Psoriasis is a chronic inflammatory skin disorder mediated by type 1 T helper cells and Th17 cells, affecting about 2-3% of the population [1,2]. It is associated with several medical conditions, the most common of which are CV diseases, hypertension, diabetes, and metabolic syndrome [3,4]. The association between psoriasis and CV diseases is only partially understood; however, inflammatory processes and oxidative stress are among the most frequently delineated pathogeneses [5].
Among CV diseases, accumulating evidence highlights the role of inflammation in the pathogenesis of AF, a known cause of increased morbidity and mortality [4,6]. The most common cardiac arrhythmia, AF, is linked to a higher risk of stroke, heart failure, coronary artery disease, and CV mortality [7,8].
Prolongation of PWD is an independent risk factor for the development of AF. PWD has been proposed as an electrocardiographic indicator of inhomogeneous and discontinuous atrial conduction during sinus rhythm in patients with paroxysmal AF [9].
The P wave in an Electrocardiogram (ECG) represents atrial depolarisation, with a normal duration ranging from 40 to 120 milliseconds (ms). PWD is the difference between the maximum and minimum P wave duration on a single 12-lead ECG, with a normal duration of 29±9 ms [10].
A better understanding of the association between psoriasis and AF will enable the early identification of susceptible patients through screening processes. Hence, the present study was conducted to compare the electrocardiographic PWD among individuals with and without psoriasis and to correlate PWD with the severity of the disease.
Materials and Methods
A hospital-based cross-sectional study was conducted in the Department of Dermatology and Venereology at Government Medical College, Trivandrum, Kerala, India, from February 2021 to January 2022. The study received clearance from the Institutional Ethics Committee (HEC No. 02/12/2021/MCT). Participants were provided with an information sheet outlining the details and purpose of the study. The study included 30 patients with psoriasis as the case group and 30 age- and gender-matched subjects without psoriasis, who accompanied other patients (non-psoriasis cases) to the Dermatology Department, as the control group.
Inclusion criteria: All consenting clinically diagnosed patients with psoriasis aged 18 years and older, as well as, all consenting individuals without psoriasis in the same age group, were included in the study as cases and controls, respectively.
Exclusion criteria: Patients with known cases of CV disease, chronic obstructive pulmonary disease, chronic kidney disease, thyroid disorders, or those already on CV medications were excluded from the study. Additionally, when recruiting controls, individuals with pre-existing CV disease and first-degree relatives of psoriasis patients were also excluded.
Sample size: Sample size calculation was done by using a formula: N=(Z1-α/2+Z1-β)2(σ12+σ22)/(μ1-μ2)2
Let ‘N’ represent the sample size. In the case group, the Standard Deviation (SD) of PWD (σ1) was 22.9, and the mean value of PWD (μ1) is 67.4. In the control group, the SD of PWD (σ2) was 19.6, and the mean value of PWD (μ2) was 45.0. The value of (Z1-α/2+Z1-β)2 was 10.49, with a β value of 90% [12]. By substituting these values, we find that N=20. Therefore, 30 individuals were selected from both the case and control groups for the study.
Study Procedure
A detailed history of demography and comorbidities was collected using a structured questionnaire. A general examination was conducted, during which vital signs, height, and weight were recorded, and Body Mass Index (BMI) was calculated. The morphology of lesions, their distribution, nail changes, and joint involvement were documented through a thorough dermatological examination, and the PASI score was calculated [2]. A systemic examination was performed to rule out any associated diseases. A 12-lead ECG was conducted on study participants from both groups in a supine position after 15 minutes of rest, using a BPL ECG machine (Cardiart 6108T single channel). ECG recordings were obtained at a paper speed of 50 mm/s and an amplitude of 20 mm/mV. The beginning of the P wave was defined as the point where the first atrial deflection crossed the isoelectric line, and the end of the P wave was defined as the point where the atrial deflection returned to the isoelectric line [10].
The P wave was assessed, and the maximum and minimum durations of the P wave were recorded in all 12 ECG leads. The difference between the maximum and minimum P wave durations was then calculated (PWD in milliseconds).
