The IC process addresses the autonomy principle of ethics by providing patients with information, enabling them to determine their preferences [1,2]. Informed consent for a surgical procedure is a process wherein a treating doctor interacts with the patient before the procedure, empowering them to make an informed choice regarding their treatment [3]. An informed consent form for surgery is a contract form given to the patient before surgery which should incorporate details about the nature of the disease, the planned intervention, the benefits and risks associated with the intervention, and any alternatives to the proposed intervention [4].
The responsibility of explaining the IC form and its contents to the patient lies with the treating surgeon’s team. After reading the IC form and discussing any concerns with the surgeon, the patient is required to complete and sign the form if they decide to proceed with the procedure. An effective IC form is a crucial patient safety measure [4]. However, merely having a patient sign an IC form does not ensure they understand its contents. It is the provider’s obligation to ensure that the patient is taking an interest in this dynamic process and then signing the form. Thus, written IC necessitates effective communication between the doctor and the patient [5].
Indian and international studies evaluating the IC process for surgeries have generally found it to be unsatisfactory in most cases [6,7]. Research by Patil A et al., in India, Ede O et al., in Nigeria, and Shafique MU et al., in Pakistan observed that crucial components, like alternative options and procedure risks, were often inadequately communicated to patients [8-10]. Similarly, a study by Oh KE et al., in Ireland highlighted the frequent use of medical acronyms in general surgery consent forms, which can be confusing for patients [11]. In India, the doctor-patient relationship is primarily governed by trust, with doctors often seen as authoritative persons [12]. Consequently, the benefits of IC does not always reach all patients in routine medical practice. A study by Singh AD et al., in Northern India found that written IC was obtained in 92% of surgical cases [7]. Other challenges include language barriers, poor patient literacy, and instances where the healthcare team may neglect the IC process, especially if the patient comes from a lower socio-economic background [13-15]. Additionally, in some hospitals, the IC form is provided to the patient just before surgery, and they are required to sign it as a mere formality, often without fully understanding or reading it [16].
As noted above, there are gaps in the implementation of the surgical IC process, and these are often overlooked. It is imperative to identify these gaps in different hospital settings and apply rectification measures to enhance patient care and satisfaction while reducing legal litigations. Given the limited number of original studies from India that have examined these issues, this study aimed to assess the current implementation levels of the IC process during surgical procedures in a tertiary care teaching hospital in Dakshina Kannada District of Karnataka, Southern India. The findings will provide valuable insights into these implementation challenges, serving as a foundation for developing effective remedial strategies.
The objectives of the study were: (i) to estimate the proportion of patients/surrogates who read, understood, and then signed the IC form before undergoing surgical procedures; (ii) to identify the different healthcare team members involved in explaining the IC form to patients/surrogates and to determine the proportions of these members; (iii) to evaluate the extent to which different components of the IC form (procedure details, risks, benefits, and alternative options) were explained to patients/surrogates; and (iv) to determine the influence of IC form on surgical procedure decision-making and the overall satisfaction with the IC process.
Materials and Methods
This cross-sectional study was conducted at a tertiary care teaching hospital in the Dakshina Kannada district of Karnataka, Southern India, from April 2020 to March 2021. The study population comprised patients admitted to the postsurgical wards of general surgery, orthopaedics, obstetrics and gynaecology, otorhinolaryngology, and ophthalmology. Permission to conduct the study was obtained from the Dean of the institution, and ethical clearance (KVGMCIEC202049 dated 04.06.2020) was granted by the Institutional Ethics Committee.
Inclusion criteria: Patients aged 18 years and older who were admitted to the postsurgical wards were included in the study.
Exclusion criteria: Patients who were seriously ill postsurgery and required intensive care were excluded from the study.
Sample size estimation: The sample size was determined based on a previous study that reported 65.6% of participants received oral information on IC and were satisfied with the process [5]. Using the formula n=4pq/L2, where p=65.6, q=34.4 and L=15% of p (relative precision), the sample size was calculated to be 93, which was rounded up to 100. Using continuous enumeration, all adult patients admitted to the postsurgical wards from July 1, 2020, onwards were invited to participate until the sample size was reached.
