The need for this study arises because autopsy is a crucial tool for evaluating pathologies that cannot be assessed in living individuals. The collated morphometric data can help demonstrate the percentage of atherosclerotic narrowing of the coronaries, especially in a young, non diseased population. This information can be beneficial for community awareness, leading to corrective and preventive measures to halt further development of atherosclerotic changes in young adults [4].
The objective of the study was to evaluate the thickness of the walls of the coronary arteries at autopsy using morphometric parameters.
Materials and Methods
This was a retrospective cross-sectional autopsy study conducted at the Department of Pathology, in collaboration with the Department of Forensic Medicine, Sri Devaraj Urs Medical College, Kolar, Karnataka, India from January 2020 to December 2020. Ethical clearance was obtained from the Institutional Ethical Committee (IEC) before the start of the study, with IEC No. DMC/KLR/IEC/540/2020-21.
Inclusion criteria: Cases autopsied for deaths that occurred during the study period due to unnatural causes, such as accidents and suicides were included in the study.
Exclusion criteria: Cases with a past history of ischaemic heart disease were excluded from the study.
Sample size: The sample size was calculated based on the formula:

d=absolute precision 0.03, α/2=desired confidence interval 95%, p=expected proportion=0.4, Z2=level of confidence according to the standard normal distribution (for a level of confidence of 95%, Z=1.96).
p=estimated proportion of the population that presents the characteristic (when unknown p=0.5). d=tolerated margin of error (the real proportion within 10.74%). Utilising the above values, sample size was estimated n=(z)2/d2.
To calculate with a 95% level of confidence and a margin of error of 10.74%, Sample size was estimated to be around 80.
Study Procedure
The cases were collected from the files of the Department of Pathology. The case details were further captured from the files of the Department of Forensic Medicine and entered into a proforma.
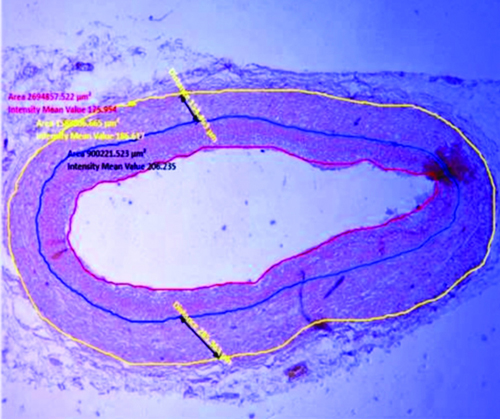
The slides and blocks of each case representing coronary arteries were retrieved from the archives of the pathology department. The tissue sections, stained with haematoxylin and eosin, were screened by two pathologists and classified into atherosclerotic and non atherosclerotic groups. The non atherosclerotic group consisted of types I and II from the modified American Heart Association (AHA) classification for atherosclerosis, while types III to VI were considered part of the atherosclerotic group [5]. For each case, tissue sections from the left anterior descending artery, left circumflex artery, and right coronary artery were screened. Fresh tissue sections were then taken from each paraffin block and stained with VVG stain to properly demarcate the internal elastic lamina, external elastic lamina, and to evaluate other histomorphological features required for morphometric analysis. In non atherosclerotic cases, one of the three arteries was selected for special staining. In cases with atherosclerotic lesions, the artery with the highest grade of lesion among the three was chosen for staining with VVG stain [Table/Fig-1,2].
Non atherosclerotic coronary artery showing internal and external elastic lamina with markings made for morphometric parameter measurements (Verhoeff-Van-Gieson (VVG) stain X400).
Atherosclerotic coronary artery showing internal and external elastic lamina with markings made for morphometric parameter measurements {Verhoeff-Van-Gieson (VVG) stain X400}.
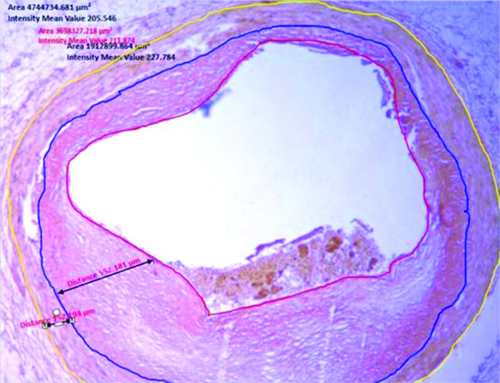
For the estimation of morphometric measurements, microscopic images of the VVG-stained tissue section slides were captured using a Zeiss microscope attached to a camera, and morphometric measurements were performed using ZEN software. The parameters measured included LA, IELA, EELA, width of the intima at maximal thickness, and width of the media at maximal thickness, as per AHA grading [Table/Fig-1,2] [5]. IELA was defined as the area surrounded by the internal elastic lamina, while EELA was defined as the area surrounded by the external elastic lamina. To calculate the intimal area, IELA was subtracted from the LA, and to calculate the medial area, EELA was subtracted from the IELA.