Statistical Analysis
The data were entered into Microsoft Excel sheets, and statistical analysis was performed using a trial version of the Statistical Package for the Social Sciences (SPSS) version 20.0. Categorical and quantitative variables were expressed as frequency (percentage) and mean±SD, respectively. The Karl Pearson test was used to find the correlation between the presence of psoriasis with both the severity of the condition and the duration of the disease. A p-value of ≤0.05 was considered statistically significant.
Results
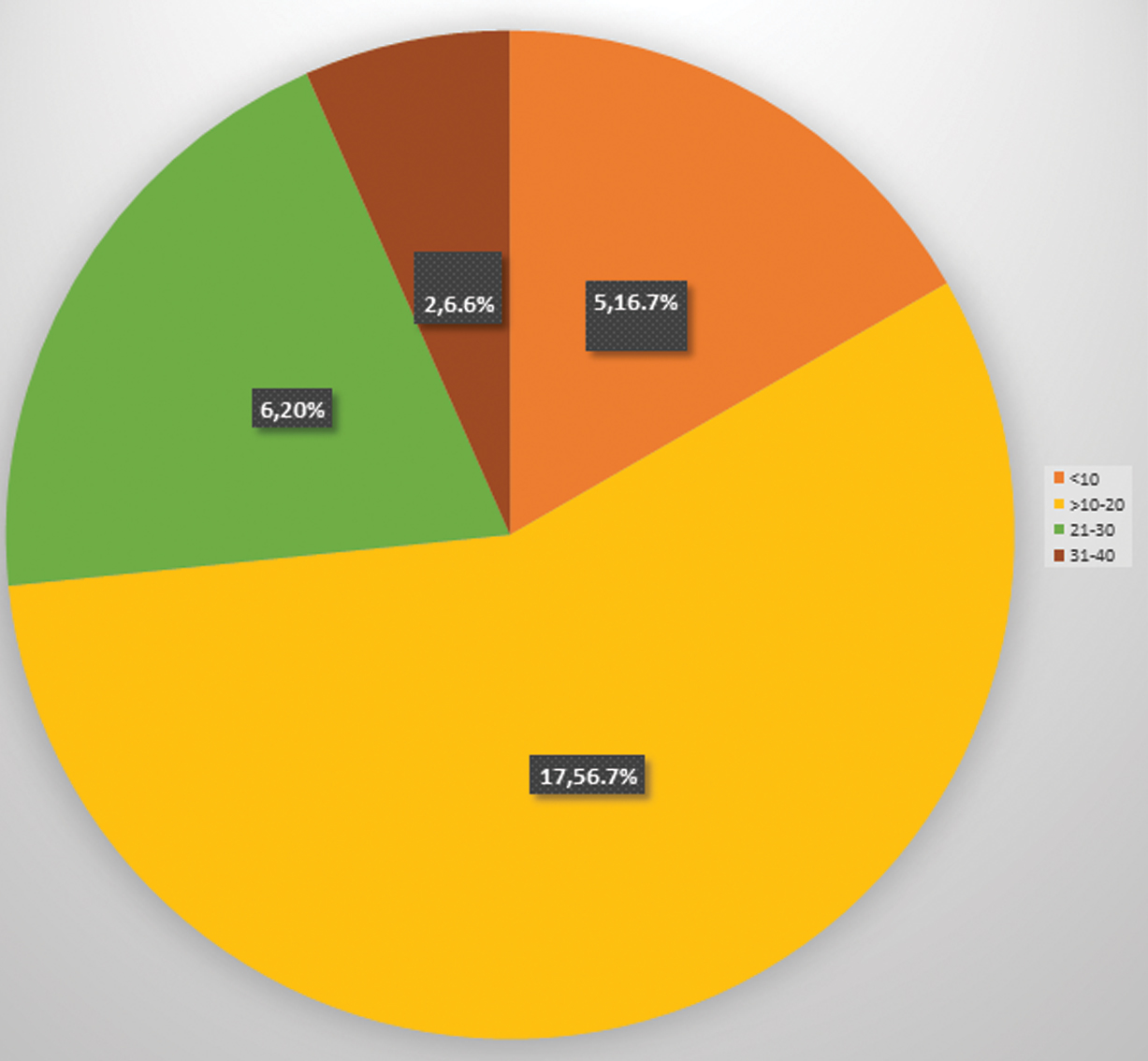
A total of 30 patients with psoriasis who met the inclusion criteria and 30 age- and gender-matched individuals without psoriasis were studied. The age of the patients ranged from 18 to 70 years. Most of the patients (10, 33.3%) were between the ages of 41 and 50, followed by those aged 51 to 60 (8, 26.7%), with a male-to-female ratio of 2.3:1. The mean age of onset was 39.5±11.3 years. Ten patients (33.3%) had their disease onset between the ages of 31 and 40 and between 41 and 50 years [Table/Fig-1]. The mean duration of the disease was 5.07±5.2 years, with a range from six months to 21 years [Table/Fig-2]. The mean PASI score was 16.6±8.6, with scores ranging from 8 to 36. The frequency distribution of the cases according to PASI score is given in [Table/Fig-3].
Age of onset. n: Number; %: Percentage.
| Age of onset (in years) | With psoriasis, n (%) |
|---|
| 18-30 | 6 (20) |
| >30-40 | 10 (33.3) |
| >40-50 | 10 (33.3) |
| >50-60 | 3 (10) |
| >60-70 | 1 (3.3) |
Duration of disease. n: Number; %: Percentage.
| Duration of disease (in years) | With psoriasis, n (%) |
