS values achieved in Group-III compared to Group-II in the experiment.
In the literature, the use of B. hispida is reported to improve bone health [16,17]. An animal study indicated the beneficial role of B. hispida in collagen health and bone mineralisation [16,17]. Supplementation with Benincasa Hispida Extract (BHE) in Ovariectomy-Induced Osteoporosis (OVX) mice resulted in the prevention of Bone Mineral Density (BMD) reduction, as well as an increase in mineralisation and collagen health. This condition is often caused by low calcium intake, inactivity and decreased oestrogen output. The bioactive compound 2-furocid present in BHE can be added to food materials to enhance bone health [16,17]. Bones and teeth share common chemistry, including calcium hydroxyapatite crystals.
The presence of 2-furocid acid and minerals such as calcium and phosphorus may have contributed to increased mineralisation of the hybrid layer. The polysaccharides found in the fruit extract exhibit significant antioxidant effects. Additionally, the fruit extract contains vitamins E and C, which further enhance its beneficial effects. The combination of these minerals and antioxidant properties may have led to increased MSBS values [14-17].
Limitation(s)
The optimum concentration of B. hispida must be established. It is necessary to analyse the bioactive compounds of B. hispida and to study the molecular mechanisms of action on human dentin. Future studies will focus on evaluating the release of minerals from B. hispida onto the surface of dentin, the mineralisation of the hybrid layer and the long-term durability of the hybrid layer formed by the application of B. hispida.
Conclusion(s)
The MDP-containing bonding agents with B. hispida pretreatment showed significantly higher MSBS than Group-I and II. MDP-containing bonding agents with CHX pretreatment exhibited significantly higher MSBS compared to Group-I. Minimum adhesive failures were observed in Group-III compared to Group-I and II. Pretreatment with B. hispida may be beneficial for increasing dentin bond strength.
*Statistically significant difference- p<0.05; †One-way ANOVA
*Statistically significant difference- p<0.05; †Tukey’s HSD test
*Statistically significant difference- p-<0.05; †Chi-square test