Study Procedure
A questionnaire was developed by the investigators and validated by three subject experts in the fields of surgery, ethics, and public health. It was divided into four parts: socio-demographic variables, administration of the IC form, details about the person explaining the IC form along with its content, and the influence of the IC form on decision-making, as well as overall satisfaction with the IC process. The questionnaire was pilot-tested among five patients in the postoperative wards in June 2020, and the feedback received was incorporated into the final version used for data collection. Data collection was conducted by the primary investigator between the third and seventh days after surgery. The study was explained in detail to all eligible patients in the postoperative wards of the general surgery, orthopaedics, obstetrics and gynaecology, otorhinolaryngology, and ophthalmology departments, and they were provided with a participant information sheet. Written and signed IC was obtained from all willing participants, and interviews were conducted in a manner that ensured their privacy. The collected data were securely stored in a locked cabinet and on a password-protected laptop.
Statistical Analysis
The data were entered into Microsoft Office Excel (version 2019, Microsoft Corporation, Washington, USA), and analysis was done using IBM SPSS (version 27, IBM Corporation, New York, USA). Descriptive analysis was performed, presenting categorical data as frequencies and proportions, and continuous data as means and standard deviations.
Results
A total of 100 patients participated in the study. A large proportion of the patients (29%) were in the age group of 41 to 50 years, and the majority were females (62%) [Table/Fig-1]. The majority of the patients were married (84%), and all patients were literate, able to read or write in at least one language, even if they lacked formal education.
Baseline characteristics of the study population (N=100).
| Variables | No. of patients |
|---|
| Age (years) |
| 18-30 | 22 |
| 31-40 | 17 |
| 41-50 | 29 |
| 51-60 | 08 |
| 61-70 | 18 |
| >70 | 06 |
| Gender |
| Male | 38 |
| Female | 62 |
| Marital status |
| Married | 84 |
| Unmarried | 16 |
| Highest education |
| Non-formal education | 21 |
| Primary school (1-4) | 23 |
| Middle school (5-7) | 08 |
| High school (8-10) | 19 |
| PUC (11-12) | 22 |
| Degree/Graduate | 07 |
| Surgical department |
| Obstetrics and Gynaecology | 37 |
| Orthopaedics | 34 |
| General surgery | 20 |
| Ophthalmology | 06 |
| Otorhinolaryngology | 03 |
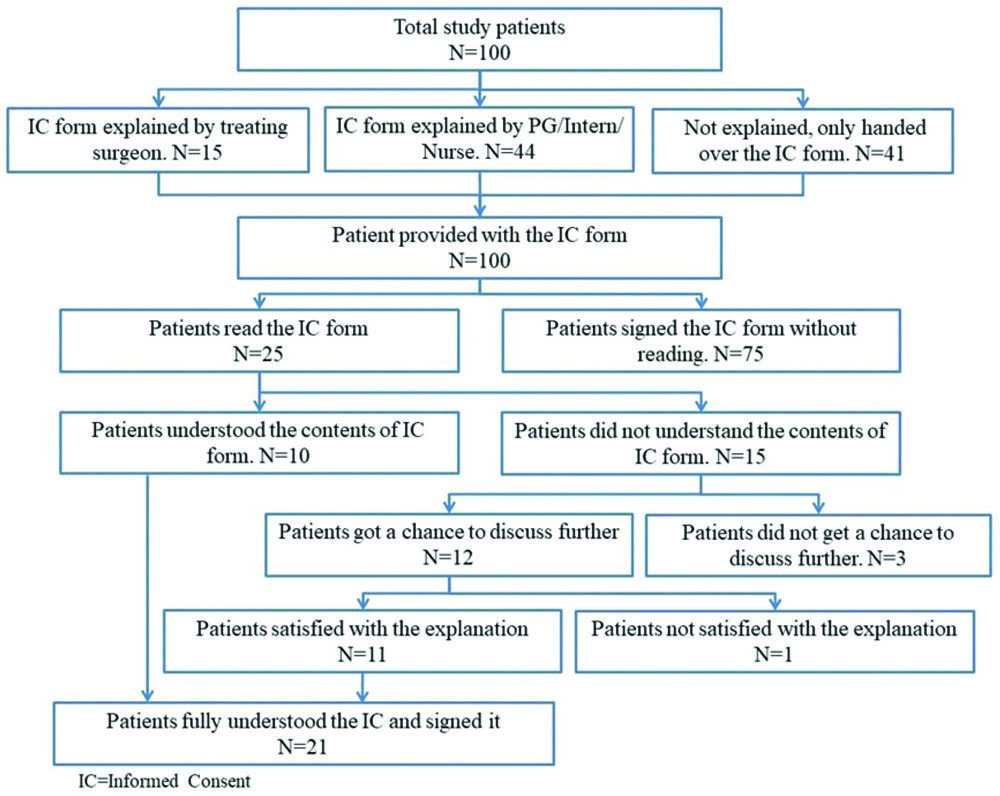
All patients were provided with the IC form before the surgical procedure. However, only 25 patients read the form completely, and just 10 of them fully understood its contents. Fifteen patients expressed doubts regarding the contents of the form, particularly concerning the adverse events secondary to the treatment. Among these, 12 individuals had the opportunity to discuss their doubts and felt comfortable asking for explanations from healthcare providers, with 11 reporting that their questions were satisfactorily answered. Overall, only 21 out of 100 patients fully understood the IC form and signed it [Table/Fig-2].