|---|
| <1 | 2 (6.7) |
| 1-5 | 19 (63.3) |
| >5-10 | 5 (16.7) |
| >10 | 4 (13.3) |
Psoriasis Area Severity Index (PASI) score (n, percentage).
A comparison of demographic features is shown in [Table/Fig-4], in which the mean Diastolic Blood Pressure (DBP) of patients with psoriasis was 78.3±4.6 mmHg, while in the group without psoriasis it was 75±5.7 mmHg.
Comparison of demographic findings between psoriatic patients and individuals without psoriasis.
| Characteristics | With psoriasis | Without psoriasis | p-value |
|---|
| Age (mean±SD) | 44.5±10.8 | 44.5±10.8 | 1.000 |
| Gender | 21 males, 9 females | 21 males, 9 females | 1.000 |
| Current smoker | 8 (26.7 %) | 10 (33.3 %) | 0.834 |
| Current alcoholic | 7 (23.3%) | 10 (33.3%) | 0.543 |
| Height (in cm) | 164.8±5.2 | 166.6±6.3 | 0.234 |
| Weight (in kg) | 65.7±6.4 | 66.6±6.9 | 0.628 |
| BMI (kg/m2) | 24.2±1.8 | 23.9±1.8 | 0.473 |
| SBP (mmHg) | 125.1±10.8 | 123.5±10.7 | 0.551 |
| DBP (mmHg) | 78.3±4.6 | 75±5.7 | 0.016 |
| Heart rate (bpm) | 72.6±6.6 | 70.9±7.4 | 0.343 |
SD: Standard deviation; BMI: Body mass index; SBP: Systolic blood pressure in millimeters of mercury; DBP: Diastolic blood pressure in millimeters of mercury; bpm: Beats per minute. A p-value <0.05 is considered significant
The triggering factors for psoriatic patients are presented in [Table/Fig-5]. The majority of the patients (22, 73.3%) had a history of infection, and two patients (6.7%) reported no aggravating factors [Table/Fig-5]. All patients had plaque lesions. Joint involvement was present in five patients (16.7%), and nail changes were observed in 28 patients (93.3%).