To estimate the severity of atherosclerosis in the coronary arteries, the following three calculations were performed. First, to calculate the percentage of luminal narrowing, the intimal area was divided by the IELA and multiplied by 100. Second, to calculate the Intimal Thickness Index (ITI), the intimal area was divided by the medial area. Third, to calculate the IMR, the width of the intima at maximal thickness was divided by the width of the media at maximal thickness [5,6].
Statistical Analysis
All the data were entered into a Microsoft Excel spreadsheet and analysed using SPSS version 22.0 (IBM SPSS Statistics, Somers, NY, USA). Categorical data were represented in the form of frequencies and proportions, while continuous data were represented as means and standard deviations. An Independent t-test was used as the test of significance to identify the mean difference between two quantitative variables. A p-value of <0.05 was considered statistically significant, assuming all the rules of statistical tests were followed.
Results
A total of 80 autopsy cases were considered for the study, of which 62 (77.5%) were males and 18 (22.5%) were females. The mean age of the cases was 37.6 years, with the maximum number of cases occurring in the age group of 30 to 39 years [Table/Fig-3]. Among the 80 cases, the causes of death were as follows: 52.5% (n=42) due to road traffic accidents, 13.75% (n=11) due to poisoning, 7.5% (n=6) due to homicide, 6.25% (n=5) due to hanging, 5% (n=4) due to electrocution, 2.5% (n=2) due to drowning, and 12.5% (n=10) due to snake bites.
Distribution of cases according to age and sex in the present study.
| Variables | n (%) |
|---|
| Sex |
| Male | 62 (77.5) |
| Female | 18 (22.5) |
| Age group (years) |
| 10-19 | 7 (8.8) |
| 20-29 | 14 (17.5) |
| 30-39 | 34 (42.5) |
| 40-49 | 13 (16.3) |
| 50-59 | 7 (8.3) |
| 60-69 | 4 (5) |
| 70-79 | 1 (1.3) |
Of the total 80 cases, 11 cases (13.8%) had atherosclerotic lesions in the coronaries. Among the 18 female cases, two cases (11.1%) had atherosclerotic lesions in the coronaries and were asymptomatic. Among the 62 male cases, nine cases (14.5%) had atherosclerotic lesions in the coronaries and were asymptomatic [Table/Fig-4]. [Table/Fig-5] shows the age distribution among non atherosclerotic and asymptomatic atherosclerotic cases, where the percentage of asymptomatic atherosclerotic cases increased progressively with advancing age.
Distribution of subjects according to sex into atherosclerotic and non atherosclerotic groups.
| Sex | Non atherosclerotic cases, n (%) | Atherosclerotic cases, n (%) | Total n (%) |
|---|
| Female | 16 (88.8) | 2 (11.1) | 18 (100) |
| Male | 53 (85.5) | 9 (14.5) | 62 (100) |
| Total | 69 (86.2) | 11 (13.8) | 80 (100) |
Distribution of subjects according to age in non atherosclerotic and atherosclerotic group.
| Age (years) | Non atherosclerotic casesn (%) | Atherosclerotic casesn (%) | Totaln (%) |
|---|
| 16-30 | 23 (92) | 2 (8) | 25 (100) |
| 31-45 | 29 (90.6) | 3 (9.4) | 32 (100) |
| 46-60 | 15 (78.9) | 4 (21.1) | 19 (100) |
| >61+ | 2 (50) | 2 (50) | 4 (100) |
| Total | 69 (86.2) | 11 (13.8) | 80 (100) |
All morphometric parameters were increased in the asymptomatic atherosclerotic group compared to the non atherosclerotic group, except for the LA and the width of the media at maximal intimal thickness, which were decreased in the asymptomatic atherosclerotic group. However, the p-values for various morphometric parameters between the two groups were not statistically significant, except for the width of the intima at maximal intimal thickness and the IMR, which had p-values of 0.005 and 0.027, respectively, indicating statistical significance [Table/Fig-6]. The arteries with the maximum lumen narrowing in the non atherosclerotic group were observed in the left anterior descending artery, followed by the left circumflex artery and then the right coronary artery.