Flowchart showing the explanation and understanding of the Informed Consent (IC) form.
The IC form was primarily handed over to patients or their surrogates by nurses (61%), followed by postgraduate students (21%), interns (10%), and operating surgeons (8%). A total of 59 out of 100 patients received an explanation of the IC form from healthcare team members. Most explanations were provided by postgraduate students, followed by the operating surgeon [Table/Fig-3]. However, 41 patients did not explained about the IC form. Among those who received an explanation, 41 (69.5%) comprehended the oral information completely, while 16 (27.1%) had a partial understanding, and 2 (3.4%) claimed they did not understand even after the explanation. In 94% of instances, both the patient and a relative or surrogate signed the IC form, while in 6%, only the surrogate signed because the patient was unable to do so.
Distribution of personnel explaining the IC form to patients (N=100).
| Person who explained the procedure | No. of patients |
|---|
| Treating surgeon | 15 |
| Postgraduate | 35 |
| Staff nurse | 05 |
| Intern | 04 |
| No explanation provided | 41 |
In terms of informing patients about various components of the IC form, either at the time of providing the IC form or during prior consultations, it was noted that information on the surgical procedure, such as the procedure to be carried out and the chance of success, of the surgical procedure, was provided to the majority of the patients [Table/Fig-4]. However, only 53% of patients were informed about the risks, and a mere 7% were apprised of potential alternatives to the proposed procedure.
Different components of the IC form explained to the patients at the time of providing the IC form or during prior consultations (N=100).
| IC form component on which information was provided to patients | No. of patients |
|---|
| Surgical procedure |
| Type of surgical procedure | 98 |
| Type of incision | 35 |
| Type of anaesthesia | 41 |
| Prognosis | 75 |
| Outcome of not receiving treatment | 20 |
| Chance of success of the surgical procedure | 68 |
| Postoperative progress | 30 |
| Risks |
| Potential complications/adverse events | 53 |
| Benefits |
| Benefits of the procedure | 76 |
| Alternative options |
| Any other alternative to the proposed procedure | 07 |
The IC form had a minor influence on surgical decision-making for 61% of patients [Table/Fig-5]. Oral information had a higher influence on surgical decisions compared to written information. The study found that 11% of patients felt more anxious after receiving the information. Nearly two-thirds of patients preferred more information related to the IC form. Overall, 43% of patients expressed satisfaction with the IC process.