Triggering factors in psoriatic patients.
| Triggering factors | Frequency (percentage) |
|---|
| Infection and psychological stress | 11 (36.7%) |
| Infection alone | 11 (36.7%) |
| Psychological stress alone | 6 (20%) |
| History of trauma | 4 (13.3%) |
| No aggravating factors | 2 (6.7%) |
Among the 30 psoriatic patients, PWD was greater than 40 in 22 patients (73.3%), compared to 12 individuals (40%) without psoriasis. The difference in PWD between the groups was found to be statistically significant, with a p-value of less than 0.001 [Table/Fig-6].
Comparison of P Wave Dispersion (PWD), t=3.814. p≤0.001.
| PWD (ms) | With psoriasis | Without psoriasis |
|---|
| n | % | n | % |
|---|
| 20-30 | 4 | 13.3 | 10 | 33.3 |
| 31-40 | 4 | 13.3 | 8 | 26.7 |
| 41-50 | 7 | 23.3 | 10 | 33.3 |
| 51-60 | 4 | 13.3 | 0 | 0.0 |
| 61-70 | 8 | 26.7 | 2 | 6.7 |
| 71-80 | 2 | 6.7 | 0 | 0.0 |
| 81-90 | 1 | 3.3 | 0 | 0.0 |
| Mean±SD | 56.0±16.2 | 42.0±11.1 |
n=Number, %=Percentage, ms: milliseconds, SD: Standard deviation. p-value<0.05 considered as significant
The mean P max was significantly higher in psoriatic patients (108.3±14.16 ms) than in non-psoriatic individuals (98.3±13.4 ms), with a p-value ≤0.001 [Table/Fig-7]. The mean P-minimum was lower in psoriatic patients (52.3±12.8 ms) compared to non-psoriatic individuals (56.3±13.3 ms) [Table/Fig-8]. A statistically significant correlation was observed between the severity of psoriasis and electrocardiographic PWD (r=0.564, p-value ≤0.001). A scatter diagram of electrocardiographic PWD and the PASI is shown in [Table/Fig-9].
Comparison of P wave maximum.
| P max (ms) | With psoriasis | Without psoriasis |
|---|
| n | % | n | % |
|---|
| 61-80 | 3 | 10.0 | 9 | 30.0 |
| 81-100 | 11 | 36.6 | 14 | 46.7 |
| 101 -120 | 14 | 46.7 | 7 | 23.3 |
| 121-140 | 2 | 6.7 | 0 | 0.0 |
| Mean±SD | 108.3±14.16 | 98.3±13.4 |
P max=P wave maximum, t=3.34** p≤0.001. n=Number, %=percentage, ms: milliseconds, SD: standard deviation. p-value <0.05 considered as significant.
Comparison of P wave minimum.
| P min (ms) | With psoriasis | Without psoriasis |
|---|
| n | % | n | % |
|---|
| 20-30 | 2 | 6.7 | 2 | 6.7 |
| 31-40 | 7 | 23.3 | 5 | 16.7 |
| 41-50 | 12 | 40.0 | 7 | 23.3 |
| 51-60 | 0 | 0.0 | 4 | 13.3 |
| 61-70 | 9 | 30.0 | 12 | 40.0 |
| Mean±SD | 52.3±12.8 | 56.3±13.3 |
P min=P wave minimum, t=0.99, p=0.166. n=Number, %=percentage, ms: milliseconds, SD: standard deviation. p-value <0.05 considered as significant.
Scatter diagram for Psoriasis Area Severity Index (PASI) Score (PASI) and Electrocardiographic P wave Dispersion (PWD), r (Karl Pearson’s coefficient of correlation)=0.564**, p≤0.001.