Morphometric parameters among non atherosclerotic and atherosclerotic groups depicting mean, standard deviation with p-value.
| Morphometric parameters | Group | Mean±SD | p-value* |
|---|
| Luminal Area (LA) (mm2) | Non atherosclerosis | 2.17±4.29 | 0.785 |
| Atherosclerosis | 1.80±2.12 |
| Internal Elastic Lamina Area (IELA) (mm2) | Non atherosclerosis | 2.92±4.22 | 0.154 |
| Atherosclerosis | 4.91±4.42 |
| External Elastic Lamina Area (EELA) (mm2) | Non atherosclerosis | 4.83±8.76 | 0.547 |
| Atherosclerosis | 6.50±6.19 |
| Width of intima at maximal intimal thickness (mm2) | Non atherosclerosis | 0.000213±0.000150 | 0.005 |
| Atherosclerosis | 0.000585±0.000343 |
| Width of media at maximal intimal thickness (mm2) | Non atherosclerosis | 71.846±80.031 | 0.496 |
| Atherosclerosis | 51.754±89.64 |
| Percentage of luminal narrowing (%) | Non atherosclerosis | 46.7±0.211 | 0.168 |
| Atherosclerosis | 56±0.158 |
| Intima to Media Ratio (IMR) | Non atherosclerosis | 1.031±0.442 | 0.027 |
| Atherosclerosis | 2.432±1.784 |
| Intimal Thickness Index (ITI) | Non atherosclerosis | 1.3118±2.338 | 0.362 |
| Atherosclerosis | 1.97±0.955 |
*Independent t-test
Discussion
Atherosclerosis of the coronary arteries is the most common cardiac pathology observed at autopsies [7,8]. Atherosclerosis is defined as an inflammatory, fibroproliferative disease of medium-sized and large arteries characterised by lipid deposition [9]. Autopsies are useful for assessing pathological defects that are difficult to evaluate in living subjects [10]. In the present study, among the total autopsy cases, 77.5% (62) were males and 22.5% (18) were females. This was consistent with data from other similar autopsy studies conducted by Dhruva GA et al., (73.6% male and 26.4% female) and Thej MJ et al., (69% male and 31% female) [11,12]. The majority of autopsy cases were males, as the primary cause of autopsy was road traffic accidents, a trend also observed in the aforementioned studies [11,12].
The mean age of the autopsy cases in the present study was 37.6 years (95% Confidence Interval [CI]: 28.6-32.0), indicating a younger population. The majority of autopsy cases fell within the age group of 30-39 years (42.5%). Dhruva GA et al., reported the highest incidence (31.1%) among individuals aged 31-49 years [11]. Thej MJ et al., noted the highest incidence (25.7%) among those aged 20-29 years, with a mean age of 37.11 years [12]. These findings were similar to those of the present study.
The prevalence of coronary atherosclerosis is undoubtedly on the rise in India, attributed to increasing westernisation and changing lifestyles, which lead to a rise in co-morbidities. South Asians account for approximately 60% of the world’s CAD burden, particularly affecting young adults. One-third of deaths worldwide are due to CAD and atherosclerosis. India, as a developing country, is considered the CAD capital of the world [7]. The prevalence of coronary atherosclerosis in the present study was found to be 13.8%, which contrasts with findings from other studies reported by Kumar S et al., and Singh H et al., which indicated prevalence rates of 80% and 78%, respectively [13,14]. Thej MJ et al., reported a prevalence of 66% [12]. The lower prevalence observed in the present study may be attributed to the fact that present study focused only on cases involving unnatural deaths and followed the modified AHA classification for atherosclerosis.
The prevalence of asymptomatic atherosclerosis among females was 11.1%, while among males it was 14.5%. The prevalence of asymptomatic atherosclerosis increased with age, peaking in those over 60 years of age at 50%. In a study by Dhruva GA et al., the prevalence of atherosclerosis increased from the age of 20 to 60, with the highest cases occurring in the sixth decade of life [11]. Thej MJ et al., reported an increased prevalence in the older age group (35-85) compared to the younger age group (15-34). Additionally, men exhibited a slightly higher prevalence of atherosclerosis compared to females, consistent with the findings of the present study [12].