Influence of IC form on surgical procedure decision-making and overall IC process satisfaction (N=100).
| Variable | No. of patients |
|---|
| Influence of IC form on surgical decision |
| Minor influence | 61 |
| Did not influence | 39 |
| Type of information of IC form that influenced surgical decision |
| Oral information | 42 |
| Written information | 12 |
| Both oral and written information | 07 |
| Did not influence | 39 |
| Consequence of receiving the IC form information |
| Relieved after obtaining the information | 37 |
| Nothing changed | 52 |
| Became more anxious | 11 |
| Preference for IC form related information |
| Prefer more information | 68 |
| Information was sufficient | 21 |
| Prefer less information | 11 |
| Overall satisfaction with the IC process |
| Satisfactory | 43 |
| Not satisfactory | 57 |
Discussion
It is essential and ethical to provide complete information to patients before any surgical procedure. This study examined the process of written IC for surgical procedures in a tertiary care teaching hospital in the Dakshina Kannada District of Southern India. A total of 100 patients participated in the study. The age distribution revealed a relatively higher proportion of senior citizens (≥60 years) at 24%, compared to the general population of India, where senior citizens account for 10.1% [17]. This is plausible, as the prevalence of many diseases, especially non communicable diseases, is higher among senior citizens. About two-thirds of the study participants were female; this pattern was seen as 37% of the study patients were from the Obstetrics and Gynaecology department.
In the present study, it was found that although all the patients received and signed the IC form, only a quarter of them read it adequately. These findings contrast with those of a study done by Agozzino E et al., in Italy, where all patients received the IC form and signed it, but 51.8% read it adequately [5]. In another study by Ede O et al., conducted in Nigeria, it was observed that 39.2% of the patients did not read the information on the consent form before signing it [9].
The lack of attention given to the IC form may be attributed to patients’ limited interest in the document. They appeared to rely more on the oral communication provided by the surgeon rather than on the written information presented to them [18]. Another reason might be the perception that they would not comprehend the form, as it might be written in technical language. A study by Mertz K et al., on patients who underwent hand surgery assessed the reading levels of IC forms and found that 78% and 58% of the forms were written above the sixth and eighth-grade reading levels, respectively, and the readability was considered poor [19]. It is generally recommended that IC forms be written at an eighth-grade reading level and in a language that the patient understands to improve comprehension [20].
When a patient is advised to undergo a surgical procedure, they often have many questions related to it. In a developing country like India, especially among poorer patients, there is a heavy reliance on the treating healthcare team to explain everything related to the procedure, as they usually do not have any other reliable source to clear their doubts. The primary responsibility of explaining the procedure, clearing the doubts and obtaining IC is of the treating surgeon [21].
In the present study, it was observed that the operating surgeons themselves explained and obtained the IC form in only 15% of the cases. In 44% of cases, it was the postgraduate student, nurse, or medical intern who explained the IC form, and unfortunately, in 41% of cases, the IC form was not explained to the patients at all. This reflects a casual attitude among some surgeons towards the IC form. According to Paterick TJ et al., the doctor engaged in treating should directly conduct the discussion with the patient and their attendees [3]. Anderson OA and Wearne IMJ, in an article on best practices in IC, believe that any person obtaining IC must either be capable of performing the procedure himself or should have specialised training in advising patients about the procedure [22]. Interns usually do not fulfill either of these criteria. The postgraduate student or trained nurse can explain the IC form to the patients under the supervision of the treating surgeon. Ultimately, it is the treating surgeon who is accountable for explaining and obtaining the IC form.
When explaining the IC form to patients, the discussion must include information about the treatment, its risks and benefits, and alternative therapies along with their associated risks and benefits [23]. Thus, when discussing the IC form, it is equally important to explain all its components to the patients. In the present study, while information on the surgical procedure and its benefits was given to a large majority of the patients, risks and alternative options to the procedure were not satisfactorily discussed.