p-value<0.05 considered as significant
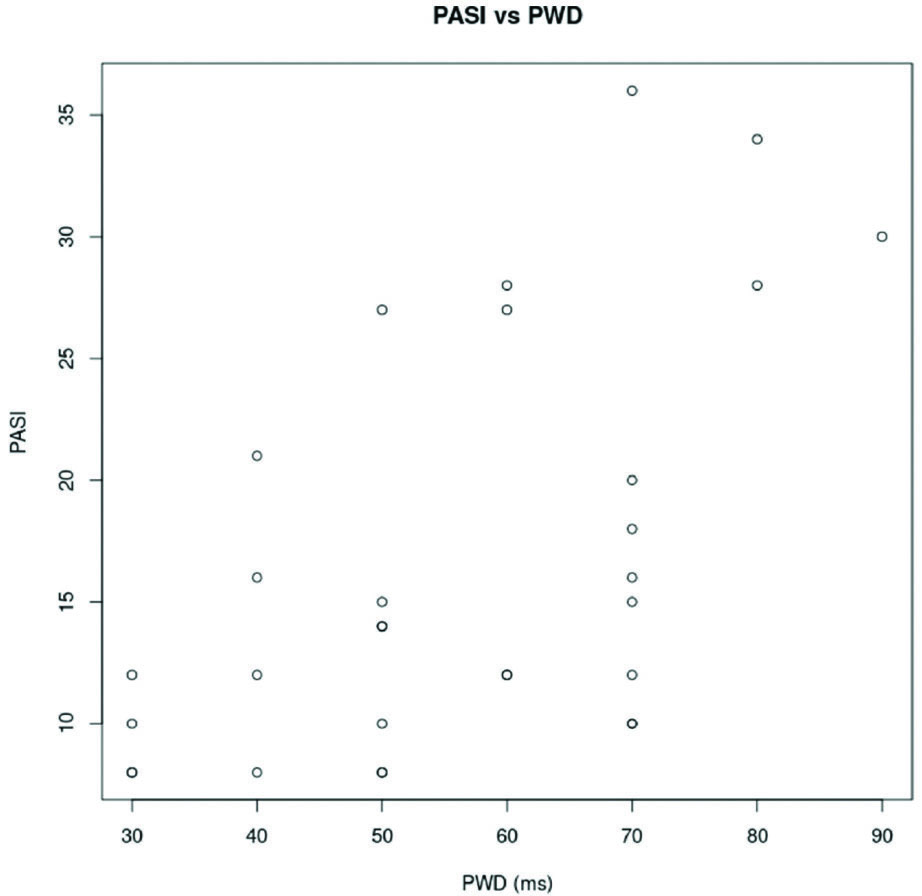
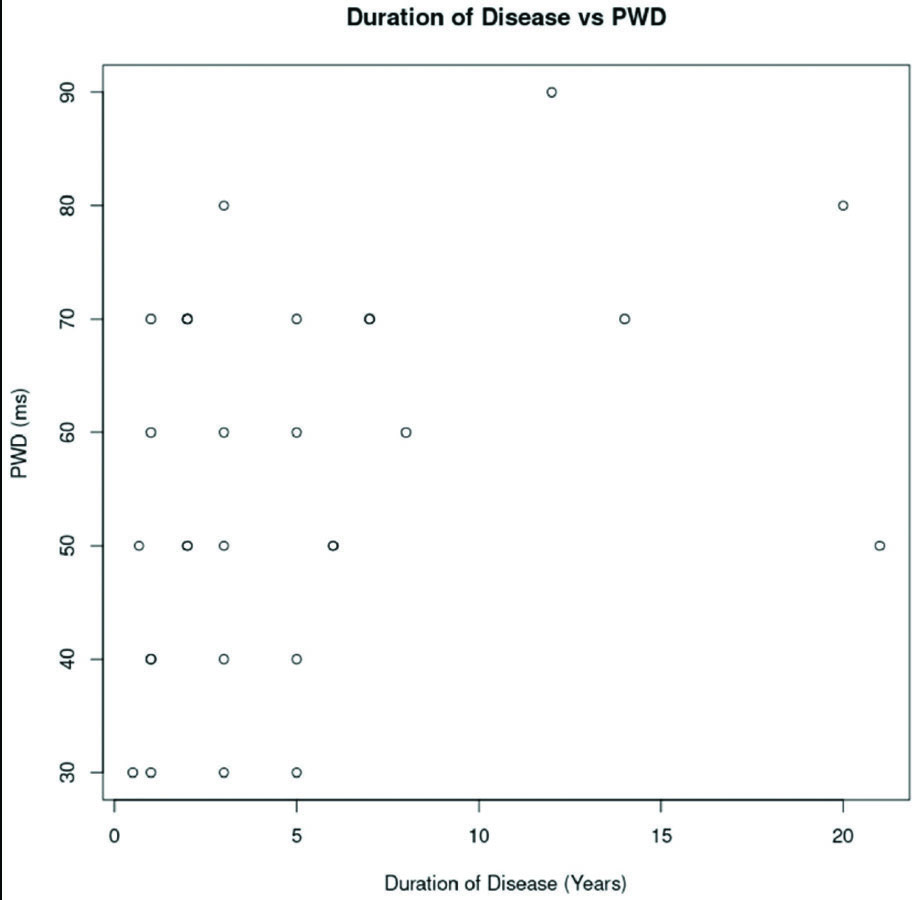
Additionally, [Table/Fig-10] presents the value of Karl Pearson’s coefficient of correlation between PASI and PWD. A statistically significant correlation was also observed between electrocardiographic PWD and the duration of the disease (r=0.372, p-value=0.04). A scatter diagram of electrocardiographic PWD and the duration of the disease is shown in [Table/Fig-11].
Heatmap of Karl Pearson’s coefficient of correlation of PWD, PASI and DoD.
PWD: P wave dispersion; PASI: Psoriasis area severity index score; DoD: Duration of disease

Scatter diagram for Electrocardiographic P wave Dispersion and duration of disease, r (Karl Pearson’s coefficient of correlation)=0.372, p=0.04.
p-value <0.05 considered as significant.
Discussion
The present study included 30 patients with a clinical diagnosis of psoriasis and an equal number of age- and gender-matched individuals without psoriasis. The most common age group was 31-50 years, with a mean age of 44.5±10.8 years for the patients, which was comparable to most other studies on psoriasis [16,17]. This finding was discordant with that observed by Bacaksiz A et al., and Simsek H et al., (33.7±6.7 and 35.8±13 years, respectively) [12,18]. The majority of the patients in this study were men (70%), consistent with most previous studies [12,16-17].
The mean age at onset of the disease was 39.5±11.3 years, with a minimum age of onset of 19 years and a maximum of 62 years. This was discordant with the study by Bacaksiz A et al., (20.1±7.7 years) [12]. The mean duration of the disease in this study was 5.07±5.2 years, which was discordant with the findings of Bacaksiz A et al., (12.8 years) and Markuszeski L et al., (17 years) [12,16]. In