In the present study, the mean width of the intima at maximal intimal thickness in the non atherosclerosis group was 0.000213 mm2, while in the asymptomatic atherosclerosis group it was 0.000585 mm2, indicating a higher value in the asymptomatic atherosclerosis group. There was a statistically significant difference between the two groups, with a p-value of 0.005. The mean percentage of luminal narrowing in the present study for the non atherosclerosis group was 46.7%, while for the asymptomatic atherosclerosis group it was 56%, indicating increased narrowing in the asymptomatic atherosclerosis group. However, the difference between the two groups was not statistically significant. The percentage of luminal narrowing in the atherosclerotic group in the LADs, LCXs, and RCA was between 26-50%, which contrasts with the study conducted by Kumar S et al., where the majority of cases showed luminal narrowing between 50-75% [13]. In the present study, only unnatural non cardiac deaths were considered. Narrowing of the lumen is a predominant feature of Grade 5 lesions of atherosclerosis [15,16]. Jain S et al., and Khiste JA et al., reported in their studies that luminal narrowing commonly ranged from 25 to 50% in the coronary arteries [17,18]. Thiripurasundari R et al., reported that the mean luminal narrowing in females and males was 40.6% and 57.3%, respectively. The artery with the maximum narrowing sampled was the Left Anterior Descending (LAD) artery, which had a narrowing of 49.4% [19]. In the present study, among all three major vessels, the LAD showed the highest degree of atherosclerotic involvement. The LAD is the most frequently affected coronary artery in atherosclerotic lesions, likely due to the hemodynamic stress it endures.
The mean IMR in the current study for the non atherosclerosis group was 1.03, while for the asymptomatic atherosclerosis group it was 2.43, indicating a higher value in the asymptomatic atherosclerosis group. The difference between the two groups was statistically significant. In atherosclerosis, the medial thickness beneath the affected intima with the atherosclerotic plaque is typically substantially thinner [20]. Thiripurasundari R et al., reported that the mean IMR in females and males was 2.05 and 4.48, respectively [19]. Khiste JA et al., found that the severity of IMR was directly proportional to the severity of atherosclerotic grade up to Grade 5 [18].
In living subjects, the assessment of Intima-Media Thickness (IMT) is performed using B-mode ultrasonography to evaluate the degree of atherosclerosis and to determine cardiovascular risk [18]. The mean ITI in the present study for the non atherosclerosis group was 1.31, while for the asymptomatic atherosclerosis group it was 1.97, indicating a higher value in the asymptomatic atherosclerosis group. However, the difference between the two groups was not statistically significant. Thiripurasundari R et al., reported that the mean ITI in females and males was 1.07 and 1.95, respectively [19].
It has been reported that the percentage of luminal narrowing and the mean IMR show a linear increment with higher AHA grades of atherosclerosis consistently across all three vessels. Therefore, both of these morphometric parameters effectively correspond with the morphological grades of atherosclerosis. These parameters can serve as reliable indicators for evaluating the severity of atherosclerotic lesions, thereby augmenting histomorphological examinations [17].
Limitation(s)
The limitations of this study include its retrospective design and the limited number of cases captured within one year. The number of cases during this period was relatively low due to social stigma and religious views associated with autopsies in the local population. Since our hospital is situated in a rural area, many of the patients are illiterate and therefore unaware of the importance of an autopsy. As a result, a significant number of deaths go unreported. Additionally, because this was a retrospective study, details related to smoking habits, tobacco chewing, alcohol consumption, other risk factors for atherosclerosis, lifestyle, and medical history was not taken.
However, an important finding from this study was the high prevalence of cardiac diseases in asymptomatic cases, particularly among young adult males in their prime age of productivity. This demographic requires special attention to promote lifestyle changes and increase awareness and knowledge about preventive measures. The width of the intima at maximal intimal thickness and the IMR are the most reliable morphometric parameters to consider when predicting atherosclerosis. Further studies with larger sample sizes are needed to substantiate these findings and to extrapolate the results to the general population.
Conclusion(s)
Morphometric analysis of coronary arteries helps predict and estimate the degree of atherosclerosis in a non diseased population. The width of the intima at maximal intimal thickness and the IMR are the most reliable morphometric parameters for predicting atherosclerosis. The study indicates a significant risk to the community, and serious measures for prevention should be adopted. This information is useful for informing health policy and improving healthcare.
*Independent t-test