The findings mentioned above were similar to a study conducted by McGaughey I on knee arthroscopic procedures, in which patients stated that surgeons most often explained the diagnosis and the type of procedure to be performed. However, information about other aspects of treatment, like postoperative course or possible complications, was seldom explained [24]. In the study by Shafique MU et al., it was found that complications of surgical procedures and alternative treatment options were informed to 24% and 44% of patients, respectively [10]. Additionally, another study by Singh AD et al., noted that alternative options were discussed with only one-third of the patients [7]. The complete risk profile of the procedure may not be explained by the surgeon due to concerns that it could unnecessarily heighten patient anxiety [18]. Alternate options to the procedure was the least discussed, which could be the result of the paternalistic attitude among some doctors who feel they can decide things on patients’ behalf. Other reasons could be the perceived incapability of patients to make informed decisions and the time constraints faced by doctors.
When the IC form is effectively communicated to patients, it becomes a mutually beneficial arrangement for both the patient and the physician. Well-informed patients are more likely to be satisfied and less inclined to pursue legal action [25]. Conversely, patients who are not adequately informed about the risks of a procedure often express regret following surgery [26-28]. Thus, all patients should be meticulously explained about the IC form, covering all its components, preferably by the treating surgeon.
The influence of the IC form on surgical procedure decision-making was found to be minimal. Similarly, a study by Patil A et al., in a Mumbai hospital reported a minor influence of the IC on surgical decisions [8]. This minimal influence may be attributed to the IC form not being provided or explained adequately in advance. Patients likely decided to undergo surgery before receiving the IC form, and in most cases, they signed it without thoroughly reading it, further contributing to its negligible influence on decision-making.
A noteworthy observation was that about one in ten patients became more anxious after receiving information from the IC form. This could be due to two potential reasons. First, there is the nocebo effect, where providing detailed information about side-effects and complications might cause patients to worry that they will experience these negative outcomes [29,30]. Second, many patients’ doubts were not adequately addressed, as evidenced by two-thirds of participants expressing a preference for more information. Improved communication between doctors and patients, along with opportunities for patients to ask questions, could help alleviate much of this anxiety.
When assessing overall satisfaction with the IC process, only 43% of patients reported it as satisfactory. In contrast, a study by Singh AD et al., in Punjab found that 87.8% of patients expressed satisfaction with the IC process [7]. This difference may be attributed to better explanations and a clearer understanding of the IC form by patients in the Punjab study. The strength of the present study lies in its valuable insights within this crucial research area, particularly amidst the scarcity of original research from India addressing gaps in IC form implementation.
Limitation(s)
The study had a few limitations, including potential bias in patient responses due to their ongoing care under the treating surgeon during data collection. There is a possibility that patients might have provided favourable responses out of concern that if the treating surgeon were to learn of their unfavourable responses, it could adversely affect their treatment. To mitigate this bias, the authors took measures such as explaining the study to patients, ensuring privacy during data collection, and maintaining data confidentiality.
Another limitation of the study was that patient comprehension of the IC form relied on subjective self-reported understanding. The study also had a higher proportion of female participants due to the large number of patients from the Obstetrics and Gynaecology department.
Moreover, data for three questions could not be included in the analysis. Two questions pertained to the timing of the IC form and further explanation, but it was determined that an additional question regarding whether the surgical procedure was elective or emergency was necessary for meaningful analysis. Since this additional data was not collected, these questions were not analysed. Another question addressed postsurgical instructions, which, upon further review, was found to be outside the scope of present study focused on the IC process. Consequently, this data was excluded from the analysis.
Conclusion(s)
The implementation of the IC form has been noted to be unsatisfactory, potentially denying patients their right to make informed choices. The treating surgeon must provide and explain the IC form in detail well in advance, ensuring that the patient fully understands the procedure, including its risks and alternatives, and has the opportunity to address any doubts. There is a pressing need for ongoing education programs for doctors that include patient ethics. Surgeons must reevaluate their attitudes toward the IC process, recognising it not only as a legal requirement but also as an opportunity to empower patients to make informed decisions. Additionally, it is crucial for Hospital Ethics Committees to ensure strict adherence to IC guidelines.