a recent publication by Aryanian Z et al., the mean duration recorded was 10±8 years [14]. In the present study, the minimum disease duration was 6 months and the maximum was 21 years. However, in the studies by Bacaksiz A et al., Aryanian Z et al., and Markuszeski L et al., the duration of disease ranged from 3 to 26 years, two months to 40 years, and 1 to 37 years, respectively [12,14,16].
In the present study, 28 (93.3%) patients with psoriasis reported a history of infection and/or psychological distress as factors aggravating their condition. Most of them attributed financial constraints and concerns regarding the chronic nature of psoriasis as the cause of their stress. In a study by Park BS et al., the most common precipitating factor noted was mental stress [19]. The mean PASI score was 16.6±8.6, ranging from 8 to 36. This result was almost concordant with the study by Markuszeski L et al., which reported a mean PASI of 13.4±8.8 [16]. However, it was discordant with the findings of Bacaksiz A et al., where the mean PASI was 3.5±3.7, ranging from 0.4 to 16.8 [12].
The interpretation of the ECG of the participants showed that the mean Heart Rate (HR) was 72.6±6.6 beats per minute in psoriatic patients and 70.9±7.4 beats per minute in participants without psoriasis. This result was consistent with a study from Iran by Aryanian Z et al., [14]. However, it was discordant with the findings of Bacaksiz A et al., which reported a mean HR of 80.5±9.9 beats per minute in patients with psoriasis and 83.1±11.5 beats per minute in individuals without psoriasis [12]. Additionally, a study from Iran found a median HR of 82 beats per minute in the psoriasis group and 84 in the control group [13]. In all these studies, the results were not statistically significant between the groups.
The mean P max was significantly higher in psoriatic patients (108.3±14.16 ms) than in non-psoriatic individuals (98.3±13.4 ms). A higher P max indicates an abnormality in atrial conduction in patients with psoriasis. This finding was similar to that of Bacaksiz A et al., where the mean P max was 112.6±22.7 ms in psoriatic patients and 93.0±12.8 ms in individuals without psoriasis [12]. However, a study from Turkey reported a median P max of 100 ms in the case group and 88 ms in the control group, while Aryanian Z et al., reported 78.67±13.89 ms in cases and 80.06±15.57 ms in controls [13,14]. In all these studies, the results were statistically significant.
The mean P-minimum was lower in psoriatic patients (52.3±12.8 ms) compared to non-psoriatic individuals (56.3±13.3 ms). No statistical association was found between the groups. This finding was similar to that of Bacaksiz A et al., where among 61 cases, the P-min was 42.2±12.5 ms in psoriatic patients and 47.4±14.3 ms in controls, with results that were not statistically significant [12]. However, in the study by Aryanian Z et al., a statistical difference between groups was noted (38.22±6.86 ms among cases and 50.67±10.94 ms in controls) [14].
PWD was found to be prolonged in psoriatic patients, and this difference was statistically significant with a p-value ≤0.001, indicating an increased risk of developing AF in patients with psoriasis compared to individuals without psoriasis. The mean PWD was 56±16.2 ms in psoriatic patients and 42±11.1 ms in non-psoriatic individuals, respectively. Studies by Bacaksiz A et al., Namazi N et al., and Aryanian Z et al., have reported similar findings [12-14].
A statistically significant correlation was observed between the severity of psoriasis and PWD (p-value ≤0.001). As the severity of psoriasis increases, PWD also increases, leading to a higher chance of developing AF later in life. Comparable findings were reported in a case-control study by Bacaksiz A et al., and in a recent observational study by Kumar U et al., [12,15]. In contrast, a study from Iran by Namazi N et al., reported no association between the severity of psoriasis and PWD [13].
In the study, a significant correlation was also observed between the duration of the disease and PWD, with a p-value of 0.04. This indicates that the longer the duration of psoriasis, the greater the PWD, and the higher the chance of developing AF. Therefore, an earlier onset of the disease correlates with a higher PWD and an increased risk of developing AF later in life. However, studies conducted by Namazi N et al., and Simsek H et al., observed no correlation between the duration of psoriasis and the incidence of arrhythmia [13,18].
Limitation(s)
The major limitation of this study was its cross-sectional design. Data were collected at a single point in time, with no follow-ups; therefore, trends that may recur over time could not be studied.
Conclusion(s)
This study showed that patients with psoriasis vulgaris had higher PWD, indicating an increased risk of AF compared to those without psoriasis. Additionally, the study revealed a significant correlation between PWD and both the severity and duration of the disease. Therefore, ECG, which is a reliable, non-invasive, and feasible method, should be considered as part of the screening process for AF, particularly in patients with severe and long-standing psoriasis. Prospective studies will be needed to confirm the development of AF in patients with psoriasis.
SD: Standard deviation; BMI: Body mass index; SBP: Systolic blood pressure in millimeters of mercury; DBP: Diastolic blood pressure in millimeters of mercury; bpm: Beats per minute. A p-value <0.05 is considered significant
n=Number, %=Percentage, ms: milliseconds, SD: Standard deviation. p-value<0.05 considered as significant
P max=P wave maximum, t=3.34** p≤0.001. n=Number, %=percentage, ms: milliseconds, SD: standard deviation. p-value <0.05 considered as significant.
P min=P wave minimum, t=0.99, p=0.166. n=Number, %=percentage, ms: milliseconds, SD: standard deviation. p-value <0.05 considered as significant.